Aggression and violence: an evidence-based medicine monograph for psychosomatic medicine practice
Aggression and Violence
An Evidence-Based Medicine (EBM) Monograph for
Psychosomatic Medicine Practice
Published co-jointly by the Guideline and EBM Subcommittee of the
Academy of Psychosomatic Medicine (APM) and the European Association
of Psychosomatic Medicine (EAPM)
Authors/Workgroup:
A.F.G. Leentjens
Version.10.31.2013
Violence and Aggression –
EBM Summary
INTRODUCTION
Objective and methods:
This monograph summarizes current knowledge related to the diagnosis, epidemiology, and
management of aggression and violence in the general hospital. The monograph is modeled
after previous guidelines provided by the Evidence-Based Medicine Sub-Committee of the
Academy of Psychosomatic Medicine and the European Association of Psychosomatic
Medicine (EAPM). It is based on a systematic review of clinical trials and expert opinion. The
quality of the evidence discussed in this monograph is graded as ‘high', ‘moderate', ‘low' or ‘very low', following the Grading of Recommendations Assessment, Development and
Evaluation' (GRADE) system, which was developed by the Cochrane Collaborative
(http://www.gradeworkinggroup.org/intro.htm) Readers are encouraged to consult the
recommended readings for more detailed information (Appendix A).
Definition and symptoms:
The terms aggression and violence and the related concepts of agitation and hostility have no
universally accepted definitions. Being concerned with overt behavior that might have the
consequence of causing damage and harm, the terms describe complex behaviors that have
dimensions with biological, psychological and social determinants. The following definitions
pertaining to these overt behaviors are based on a consensus from the extant literature:
Impulsivity: A behavioral state characterized by diminished restraint to action in response to
some stimulus.
Agitation: A state of emotional arousal or motor restlessness associated with purposeless
activity.
Aggression: Physical violence toward people or objects or verbal threats and intimidation (1).
Violence: Overt physical aggression that has the potential consequence of physical harm to
another person or object.
Risk Factors:
Aggression and violence are often classified according to whether the behavior is considered
to be impulsive (associated with a high degree of affective arousal) or predatory (planned and
not associated with high levels of affect).
A variety of psychiatric diagnoses are associated with either repetitive or acutely elevated risk
for aggression and violence. When confronted with episodes of aggression or violence within
the general hospital the consultation psychiatrist may be called upon to make a specific
diagnosis as a basis for understanding and intervention.
Prevalence and incidence:
Violence is a major public health problem worldwide. Each year, millions of people die as the
result of injuries due to violence. Many more survive their injuries, but live with permanent
disabilities. Violence is a leading cause of death among people aged 15-44 years worldwide,
accounting for 14% of deaths among males and 7% of deaths in females (2). The Centers for
Disease Control (CDC) maintains a comprehensive surveillance system for monitoring violent
deaths in the US. The National Violent Death Reporting System (NVDRS) is operative in 18
states. The CDC estimated that there were18, 500 homicides in the US in 2006 (3). While
affecting individuals at each stage of life, homicide is the third leading cause of death among
those ages 15-24, after accidents and suicide (4).
Workplace violence is an occupational hazard drawing increasing attention. Healthcare
facilities are among the more frequent sites for violence. Between 1993 and 1999, there were
1.7 million episodes of workplace-related violence each year in the United States, and in 12%
of these episodes, the victim was a health care worker (4). The occurrence rate is such that
surveys in general hospitals reveal that half of surveyed employees have witnessed patient or
visitor violence within the prior year, 11% within the prior week (5).
Consultation psychiatrists may be called upon to assist with recommending methods to
predict or manage such events.
There are no available surveys of the incidence of aggression or violence among patients in
general hospitals.
Diagnosis and risk factors:
In epidemiological studies aggression is often associated with psychiatric diagnoses (6).
Longitudinal data collected during the National Epidemiologic Survey on Alcohol and
Related Conditions (NESARC) indicates that mental illness alone does not predict future
violent behavior. Future violence instead is associated with various clinical factors (substance
abuse and perceived threats), demographic factors (younger age, male sex, less than high
school education, and lower income), historical factors (past violence, juvenile detention,
physical abuse, and parental arrests), and social factors (recent divorce, unemployment,
history of victimization). The strongest predictor of future violence is the co-occurrence of
serious mental illness and substance abuse (7). Sheridan et al (8,9) describe that patient and
staff conflicts, especially those that involve enforcement of rules, denial of requests, and
involuntary admission or transfer can precipitate aggressive acts and violence.
A variety of psychiatric disorders are associated with either repetitive or acutely elevated risk
for aggression and violence, such as psychosis, mania, delirium, and some personality
disorders.
Psychotic Disorders:
Schizophrenia
There is an extensive literature documenting increased risk for violent behavior among
individuals diagnosed with schizophrenic disorder. Moderate quality evidence from
epidemiological studies links violent episodes with the presence of some positive psychotic
symptoms. There is low quality evidence suggesting that some symptoms, such as persecutory
delusions (10) and command hallucinations (11) increase risk of violence. The presence of
negative symptoms may decrease risk of violence (12). There is moderate quality evidence
that the majority of risk for serious violence in this group is due to the frequent co-occurrence
of substance use disorders (13). Patients with high levels of hostility and low levels of insight
are at greater risk for violent offending (14, 15).
Bipolar Disorder: There is low quality evidence that the presence of bipolar disorder is a predisposing factor to
violence (with odds ratios reported between 2.0 to 9.0). While severity of illness or symptom
profile does not predict aggressive and violent behavior the largest amount of variance is due
to presence of co-occurring substance use disorder (16, 17).
Personality Disorders:
Antisocial personality disorder
There is high quality evidence for linking violent episodes to disorders associated with a lack
of empathy or concern for others. Individuals with these characteristics are overrepresented in
cases of purposeful and directed violence (18, 19).
Borderline personality disorder
The diagnostic criteria for Borderline Personality include the presence of impulsivity,
affective instability, inappropriate anger or deficits in emotional regulation. Paranoid ideation
and brief psychotic episodes have been described in this group of patients (20). There is
moderate quality evidence that a diagnosis of BPD is a risk factor for elevated risk for
violence in clinical and forensic populations. The evidence for violent predisposition in
community samples is low (21).
Impulse Control Disorders:
Intermittent Explosive Disorder (IED): IED is an impulse control disorder characterized by
repeated episodes of serious assaultive or destructive acts out of proportion to precipitating
stressors. Since DSM-IV TR includes an exclusion criterion for the co-occurrence of another
disorder that would better account for this symptom picture, some have argued that this has
led to under-diagnosis of this condition because of frequent co-occurrence of personality
disorder (22). The DSM-5 criteria for IED does not include such exclusionary criteria.
Epidemiological studies suggest that this condition appears early in life (age 14-20) and is
underrepresented in treatment samples. Estimates of lifetime prevalence are 5-7% in
community samples. (22). There is no equivalent diagnosis present in ICD-10.
