Doi:10.1016/j.ophtha.2006.01.07
Deep Lamellar Keratoplasty
by Intracorneal Dissection
A Prospective Clinical and Confocal Microscopic Study
Giorgio Marchini, MD,1 Leonardo Mastropasqua, MD,2 Emilio Pedrotti, MD,1 Mario Nubile, MD,2Marco Ciancaglini, MD,2 Arianna Sbabo, MD1
To evaluate the clinical findings, visual outcomes, and confocal microscopic corneal features of a
surgical technique for manual deep lamellar keratoplasty (DLKP) with intentional sparing of the most posterior stroma.
Noncomparative, prospective, 12-month interventional study.
Forty-six eyes of 45 patients who had corneal pathologic features without endothelial abnor-
malities and requiring corneal graft were treated by DLKP by manual stromal delamination. They were examinedclinically after surgery and using in vivo confocal microscopy at 2 weeks and 1, 3, 6, and 12 months.
The surgical technique consisted of an intracorneal deep manual stromal dissection through
a 4-mm limbal incision at 50 m from Descemet's membrane (DM). After trephination, an endothelial free graftwas sutured.
Main Outcome Measures:
Topographic parameters, interface depth and reflectivity, and anterior and
postinterface keratocyte density; visual acuity was correlated with these parameters.
Two eyes had rupture of the DM. Two eyes that had delayed epithelial healing because of graft
override with stromal inflammation underwent a second surgery (penetrating keratoplasty). Mean uncorrectedlogarithm of the minimum angle of resolution (logMAR) uncorrected visual acuity and logMAR best-correctedvisual acuity (BCVA) improved from preoperative values (1.342⫾0.239 and 0.923⫾0.226, respectively) to0.421⫾0.122 and 0.104⫾0.068, respectively, at 12 months. Mean topographic astigmatism was 3.09⫾1.30diopters (D) at 3 months after suture adjustment, and 2.87⫾0.92 D at 12 months after suture removal. Averageinterface depth was 64.2⫾6.7 m at 15 days and showed no significant changes up to 12 months. Meaninterface reflectivity was highest at 15 days (95.5⫾15.7 light reflectance units [LRU]) and showed a progressivedecrease over time of 55.3⫾8.7 LRU at 12 months. A significant negative correlation was observed betweenBCVA and topographic astigmatism up to 1 month and between BCVA and interface reflectivity starting from 6months after surgery.
Deep lamellar keratoplasty by intracorneal dissection provides visual and clinical results
comparable with that of other DLKP techniques. Visual recovery is slow and progressive, taking up to 1 year.
Confocal microscopy enables precise evaluation of corneal features, interface morphologic features, andreflectivity, demonstrating a negative correlation between interface reflectivity and BCVA showing that theprogressive recovery over months of the interface transparency is correlated with the increase in visual acuityafter 6 months.
Ophthalmology 2006;113:1289 –1300 2006 by the American Academy of Ophthalmology.
Lamellar keratoplasty (LKP) is a corneal graft technique
able aspects with respect to penetrating keratoplasty (PKP).
consisting in the transplantation of partial thickness donor
Because it is an extraocular procedure, it has a more limited
cornea without endothelium, Descemet's membrane (DM),
risk of complications, such as anterior synechia, secondary
and rear stroma onto a recipient healthy stromal bed after
glaucoma, or Because LKP maintains the
dissection of pathologic anterior cornea. It presents favor-
recipient's endothelium in place, there is no risk of endo-thelial rejection and consequently no need for long-termimmunosuppressive therapy, decreasing the incidence of
Originally received: July 7, 2005.
infection, glaucoma, and It also offers a superior
Accepted: January 24, 2006.
Manuscript no. 2005-621.
wound strength, the sutures can be removed earlier, and it
1 Eye Clinic, Department of Neurological and Visual Sciences, University
requires less rigid criteria for donor corneal tissue selec-
of Verona, Verona, Italy.
