Microsoft word - macular degeneration.docx


Macular Degeneration
Age related macular degeneration (AMD) is the leading cause of legal blindness in the elderly Caucasian population, but is relatively rare in other races. The degenerative condition of the central retina (macula) only affects central vision, leaving peripheral vision intact. AMD affects approximately 30% or more of the Caucasian population age 75 and greater and, while no one knows the exact cause of this disorder, a genetic link has been made. The primary lesion appears to occur deep to the central retina with deposits known as drusen. Drusen are thought to be metabolic by-products, the increasing deposition of which may further interfere with the high metabolic activity of the macula. Risk factors for vision loss with AMD include advancing age, hyperopia (farsightedness), family history of AMD, exposure to ultraviolet (UV) light, smoking, and high blood pressure. Nutritional factors may also play a role, and will be discussed in further detail below under "Protection Against AMD". There are two basic forms of AMD: "dry" AMD and "wet" AMD. The latter of these is the more visually debilitating form. These are discussed in further detail below.
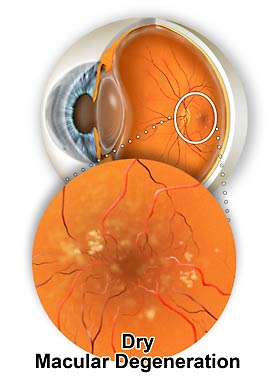
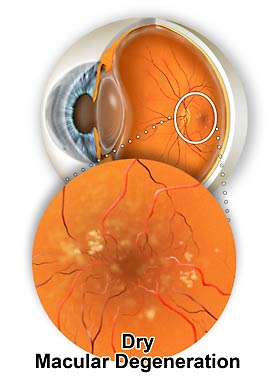
"Dry" AMD
The deposition of drusen typically begins
in the middle-aged and progressively
worsens over a period of many years,
perhaps several decades. This is
associated with increasing macular
destruction and gradual reduction in
central vision. "Dry " AMD accounts for
90% of cases and, fortunately, does not
usually cause total loss of reading vision.
Patients with this form of AMD must be
monitored quite closely, as the condition may deteriorate into "wet" AMD.
The yellowish deposits in the macula, known as drusen, are a classic sign of dry macular degeneration
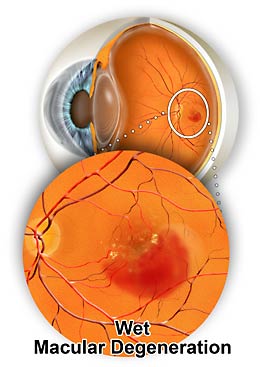
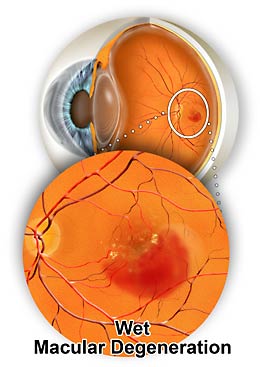
"Wet" AMD
The "wet" form of AMD accounts for only
10% of all cases, and is more visually
debilitating. This form of the disease
occurs when a tiny frond of vessels
(capillaries) breaks through a layer of the
retina known as Bruch's membrane, and grows beneath the macula. This is known as a choroidal neovascular membrane (CNVM). The abnormal vessels of the CNVM may leak fluid causing a localized swelling, or worse, result in a localized bleed. This is the condition most likely to
result in legal blindness. It is important to realize, however, that even "wet" AMD
A tiny net of abnormal blood vessels has
doesn't lead to "cane blindness," given
developed under the retina, causing
that peripheral vision remains intact
bleeding and loss of central vision
Diagnosis of ARMD
The diagnosis of "dry" AMD is made on clinical findings alone, that is, by examination of the retina using specialized equipment. When an ophthalmologist suspects "wet" AMD, a fluorescein angiogram (FA) may be completed. This study involves intravenous injection, and in some cases, oral administration, of the dye with subsequent photography of the retina. This is a extraordinarily safe procedure, which is completed in the office. The photographs are subsequently reviewed by the ophthalmologist for signs of "leaky" or bleeding vessels beneath the macula indicative of a CNVM. If a CNVM is confirmed, the patient is said to have "wet" AMD.
Evolving Treatments
While a cure for wet AMD is not yet a reality, there are now more treatment choices, and the field is changing rapidly. Recommendations made only a few years ago no longer hold today.
For example, doctors previously used a laser to treat wet AMD. Although lasers may sound high-tech, the strategy for their use was fairly simple. The doctor used the laser to burn the blood vessels in order to make them go away. Since the body actively tries to make blood vessels grow, it isn't hard to figure out the problem with lasers - even if a doctor could successfully "cook" these blood vessels, new ones often quickly regrew to take their place. Unfortunately, each laser treatment destroys retinal cells.