Substance Use Disorders:
Aggression and violence are frequently associated with patients who have alcohol and drug
use disorders. There is moderate evidence that violent behavior attributed to serious mental
illness is accounted for by the coincident presence of substance use.
Alcohol
There is high quality evidence supporting an association between alcohol use and violent
injuries reported in many countries (23). There is moderate quality evidence linking the onset
of aggressive and violent behavior to the amount of drinking preceding such events and blood
alcohol levels at the time of presentation. There is high quality evidence for the relationship
between alcohol use disorders and admission to general hospitals for multiple causes (24).
Alcohol use has been long recognized to play a role in criminal violence (25).
Stimulants
Use of stimulant drugs, including cocaine, is associated with a propensity for irritability,
hostility and aggression, resulting in high rates of interpersonal violence, emergency
department and trauma center visits, assault, weapons charges and increased public health and
safety burdens. (26,27). Up to a third of such users presenting to emergency departments
require sedation for agitation and aggression. High rates of aggressive behavior have been
reported in community samples of amphetamine users. (28).
CNS Depressants
There is moderate quality evidence that aggressive behavior may follow the use of
benzodiazepine drugs in persons with impulse control or personality disorders (29).
Anabolic Steroids
There is low quality evidence for development of irritability, aggression and violent behavior
in individuals using anabolic steroids to enhance athletic performance or in body-building
(30,31).
Developmentally Disabled - There is moderate quality evidence demonstrating increased
prevalence of significant aggressive and challenging behavior in persons with developmental
disability. Over half of this population engages in some form of aggression. Only a small
number is responsible for frequent or severe acts (32). There is moderate quality evidence
suggesting that half of patients are involved in overt aggressive acts. Such behavior is often
directed at healthcare personnel and may lead to considerable caretaker burden in all settings
(33).
Delirium: There is high quality evidence that the presence of the attention deficits, paranoia,
illusions and hallucinations can result in reactive aggression in patients with hyperactive
delirium. (34).
Dementia (Neurocognitive Disorders –
moderate and severe): There is high quality
evidence that psychotic symptoms such as hallucinations and delusions are common among
those suffering with dementing illnesses with rates of 30 to 50% in those with Alzheimer's
and other dementias (35). Aggressive behaviors are frequent symptoms among patients with
dementia. Symptoms such as hitting, kicking, biting, pushing are very commonly associated
with cognitive decline and occur more frequently (70-100%). These symptoms are
particularly common in patients with moderate to severe neurocognitive disorders in inpatient
settings. Aggressive symptoms are the cause of considerable caregiver burden and risk of
injury to patients and staff (36).
Brain Disorders: Moderate evidence suggests that lesions that affect frontal lobe function
including tumors, vascular disorders or traumatic injuries are associated with disinhibition
resulting in aggression and violence (37).
Traumatic Brain Injury: While there is moderate quality evidence for agitation and
aggression in the acute phase of traumatic brain injury (10-34%), it is predominantly verbal,
characterized by anger and threats of violence rather than physical aggression. Violent acting-
out is not common. Significant correlates for violence include impaired psychosocial
functioning and new-onset major depression (38). In case studies, lesions of the hypothalamus
and amygdala have been associated with rage attacks (39,40).
Epilepsy: While agitated and aggressive behavior has been observed among patients with
seizure disorder there is low quality of evidence supporting an association between idiopathic
epilepsy and elevated levels of aggression or violent behavior (41).
TREATMENT
Acute agitation and violence when diagnosis is unclear
Intervention in situations involving aggression and violence begins with an understanding of
the nature of any provocation and a diagnostic assessment of factors that might lead to altered
arousal or impaired impulse control. A detailed assessment of provocative factors that
produce frustration or anger can often suggest methods of intervention. Evidence for
effectiveness in reducing aggression and violence in the acute care setting has been limited by
the obvious difficulty in obtaining informed consent to participate in such studies.
Non-pharmacological treatment
Recommendations provided here are based on expert consensus in the management of acute
agitation (42).
De-escalation of agitated patients – Clinicians who have worked with patients who present with agitation to emergency departments have developed the following principles published as guidelines for management of patients recognized at risk for aggressive or violent acting out.
• Ensure the safety of patients, staff and others in the area.
• Assist the patient in managing emotional arousal and distress while helping to regain
control of behavior.
• Avoid use of coercion or restraint that tend to escalate agitation.
If such approaches fail to reduce agitation and threat then the following are suggested:
• Offer of pharmacologic assistance • Offer of a "quiet room" if available • Show of force (show of concern)
Coercive interventions – There is moderate quality evidence that application of the above methods can result in dramatic reductions in the use of seclusion and restraints within inpatient hospital settings. If trial of these methods fails to result in return of behavioral control coercive methods such as seclusion and restraint may become necessary to prevent harm to patients, staff and others. There is no evidence to support any coercive intervention having advantage over any other.
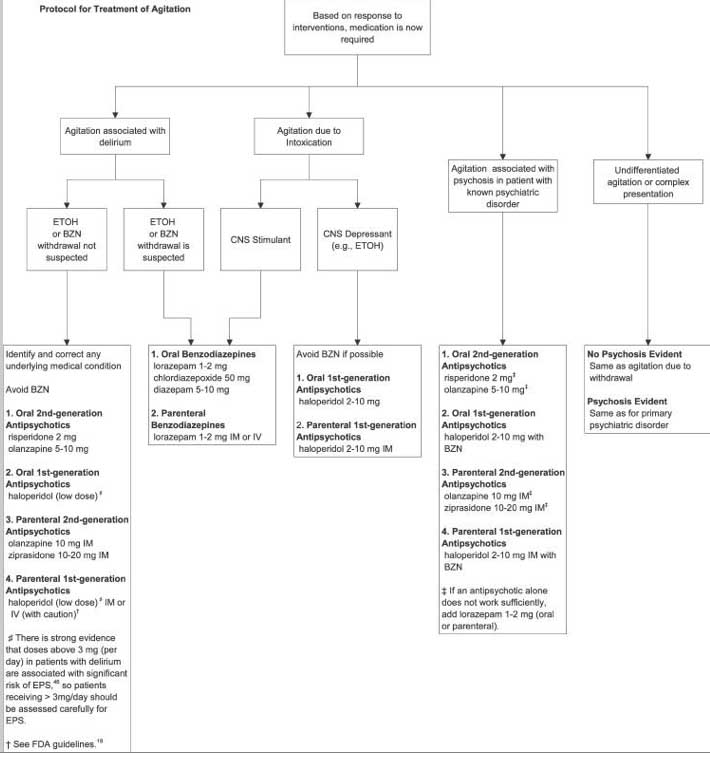
Pharmacological symptomatic treatment: The aim of pharmacologic treatment is to calm a patient to allow complete evaluation of the
causes of a behavioral disturbance. Efficacy for use of agents to achieve "rapid
tranquilization" is supported by low quality evidence. This should be undertaken only after
consideration of risks of such intervention balanced against risk of harm to patients and others in attendance (43). Three categories of drugs have been customarily used and studied for control of agitation and aggression in these circumstances. First-Generation Antipsychotics Haloperidol is a highly potent antagonist of the D2 receptor approved in oral and intramuscular forms for treatment of schizophrenia. Haloperidol has a long record of efficacy and safety, though the quality of evidence for its use in treating acute agitation or aggression is low (44,45,46). The FDA has issued a safety alert highlighting the risk of prolonged QTc interval associated with the aggressive use of haloperidol in parenteral formulations. There have been case reports of development of Torsade de Pointes, some with cardiac arrest. While these cases have generally involved intravenous use clinicians should be aware of the risk of potentially fatal arrhythmias when parenteral haloperidol is used. Cardiac monitoring and assessment of electrolyte status may reduce risk. Haloperidol should be used with greater caution in patients with QTc greater than 450 milliseconds (47). Second generation antipsychotics Moderate quality evidence supports the view that efficacy of the second generation antipsychotics is equal to Haloperidol in the treatment of acute agitation (48). Antipsychotic agents should be used with caution in situations where a psychotic diagnosis has not been established. Benzodiazepines There is moderate quality evidence that benzodiazepines such as diazepam, lorazepam and clonazepam are effective in calming the agitated patient. Risks include central nervous system depression. These drugs are often used together with the first or second-generation antipsychotics though the quality of evidence for enhanced efficacy in combination is low (49, 50) Agitation and violence where a psychotic diagnosis (schizophrenia, mania) has been established When patients present with acute agitation or threatening or violent behavior when a diagnosis of psychotic illness has been established the goal of treatment is twofold. These include the calming of the patient to allow complete evaluation of the causative factors and amelioration of the underlying psychotic process. When severe agitation, threatening or menacing behaviors occur in patients known to have a diagnosis of schizophrenia or mania initial pharmacological interventions should include antipsychotic agents. There is no evidence that first generation antipsychotics are any less effective than second generation agents in managing agitated behaviors. Increasingly second- generation agents such as ziprasidone or olanzapine are being utilized in this context (51)
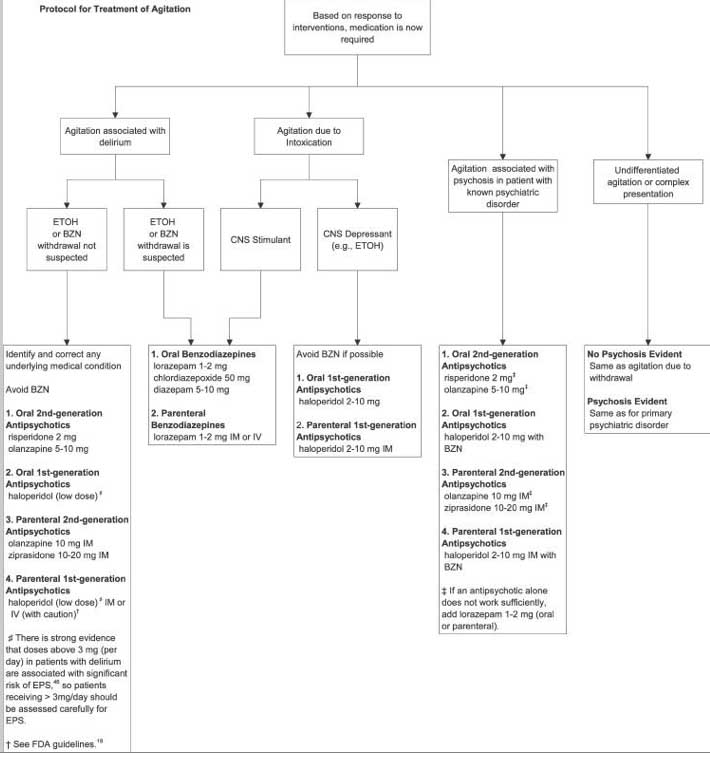
Figure 1 Protocol for Treatment of Agitation – Reproduced with permission
Agitation and violence where a psychotic diagnosis (schizophrenia, mania) has
been established
Prevention and Extended Treatment
Psychotic Disorders – Schizophrenia
Antipsychotics are the mainstay of treatment for schizophrenia. High quality evidence
supports offering clozapine to patients with schizophrenia who present with persistent
symptoms of hostility and/or display persistent violent behaviors. Clozapine has anti-
aggressive properties that go beyond its efficacy for psychotic symptoms. In the Clinical
Antipsychotic Trials of Intervention Effectiveness (CATIE) cohort, second generation
antipsychotics (not including clozapine) were not superior to perphenazine with regards to
reducing violence over 6 months (52). In the European First Episode Schizophrenia Trial
(EUFEST), olanzapine was superior in reducing hostility in early course schizophrenia
compared to haloperidol, quetiapine, or amisulpride (53)
Bipolar Disorder
There is low quality evidence in support of use of quetiapine to control agitated and
aggressive behavior in bipolar manic and mixed states (54).
Personality Disorders
There is low quality evidence suggesting a role for atypical antipsychotics and mood-
stabilizing agents in patients with borderline personality disorder who demonstrate repeated
aggressive or violent behavior (55).
Intellectually Disabled
Evidence is lacking for the effectiveness of antipsychotic medication in reducing repetitive
aggression and challenging behavior in those with intellectual impairment despite their
common use. (56). A small series utilizing placebo lead-in provides low quality evidence that
buspirone may reduce aggressive behavior in this population (57).
Intermittent Explosive Disorder
There is modest evidence for reduction in impulsive aggressive episodes following use of
fluoxetine 20-60 mg per day (58).
Low quality evidence exists from multiple studies for improvement in impulsive aggression
with use of several anti-epileptic agents. There is evidence for significant reductions in both
frequency and severity of aggression for those taking phenytoin, lithium and carbamazepine
and oxcarbazepine, but not valproate or levetiracetam. (59).
Substance Use Disorder
Identification of the presence of substance use disorders can result in referral to specialty care
for definitive treatment.
Delirium
Recommendations for treatment of aggressive behavior due to delirium can be found in the
EBM Monograph, Delirium (60). The effective treatment of delirium requires identification
and management of the medical or toxic factors causing or maintaining the condition. There is
expert consensus that orientation strategies are helpful in management of delirium. There is
low to moderate quality evidence that antipsychotic agents are effective in the treatment of
symptoms of delirium.
Dementia (Neurocognitive Disorders – moderate and severe)
Neuropsychiatric symptoms are commonly associated with Alzheimer's and other forms of dementia. Evaluation of such complaints requires consideration of precipitants, evaluation of potential painful conditions and the identification of superimposed delirium. Treatment of these conditions can reduce the severity of behavioral symptoms that are challenging. Behavioral interventions should be attempted before pharmacological treatment is considered. There are no FDA approved agents for treatment of agitation, aggression or violence in patients with dementia. While moderate quality evidence exists for modest effects of some antipsychotic agents in controlling agitation and aggression in patients with dementia there is high quality evidence for risks of use of these drugs (61,62). While there is moderate quality
evidence for modest effects in improvement of agitation and aggression with risperidone,
olanzapine and quetiapine for periods of 6 weeks to 3 months there is moderate quality
evidence that advantages can be offset by cognitive decline and increased morbidity
associated with use of these drugs (63).