The next development used a drug called Visudyne® that specifically binds to blood vessels. When Visudyne® is activated with a special cold laser in a process called photodynamic therapy, the drug damages blood vessels and causes them to close down. In the process, the treatment caused inflammation but not as much damage to the retina as the hot laser. Yet again, the same difficulty exists: blood vessels regrow after treatment. While photodynamic therapy can be repeated without causing too much damage, it does have several drawbacks: it causes some damage to normal tissue, and doesn't work for many subtypes of wet AMD.
To avoid some of the problems with photodynamic therapy, doctors began to use triamcinolone - a corticosteroid injected directly into the eye. Triamcinolone reduces inflammation specifically caused by photodynamic therapy and suppresses the regrowth of vessels. In addition, triamcinolone lasts for up to six months in the eye. Patients treated with a combination of triamcinolone and photodynamic therapy appeared to have better visual outcomes with fewer treatments per year. Unfortunately, triamcinolone has many side effects, including glaucoma and cataract formation.
Anti-VEGF Treatments
The need emerged to develop a way to suppress blood vessel growth without causing so many side-effects. The answer came from cancer therapy. Tumors grow, and to grow past a certain size, they need blood vessels to feed them. Cancer research has focused a lot of attention on inhibiting this process. The most important chemical that causes blood vessel growth is a protein made by the body called Vascular Endothelial Growth Factor (VEGF). Various drugs have been developed to block the effects of VEGF so that blood vessel growth can be stopped or, at least, restrained.
Injecting VEGF blockers (anti-VEGF agents) into the eye was a huge breakthrough in treating wet AMD. The first drug used was Macugen® developed by (OSI) Eyetech, which could only block some forms of VEGF. Patients treated with Macugen® did better than those not having treatment, but they still lost vision. Later development of two closely related drugs, Avastin® and Lucentis® by Genentech, brought macular degeneration treatment to a new level.
Patients treated with Lucentis® have a small improvement, on average, in visual acuity. Until now, no other treatment had resulted in a net gain in vision. Some doctors are using Avastin® and, while the cost differs, the results to date are very similar. Both drugs are significant advances, producing much better results than no treatment or previous treatment. Lucentis® is FDA-approved for wet AMD. Avastin® is FDA-approved for colorectal cancer and is being used "off-label" to treat wet AMD. Both drugs continue to be evaluated in ongoing clinical trials.
Initial clinical studies used monthly injections of Lucentis® in patients with wet AMD with impressive results. Various strategies are being used to try to reduce the number of injections needed, as monthly treatment is a difficult regimen for patients. We don't know the right approach for everyone, but we are finding that it's possible to use less frequent dosing in many patients. About one-third of patients treated will have a significant improvement in vision, which retinal specialists define as being able to read three lines more on the eye chart than before treatment. However, many patients lose more lines than this when they initially develop the disease, so a three line improvement in a minority of patients still isn't the desired outcome.
What we would like is for a greater proportion of patients to have a greater amount of vision gained. To accomplish this, treatment trials are underway to combine other drugs or treatments with Lucentis® or Avastin® For instance, the use of Lucentis® with a drug that blocks a factor called Platelet Derived Growth Factor (PDGF) is under investigation to see if the results are better than using Lucentis® alone. Most studies of this type focus on newly diagnosed, previously untreated patients. Another goal is to reduce the number of required treatments. Some new research is investigating various strategies to reduce the treatment frequency, but the visual outcomes of these approaches are not known at present.
It's important to work with your doctor to stay informed and assess your treatment options. Early treatment is critical. Although the results of treatment are better than ever before, we continue to look for even more promising results in the future.
Source: http://www.clearsight.com.au/images/pdf/Macular%20Degeneration.pdf
PAR LYNN M VAN LITH, LE DÉSIR CROISSANT DES FEMMES MÉLANIE YAHNER ET LYNN BAKAMJIAN D'AFRIQUE SUBSAHARIENNE DE LIMITER LE NOMBRE DE GROSSESSES : RELEVER LE DÉFI Contrairement aux idées reçues, de nombreuses et les moins instruites, utilisent des méthodes femmes d'Afrique subsaharienne—souvent à de contraception temporaires moins efficaces.
The Center forHealth and Health 2121 K Street, NW, Suite 250Washington, DC 20037 Health and Health Care in Schools 202-466-3396 fax 202-466-3467 A report from the Center for Health and Health Care in Schools on the policies and financing of health programming in schools Volume 9, Number 2 In this issue: Prescription for Danger--Trends in Teen Drug Abuse