All antipsychotics carry a black box warning that elderly patients with dementia-related
psychosis treated with antipsychotic drugs are at increased risk of death. Most deaths
occurring in this setting are from cardiovascular, cerebrovascular or infectious causes (64).
Despite the risks associated with use of antipsychotics in this population these drugs are the
only agents with evidence of effectiveness in psychotic symptoms associated with
Alzheimer's dementia. US Federal regulations for nursing homes recommend a trial of
discontinuation of antipsychotic drugs after three to six months. There is very limited
evidence from clinical trials to support this suggestion. One study of a group of patients for
whom this advice was followed point to a high risk of relapse in the months after stoppage in
patients for whom discontinuation has been pursued (65).
There is low quality evidence for a modest effect in randomized control trials that memantine
reduced incidence and severity of agitation in moderate to severe dementia (66).
Recommendation: In patients with dementia who display symptoms of severe agitation,
threatening or overtly violent behavior care should be taken to establish the existence of co-
existing delirium or disorders that may be producing pain. Use of antipsychotics to reduce the
severity of agitation or violence should be confined to periods of up to six weeks. Regular
weekly re-evaluation directed at measurement of efficacy and evaluation of side-reactions
including metabolic and cardiovascular effects should be part of antipsychotic management
with such patients. The majority of patients with moderate or severe neurocognitive disorders
lack capacity to provide informed consent. Risks and benefits of pharmacological
interventions should be explained to alternate decision makers and consent for specific
interventions should be obtained and documented.
Traumatic Brain Injury
There is low quality evidence that use of antipsychotics after brain injury results in declines in
cognitive function and slowing of rehabilitation (67,68). Low quality evidence exists for the
use of quetiapine for control of agitation that threatens progress in rehabilitation (69).
Evidence that carbamazepine or valproate is effective in the management of agitation and/or
aggression following brain injury is lacking.
Evidence to support pharmacological intervention to prevent or treat aggressive behavior
consequent to traumatic brain injury is lacking. Moderate quality evidence supports
aggressive treatment of depressive symptoms using SSRIs (70).
Over thirty studies provide moderate support for the efficacy of propranolol in reducing
repetitive violent behavior in patients with a variety of chronic mental illnesses,
developmental disability and organic brain disorders such as traumatic brain disorder (71).
TABLE I – Medications used for treatment of agitation (off label) with FDA approved
indications
FDA Indication
Haloperidol
Hyperactive behavior
0.5 – 2 mg qAM, qHS
(po, syrup, im, iv)
Problematic behavior in children Schizophrenia
12.5-50mg bid/tid
Behavioral syndrome
(po, syrup, im, iv, supp)
Hyperactivity Schizophrenia
2.5 mg qHS (max 30 -
Agitation in Bipolar disorder
Olanzapine
40 mg/day)
Agitation in Schizophrenia
(po, wafer, IM
Ziprasidone
10mg im q2hr, max
Agitation in Schizophrenia
40mg/day
Irritability associated with
Risperidone
0.5 – 2 mg q12hrs
autistic disorder
(po, syrup, tab)
Behavioral Syndrome (MR)
Psychomotor agitation in autistic
(Po, syrup, IM)
2mg po, 9.5mg im
dsd/bipolar dsd/Schizophrenia
Loxapine Inhaler 10mg inh/24 hours
Agitation with bipolar I disorder
QUALITY INDICATORS
Organization of detection and management:
The available evidence does not allow for a recommendation of a specific model of
intervention for violent and aggressive behavior.
Specific quality indicators
The following indicators provide insight into the quality of the organizational response to
potential violent acts.
The presence of an institutional protocol for response to violent and aggressive behaviors.
Presence of documentation justifying use of antipsychotics in treatment of aggression and
violence in patients without a psychotic diagnosis.
References:
1
Coccaro EF, Berman ME, Kavoussi RJ. Assessment of life history of aggression:
development and psychometric characteristics. Psychiatric Research. 1997;73(3):147- 157. 2
Krug EG, Dahlberg LL, Mercy JA et al. World report on violence and health.
World Health Organization. Geneva. 2002. 3
US Center for Disease Control.
4. Hoyert DL, Xu J. Deaths, Preliminary Data for 2011. National Vital Statistics Report. Centers for Disease Control. 2012;61(6):1-52. 5. Kansagra SM, Rao SR, Sullivan AF et al. A Survey of workplace violence Across 65 US emergency departments. Academic Emergency Medicine. 2008. 15(12):1268 -72. 6. Hahn S, Hantikainen V, Needham I et al. Patient and visitor violence in the general hospital, occurrence, staff interventions and consequences. Journal of Advanced Nursing 2012;68(12):2685-99. accessed 5-28-2012. 7.
Swanson JW, Holtzer CE, Ganju VK et al. Violence and psychiatric disorder in the
community: Evidence from the Epidemiological Catchment Area surveys. Hospital and Community Psychiatry. 1990 41:761-770. 8.
Elbogen EB, Johnson SC. The intricate link between violence and related
conditions. Archives of General Psychiatry.2009. 66(2):152-160. 9. Sheridan M, Henrion R, Robinson L et al. Precipitants of violence in a psychiatric inpatient setting. Hospital and Community Psychiatry 1990;41(7):776-80. 10. Barlow K, Grenyer B, Ilkiw-Lavalle. Prevalence and precipitants of aggression in psychiatric inpatient units. Australian and New Zealand Journal of Psychiatry. 2000;34(6):967-974. 11.
Junginger J, McGuire L. Psychotic motivation and the paradox of current research
on serious mental illness and rates of violence. Schizophrenia Bulletin 2004;30(1):21-30. 12. McNiel DE, Eisner JP, Binder RL. The Relationship Between command hallucinations and violence. Psychiatric Services. 2000;51:1288-1292. 13.
Swanson JW, Swartz MS, Van Dorn RA et al. A national study of violent behavior
in persons with schizophrenia. Archives of General Psychiatry. 2006. 63:490-499. 14.
Fazel S, Gulati G, Linsell L et al. Schizophrenia and violence: systematic review and
meta-analysis. PLoS Medicine. 2009. 6(8): journal.pmed.1000120 15. Soyka M, Graz C, Bottlender R. et al. Clinical correlates of later violence and criminal offenses in schizophrenia. Schizophrenia Research. 2007.94:89-98. 16. Ballister J, Goldstein T, Obreja M et al. Is bipolar disorder specifically associated with aggression? Bipolar Disorder 2012;14(3):283-90. 17. Fazel S, Lichtenstein P, Grann M. Bipolar disorder and violent Crime. Archives of General Psychiatry. 2010. 67(9):932-938. 18. Reid WH, Thorne SA. Personality disorders and violent potential. Journal of Psychiatric Practice. 2007.;13(4):261-268. 19.
Fountoulakis KN, Leucht S, Kaprinis GS. Personality disorders and violence.
Current Opinion in Psychiatry. 2008;21:84-92. 20.
Diagnostic and Statistical Manual, Fourth Edition, Text Revision.
(DSM-IVTR).American Psychiatric Association. Arlington, Va. 2000. 21. Allen A, Links PS. Aggression in borderline personality disorder: Evidence for Increased Risk and Clinical Predictors. Current Psychiatry Reports. 2012. 22.
Coccaro EF. Intermittent Explosive Disorder: development of integrated research
criteria for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Comprehensive Psychiatry.2011;52:119-125. 23.
Kessler RC, Caccaro EF, Fava M. The Prevalence and correlates of DSM-IV,
intermittent explosive disorder in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2006;63(6):669-678. 24.
Cherpitel CJ. Alcohol and injuries: a review of international emergency room
studies since 1995. Drug and Alcohol Review. 2007. 26:201-214. 25. Roche AM, Freeman T, Skinner N. From data to evidence, to action: Findings from a systematic review of hospital screening studies for high-risk alcohol consumption. Drug and Alcohol Dependence. 2006;83:1-14. 26.
Roizen, J. Epidemiological issues in alcohol-related violence. In: Galanter, M.,
ed. Recent Developments in Alcoholism.1997; Vol. 13. New York: Plenum Press7-40.
Hoaken PN, Stewart SH. Drugs of abuse and the elicitation of human aggressive
behavior. Addictive Behaviors. 2003;28:1533-1554. 28.
Dawe S, Davis P, Lapworth et al. Mechanisms underlying aggressive and
hostile behaviour in amphetamine users. Current Opinion in Psychiatry. 2009; 22:268-273. 29. Payer DE, Lieberman MD, London ED. Neural correlates of affect processing and aggression in methamphetamine dependence. Archives of General Psychiatry. 2011;68(3):271-282. 30. Rouve N, Bagheri H, Telmon N et al. Prescribed drugs and violence: a case/non-case study in the French PharmacoVigilance Database. European Journal of Pharmacology. 2011;67:1189-1198. 31. Kanayama G, Hudson JI, Pope HG. Long term psychiatric and medical consequences of anabolic-androgenic steroid abuse. Drug and Alcohol Dependence 2008;98(12):1-12. 32. Trenton AJ, Currier GW. Behavioral manifestations of anabolic steroid use. CNS Drugs.2005;19(7):571-595. 33. Benson BA, Brooks WT. Aggressive challenging behavior and intellectual disability. Current Opinion in Psychiatry 2008;21:454-458. 34. Brylewski J, Duggan L. Antipsychotic medication for challenging behavior in people with learning disabilities (Review). Cochrane Database of Systematic Reviews. 2004 Issue 3:1-32. 35. Onyike, C, Lyketsos CG. Aggression and Violence. Textbook of Psychosomatic Medicine. American Psychiatric Publishing Inc. Washington/London. 2010. 36. Susan A, Ropacki, Dilip V. Jeste. Epidemiology of and risk factors for psychosis of
Alzheimer's Disease: A Review of 55 studies published from 1990 to 2003. American Journal of Psychiatry 2005;162:2022-2030. 37. Somaia M, Rosenheck R, Lyketsos, CG. Effect of second generation antipsychotics
on caregiver burden in Alzheimer's Disease. Journal of Clinical Psychiatry. 2012;73(1):121-128. 38. Brower MC, Price BH. Neuropsychiatry of frontal lobe dysfunction in violent and criminal behavior. Journal of Neurology, Neurosurgery and Psychiatry. 2001;71:720- 726. 39. Rao V, Rosenburg P, Bertrand M et al. Aggression after traumatic brain injury:
Prevalence and Correlates. Journal of Neuropsychiatry and Clinical Neuroscience. 2009;21(4):420-429.
40. Demarree HA, Harrison DW. Case study: topographical brain mapping in hostility following mild closed head injury. International Journal of Neuroscience. 1996;87 (1-2):97-101. 41. Tonkonogy JM, Geller JL. Hypothalamic lesions and intermittent explosive disorder. Journal of Neuropsychiatry and Clinical Neuroscience. 1992;4(1);45-50. 42. Delgado-Escueta AV, Mattson RH, King L et al. The nature of aggression during epileptic seizures. New England Journal of Medicine. 1981;305:711-716. 43. Knox DK, Holloman GH. Use and avoidance of seclusion and restraint: consensus
statement of the American Association of Emergency Psychiatry, "Project BETA". Seclusion and Restraint Work Group. Western Journal of Emergency Medicine. 2012;13(1):35-40. 44. Ferrier N, Piling S, Bazire S. Bipolar Disorder, the management of bipolar disorder in adults, children and adolescents in primary care. National Clinical Practice Guideline number accessed 5-28-2012. 45. Lehman AF, Liebermen JA, Dixon LB et al. Practice guideline for the treatment of Patients with Schizophrenia, 2nd edition. American Journal of Psychiatry.2004;161(2):1-56. 46. MacDonnald K, Wilson MP, Minassian A et al. A retrospective analysis of intramuscular haloperidol and olanzapine in the treatment of agitation in drug and alcohol using patients. General Hospital Psychiatry 2010;32:443-445. 47. Huf G, Alexander J,Allan MH et al. Haldol plus promethazine for psychosis-induced aggression. Cochrane Database of Systematic Reviews. 2011,11. 48. Hassaballa HA, Balk RA. Torsade de Pointes associated with the administration of intravenous Haldol. American Journal of Therapeutics. 2003;10(1):58-60. 49. Citrome L. Comparison of intramuscular ziprasidone, olanzapine or aripiperazole: a quantitative review of efficacy and safety. Journal of Clinical Psychiatry. 2007;68:1876-1885. 50. Marder SR. A review of agitation in mental illness: treatment guidelines and current therapies. Journal of Clinical Psychiatry. 2006;(suppl 10):13-21. 50. Battaglia J, Rush J et al. Haloperidol, lorazepam, or both for psychotic agitation: a multicenter, prospective, double-blind, emergency department study. 1997;15:335-340. 51. Schatzberg AF, Cole JO, DeBattista C. Manual of Clinical Pharmacology 7th ed. Washington, DC American Psychiatric Publishings, Inc. 2010 52. Swanson JW, Schwartz MS, Van Dorn RA. Comparison of antipsychotic medication effects in reducing violence in people with schizophrenia. British Journal of Psychiatry. 2008;193(1):37-43. 53. Volavka J, Czobor P, Derks EM. Efficacy of antipsychotic drugs against hostility in the European First-Episode Schizophrenia Trial (EUFEST). Journal of Clinical Psychiatry. 2011;72(7);955-61. 54. Buckley PF, Paulsson B, Brecher M. Treatment of agitation and aggression in bipolar mania: efficacy of quitiapine. Journal of Affective Disorders.2007;100:S33-43. 55. Latalova K, Prasco J. Aggression in borderline personality disorder. Psychiatric Quarterly. 2010;81:239-251. 56. Tsiouris JA. Pharmacotherapy for aggressive behavior in persons with intellectual disabilities: treatment or mistreatment? Journal of Intellectual Disabilty Research. 2010;54(1):1-16. 57. Ratey J, Sovner R, Parks A et al. Buspirone treatment of aggression and anxiety in
mentally retarded patients. Journal of Clinical Psychiatry. 1991;52(4) :159-62. 58. Coccaro, EF, Lee RJ, Kavoussi RJ. A Double blind, placebo controlled trial of Fluoxetine in patients with intermittent explosive disorder. Journal of Clinical Psychiatry. 2009;70(5):653-662. 59. Jones RM, Arlidge J, Gillham R et al. Efficacy of mood stabilizers in the treatment of impulsive or repetitive aggression: a systematic review and meta-analysis. British Journal of Psychiatry. 2011;198;93-98. 60. Leentjens A.F.G., Rundell J, Rummans T et al. Delirium: An evidence-based monograph for psychosomatic medicine practice. Published jointly by Academy of Psychosomatic Medicine and European Association for Psychosomatic Medicine. 2012; Journal of Psychosomatic Research 2012;73(2):49-51. 61. Sink KM, Holden KF, Yaffe K. Phamacological treatment of neuropsychiatric symptoms of dementia - A review of the evidence. Journal of American Medical Association. 2005. 293(5): 596-608. 62. Scneider L, Tariot PN, Dagerman KS et al. Effectiveness of atypical antipsychotic
drugs in patients with Alzheimer's Disease. New England Journal of Medicine. 2006;355(15):1525-1538. 63. Sultzer DL, Davis SM, Tariot PN et al. Clinical symptom responses to atypical
antipsychotic medications in Alzheimer's Disease Phase 1 Outcomes from the CATIE- AD Effectiveness Trial. American Journal of Psychiatry. 2008;165(7):1-21. 64. Huybrechts KF, Gerhard T, Crystal S et al. Differential risk of death in older residents in nursing homes prescribed specific antipsychotic drugs: population-based cohort study. British Journal of Medicine. 2012;344:e977. 65. Devanand DP, Mintzer MD, Schultz SK et al. Relapse risk after discontinuation of
risperidone in Alzheimer's Disease. New England Journal of Medicine. 2012;367(16):
1497-1506.
66. Herrman N, Li A, Lanctot K. Mementine in Dementia: a review of the current evidence.
Expert Opinion, Pharamcotherapeutics. 2011;12(5):787-800.
67. Levy M, Berson A, Cook T. Treatment of agitation following traumatic brain injury: A
review of the literature. Neurorehabilitation. 2005;20:279-306.
68. Fleminger S, Greenwood RRJ, Oliver DL. Pharmacological management for agitation
and Aggression in People with acquired brain injury. Cochrane Database of Systematic
Reviews. 2008. 4:1-25.
69. Kim E, Bijlani M. A pilot study of quetiapine treatment of aggression due to traumatic
brain injury. Journal of Neuropsychiatry and Clinical Neuroscience. 2007.18(4):547-549.
70. Chew E, Zafonte RD. Pharmacological management of neurobehavioral disorders
following traumatic brain injury - a state of the art review. Journal of Rehabilitation
Research and Development. 2009. 46(6):851-878.
71. Silver, JM, Yudofsky SC, Slater JA et al. Propranolol treatment of chronically
hospitalized aggressive patients. Journal of Neuropsychiatry and Clinical Neuroscience.
1999;11(3):328-335.
Appendix (Additional Materials)
A)
Recommended Readings
Annotated List of Randomized Clinical Trials
Assessment and Scales
Areas for Future Research
APPENDIX A
Recommended Readings
Relevant literature:
Abraham F.P. Calabrese J.R. Evidenced-based pharmacological treatment of borderline
personality disorder: a shift from SSRIs to anticonvulsants and atypical antipsychotics.
Journal of Affective Disorders. 2008;111(1):21-30.
Buchanan R.W., Kreyenbuhl J, Kelly D. R. et al. The 2009 Schizophrenia PORT
Psychopharmacological Treatment Recommendations and Treatment Summary.
Schizophrenia Bulletin. 2010;36(1):71-93.
Lieb K, Vollm B, Rucker G. Pharmacotherapy of borderline personality disorder: Cochrane
systemic review of randomized control trials. British Journal of Psychiatry. 2010;196:4-12.
Maytal G., Sanders K.M. Aggressive and Impulsive Patients in Handbook of General Hospital
Psychiatry. 6th ed. Saunders Elsevier. Philadelphia. 2010
Monahan J., Steadman H.J., Silver E et al. Rethinking risk assessment: The MacArthur Study
of mental disorder and violence. Oxford University Press. New York. 2001.
Onyike, C, Lyketsos CG. Aggression and Violence. Textbook of Psychosomatic
Medicine. American Psychiatric Publishing Inc. Washington/London. 2010.
Scott C.L, Quanbeck C.D., Resnick P.J. Assessment of Dangerousness in American
Psychiatric Publishing Textbook of Psychiatry, 5th edition. APPI. Washington, DC. 2008.
Simon RI, Tardiff, K ed. Textbook of Violence Assessment and Management American
Psychiatric Press Inc. Washington, DC.2008.
Wilson M.P., Pepper D, Currier G.W. et al. The Psychopharmacology of agitation: consensus
statement of the American Association for Emergency Psychiatry Project BETA
Psychopharmacology Workgroup. Western Journal of Emergency Medicine. 2012;13(1):26-
34.
Relevant websites
http//www.cdc.gov/ViolencePrevention/data_stats/index.htm
APPENDIX B
Annotated List of Randomized Pharmacological Trials
Schizophrenia and Bipolar Disorder
Krakowsli M.I., Czobor P., Citrome L. et al. Archives of General Psychiatry. 2006;63(6):622-
629. Randomized, double-blind, parallel-group, 12-week trial. Physically assaultive subjects
with schizophrenia or schizoaffective disorder who were inpatients in state psychiatric
facilities were randomly assigned to treatment with clozapine (n = 37), olanzapine (n = 37),
or haloperidol (n = 36). Outcome measures were number and severity of physical assaults as
measured by the Modified Overt Aggression Scale (MOAS) physical aggression score and the
number and severity of all aggressive events as measured by the MOAS overall score. Psychiatric symptoms were assessed through the Positive and Negative Syndrome Scale (PANSS). Clozapine was superior to both olanzapine and haloperidol in reducing the number and severity of physical assaults as assessed by the Modified Overt Aggression Scale (MOAS). Olanzapine was superior to haloperidol on similar outcomes. There were no significant differences among the 3 medication groups in improvement of psychiatric symptoms as measured by the PANSS total score and PANSS subscales.
The authors concluded that clozapine shows greater efficacy than olanzapine and olanzapine greater efficacy than haloperidol in reducing aggressive behavior. This anti-aggressive effect appears to be separate from the antipsychotic and sedative action of these medications. Breier A., Meehan K., Birkitt M. et al. A double-blind, placebo-controlled dose-response comparison of intramuscular olanzapine and haloperidol in the treatment of acute agitation in schizophrenia. Archives of General Psychiatry. 2002;59(5):441-48. This study was sponsored by a pharmaceutical company and included recently hospitalized acutely agitated patients with schizophrenia (N = 270) randomized to receive 1 to 3 IM injections of olanzapine (2.5, 5.0, 7.5, or 10.0 mg), haloperidol (7.5 mg), or placebo within 24 hours. A dose-response relationship for IM olanzapine in the reduction of agitation was assessed by measuring the reduction in Positive and Negative Syndrome Scale Excited Component scores 2 hours after the first injection. Safety was assessed by recording adverse events and with extrapyramidal symptom scales and electrocardiograms at 24 hours after the first injection.
Olanzapine exhibited a dose-response relationship for reduction in agitation. Mean PANSS-EC reductions 2 hours after the first injection of olanzapine were superior to those with placebo but not with haloperidol. A dose of 5.0, 7.5, or 10.0 mg of olanzapine caused a greater reduction in agitation than placebo 30 minutes after the first injection. There were no differences between treatment groups for hypotension, the most frequently reported adverse event. There was also no difference in clinically relevant changes in the QTc interval. There was a greater incidence of treatment-emergent parkinsonism during treatment with IM haloperidol (16.7%) than with IM olanzapine (0%) or with placebo (0%).
The authors concluded that intramuscular olanzapine at a dose of 2.5 to 10.0 mg per injection exhibits a dose-response relationship in the rapid treatment of acute agitation in patients with schizophrenia and demonstrates a favorable safety profile.
Dementia
Devanand DP, Mintzer MD, Schultz SK et al. Relapse Risk after Discontinuation of
Risperidone in Alzheimer's Disease. New England Journal of Medicine. 2012;367(16):
1497-1506. 180 patients with psychosis or agitation with Alzheimer's Disease who received open-label of risperidone (average dose 0.97mg per day) for 16 weeks. Those who had a response were randomly assigned to three groups: continued risperdone therapy for 32 weeks, risperdone for 16 weeks followed by placebo for 16 weeks or placebo for sixteen weeks. Rates of adverse events and deaths did not differ significantly. However, relapse in the group who had discontinued active treatment relapsed at higher rates (hazard ratio 4.88).
Sultzer D.L, Davis S.M. Tariot P.N. et al. Clinical Symptom Response to Atypical Antipsychotics: Phase I Outcomes from the CATIE-AD Effectiveness Trial. American Journal of Psychiatry. 2008:165(7):844-854. The CATIE-AD effectiveness study included 421 outpatients with Alzheimer's Disease and psychosis or agitation. Assigned randomly to masked flexible-dose treatment with olanzapine, quetiapine, risperidone, or placebo for up to 36 weeks, patients could be re- randomized to a different medication treatment at the clinician's discretion This ended the Phase 1 period. Psychiatric and behavioral symptoms, functional abilities, cognition, care needs, and quality of life were measured at regular intervals.
There was greater improvement in patients treated with olanzapine or risperidone on the Neuropsychiatric Inventory total score, with risperidone on the Clinical Global Impression of Change, with olanzapine or risperidone on the Brief Psychiatric Rating Scale (BPRS) Hostile Suspiciousness factor, and with risperidone on the BPRS Psychosis factor at the end of phase I. There was worsening with olanzapine on the BPRS Withdrawn Depression factor.
In this descriptive analysis of clinical outcomes in AD outpatients in usual care settings, some clinical symptoms improved with atypical antipsychotic treatment. The authors concluded that antipsychotic medications may be more effective for particular symptoms, such as anger, aggression, and paranoid ideas. Functional abilities, care needs, or quality of life did not appear to improve with antipsychotics.
Vigen C.L.P. Mack W.J, Keefe R et al. Cognitive Effects of Second Generation Antipsychotic
Medication in Patients with Alzheimer's Disease: Outcomes from CATIE-AD. American Journal of Psychiatry. 2011;168(6):831-39. CATIE-AD included 421 Alzheimer's disease patients with psychosis or agitated behavior, randomized to blinded flexible-dose olanzapine, quetiapine, risperidone or placebo. Based on clinician's judgment, patients could discontinue originally assigned medication and be randomized to another medication. They were followed for 36 weeks. Cognitive assessments were obtained at baseline, 12 weeks, 24 weeks and 36 weeks. Outcomes were compared among 357 patients with baseline and at least one follow-up cognitive measure obtained while on their prescribed medication or placebo for at least 2 weeks before cognitive testing.
Patients showed steady, significant declines over time in most cognitive areas, Patients on antipsychotics declined more than patients on placebo for multiple cognitive measures.
Agitation
Battaglia J., Moss S., Rush J et al. Haloperidol, Lorazepam or Both for Psychotic Agitation?
A multi-center, prospective, double-blind emergency department study. American Journal of
Emergency Medicine. 1997;15(4):335-340.
Ninety-eight psychotic, agitated, and aggressive patients were prospectively enrolled during
an 18-month period in emergency departments in five university or general hospitals. Patients
were randomly assigned to receive intramuscular injections of lorazepam (2 mg), haloperidol
(5 mg), or both in combination. Patients in each treatment group received 1 to 6 injections of
the same study drug within 12 hours, based on clinical need. They were evaluated hourly
after the first injection until at least 12 hours after the last. Efficacy was assessed on the
Agitated Behavior Scale, a modified Brief Psychiatric Rating Scale, Clinical Global
impressions scale, and an Alertness Scale. Effective symptom reduction was achieved in each
treatment group with significant (P < .01) mean decreases from baseline at every hourly ABS
evaluation. Significant (P < .05) mean differences on the ABS (hour 1) and MBPRS (hours 2
and 3) suggest that tranquilization was most rapid in patients receiving the combination
treatment. Side effects incidence did not differ significantly between treatment groups, although patients receiving haloperidol alone tended to have more extrapyramidal system symptoms. The authors conclude that superior results are produced by the combination treatment and support the use of lorazepam plus haloperidol as the treatment of choice for acute psychotic agitation.
Kwentus J. Riesenberg RA. Marandi M. Manning RA. Allen MH. Fishman RS. Spyker DA. Kehne JH. Cassella JV. Bipolar Disorder. 2012;14:31-40.
Rapid acute treatment of agitation in patients with bipolar I disorder: a multicenter, randomized, placebo-controlled clinical trial with inhaled loxapine. Bipolar Disorders. 2012;14(1):31-40,
This randomized, double blind, placebo-controlled, multi-center study of 314 inpatients with agitation associated with with bipolar I disorder. Subjects were randomized to inhaled loxapine 5 mg or 10 mg, or inhaled placebo. Patients receiving Dose 1 were evaluated for 24 hours. If required, up to two additional doses of study drug and/or lorazepam rescue medication were given. The primary efficacy endpoint was change from baseline in the Positive and Negative Syndrome Scale-Excited Component (PANSS-EC) score two hours after Dose 1. The secondary endpoint was the Clinical Global Impression-Improvement score two hours after Dose 1. Safety was assessed by adverse events, vital signs, physical examinations, and laboratory tests. For the primary and key secondary endpoints, both doses of inhaled loxapine significantly reduced agitation compared with placebo. Reduced agitation, as reflected in PANSS-EC score, was evident 10 min after Dose 1 with both doses. Inhaled loxapine was well tolerated, and the most common adverse events were known effects of loxapine or minor oral effects common with inhaled medications. The authors concluded that inhaled loxapine provided a rapid, non-injection, well-tolerated acute treatment for agitation in patients with bipolar I disorder.
Impulse Control Disorders
Coccaro, EF, Lee RJ, Kavoussi RJ. A Double Blind, Placebo Controlled Trial of
Fluoxetine in Patients with Intermittent Explosive Disorder. Journal of Clinical
Psychiatry. 2009;70(5):653-662.
A double-blind, randomized, placebo-controlled trial of fluoxetine conducted in 100 individuals with Intermittent Explosive Disorder (research diagnostic criteria) and current histories of impulsive aggressive behavior. The primary measure of efficacy was the aggression score from the Overt Aggression Scale-Modified (OAS-M) for Outpatient Use. Secondary efficacy measures included the irritability score from the OAS-M and the Clinical Global Impressions-Improvement scale (CGI-I) score. The study took place between July 1990 and July 1999.
Fluoxetine treatment resulted in a sustained reduction in OAS-M aggression, and OAS-M irritability scores, apparent as early as week 2 (p < .01 for aggression and p < .001 for irritability at endpoint). Fluoxetine was also superior to placebo in the proportion of responders on the CGI-I (p < .001). Closer examination of the data revealed that full or partial remission of impulsive aggressive behaviors occurred in 46% of fluoxetine-treated subjects. Fluoxetine did not exert an antidepressant or antianxiety effect, and its effects on
impulsive aggression were not influenced by presence of current symptoms of depression or anxiety. Fluoxetine can reduce aggressive behaviors in those diagnosed with intermittent explosive disorder.
APPENDIX C
Assessment and Scales
Several Scales have been developed to measure the propensity for and severity of violent and
aggressive behavior.
The scales listed below are the best in terms use in prospective studies.
For psychiatric clinicians:
Overt Aggression Scale
Overt Aggression Scale – Modified For nurses and other staff: Staff Observation of Aggression Scale Staff Observation of Aggression Scale - Revised The Excited Component from the Positive and Negative Syndrome Scale (PANSS-EC) is a validated scale to assess agitated patients. The PANSS-EC consists of 5 items taken from the PANSS that clinicians can quickly and routinely assess: excitement, tension, hostility, uncooperativeness, and poor impulse control. The 5 items are rated from 1 (not present) to 7
(extremely severe) with scores ranging from 5 to 35 (scores ≥ 20 correspond to severe agitation. Violence Risk Assessment Tools – Otto RK, Douglas KS. Handbook of Violence Risk Assessment. Routledge. New York, 2010.
References:
Palmstierna T., Wistedt B. Staff Observation Aggression Scale, SOAS: Presentation and
Evaluation. Acta Psychiatrica Scandanavica. 1987;76(6):657-663.
Nijman H. Palmstierna T. Measuring Aggression with Staff Observation. Acta Psychiatrica
Scananavica. 2002;412:101-102.
Yudofsky S.C., Slivler J.M., Jackson W et al. The Overt Aggression Scale for Objective
Rating of Verbal and Physical Aggression. American Journal of Psychiatry. 1986;143:35-39.
Knoedler D. W. The Modified Overt Aggression Scale. American Journal of Psychiatry.
1989;146(8):1081.
APPENDIX D
Areas for Future Research
Establishing the effectiveness of various interventions among patients prone to violence and
aggression has been limited by ethical constraints. In situations involving acute, frequently
unanticipated, events obtaining informed consent for participation is frequently not practical.
Reliance on prospective observational trials has been helpful in a limited number of studies.
More of such studies are needed to establish an evidence base for use of many long accepted
interventions for treatment of agitation, aggression and violence.
Further studies in special populations such as personality disorders, intellectually disabled,
traumatic brain injured and demented patients are needed to assure that benefits of treatment
outweigh iatrogenic morbidity and mortality.
APPENDIX E
Multiple choice questions
While there is widespread public perception the patients with schizophrenia are prone to
violent acts epidemiological studies have repeatedly demonstrated a strong relationship
between aggressive behaviors and:
A. Personality disorders
B. Substance Use Disorders
C. Financial Stresses
D. Social Isolation
(Correct answer: B.)
The best evidence for violent behavior among patients with brain disease is for disorder
involving?
A. Frontal Lobe
B. Temporal Lobe
C. Parietal Lobe
D. Corpus Striatum
E. Limbic System
(Correct answer: A)
In approaching the patient with agitation without clear etiology which of these should be
utilized first?
A. Voluntary use of oral benzodiazepines
B. First-generation antipsychotics with promethazine
C. Second-generation antipsychotics intramuscularly
D. Confrontation
E. Verbal De-escalation
(Correct answer: E
Evidence exists for aggressive behavior following the use of these addictive substances
except?
A. Methamphetamines
B. Cocaine
C. alcohol D. synthetic cathinones E. Hallucinogens (Correct answer: E) Among patients with the diagnosis of Intermittent Explosive Disorder which of the following pharmacological agents has shown efficacy in randomized control trials:
A. Olanzapine B. Benztropine C. Fluoxetine D. Alprazolam E. Methylphenidate
(Correct Answer: C)
Source: http://www.eapm.eu.com/tl_files/content/Publications/APM-EAPM-Aggression-Violence.pdf
Banking on cord blood stem cells lion cells, whereas the lower threshold for public banking is 1–1.5 billion. Only 8–12% of banked units have enough cel s to transplant New research will shed light on claims from commercial banks that an average ( 80 kg) size adult.cord blood–derived stem cells can be used in diseases beyond One strategy to get around this limit is to
Acta Crystallographica Section A Early days in drug discovery by crystallography – personal recollections Received 10 December 2012 Accepted 11 December 2012 The Walter and Eliza Hall Institute of Medical Research, 1G Royal Parade, Parkville, Victoria, Australia. Correspondence e-mail: The influences of Lawrence Bragg and Max Perutz are evident in thecontemporary emphasis on ‘structural enablement' in drug discovery. Onthis occasion of the centenary of Bragg's equation, his role in supporting theearliest structural studies of biological materials at the Cavendish Laboratory isremembered. The 1962 Nobel Prizes for the structures of DNA and proteinsmarked the golden anniversary of the von Laue and Bragg discoveries.