Despite these advantages, the main clinical concern
2 Department of Medicine and Aging Science, Ophthalmic Clinic, Univer-
that limits the applications of LKP as a therapeutic kerato-
sity of Chieti-Pescara, Chieti-Pescara, Italy.
plasty is that the resulting visual acuity is not as good as that
Correspondence to Emilio Pedrotti, MD, Eye Clinic, Department of Neu-
obtained with The reason for the poor visual
rological and Visual Sciences, University of Verona, Borgo Trento Hos-pital, Piazzale Stefani, 1, Verona 37126, Italy.
acuity after LKP is thought to be the scarring that involves
2006 by the American Academy of Ophthalmology
ISSN 0161-6420/06/$–see front matter
Published by Elsevier Inc.
Volume 113, Number 8, August 2006
the interface between the graft cornea and the recipient
point of more than 300 m; and (4) absence of other ocular
stromal bed. Deep lamellar keratoplasty (DLKP) has been
pathologic features such as glaucoma or retinal diseases. The
proposed as a surgical alternative procedure to avoid inter-
original diseases were keratoconus with contact lenses intolerance
face It consists of the removal of all recipient
(34 eyes), stromal dystrophies (5 eyes), corneal leucoma (5 eyes),and stromal opacity occurring after herpes keratitis (2 eyes). All
stromal tissue down to DM and the transplantation of the
patients enrolled in the study gave informed consent, and the
donor cornea without endothelium over the host bed. Deep
principles of the Helsinki Declaration and good clinical practice
lamellar keratoplasty presents the advantage of a greater
were followed. A complete ocular examination, including uncor-
improvement in postoperative visual acuity with respect to
rected visual acuity (UCVA) and best-corrected visual acuity
LKP and compares favorably with PKP while maintaining
(BCVA) evaluation, slit-lamp biomicroscopy, applanation tonom-
the same advantages of Deep lamellar kerato-
etry, fundus examination, computerized topography, specular mi-
plasty is indicated in many pathologic features where PKP
croscopy endothelial cell density, and ultrasound pachymetry were
was previously regarded as the first surgical choice in pa-
performed before surgery. Each patient was examined in the post-
tients with healthy endothelium and the absence of stromal
operative period at 15 days and 1, 3, 6, and 12 months after
edema, such as corneal scarring resulting from keratitis,
surgery. Each follow-up visit included UCVA and BCVA, slit-lamp biomicroscopy, endothelial specular microscopy (Noncon
corneal dystrophies, and The main concern
Robo-P, Konan, Hyogo, Japan), ultrasound pachymetry (Ophtha-
regarding DLKP is the difficulty of the surgical procedure:
sonic, Teknar, St. Louis, MO), and in vivo confocal microscopy of
perforation of DM is the main intraoperative risk, especially
the cornea (Confoscan 3, Nidek Technologies, Padova, Italy).
when DM is completely exposed free of overlying If
Visual acuity measurements were performed using Snellen acuities
perforation occurs, even if DLKP can be completed in some
and were analyzed using logarithm of the minimum angle of
cases, the stromal dissection may be difficult, leading to a
resolution (logMAR) equivalents for statistical analysis. Corneal
low-quality corneal bed. Furthermore, when conversion of the
topography was performed using an EyeTop instrument (CSO
procedure into PKP is needed because of significant breaks in
Ophthalmic, Firenze, Italy), and topographic astigmatism was
DM, good quality endothelium of donor cornea may not be
measured using a simulated keratometry value given by the power
It is not clear whether a complete stromal excision
and axis of the steepest meridian and that of 90°. Surface regularityindex (SRI) and surface asymmetry index (SAI) were analyzed to
baring DM provides better visual results than cases in which a
study quantitatively the irregularity of topographic
small portion of rear stroma is left undissected. Sugita and
Intraoperative and postoperative complications also were recorded.
reported that leaving a small amount of stroma doesnot produce differences in visual acuity compared with com-
plete stromal dissection, as long as the deep stroma is healthy.
Thus, intentional sparing of the deepest stroma could be help-
All the DLKP surgeries were performed under general anesthesia
ful in preventing intraoperative DM rupture.
at the Eye Clinic of the University of Verona. To facilitate and
We developed a new kit of instruments for DLKP based on
speed up the procedure, we designed a special surgery kit com-
blunt spatula manual delamination, and we named the surgical
posed of a precalibrated diamond knife (Janach, Como, Italy), a
technique DLKP by intracorneal dissection; this technique
2.25-mm surgical knife with a round head angled 60° with respectto the handle (BD Edge Ahead Circular knife, BD Ophthalmic
intentionally leaves a minimal thickness of deep stroma on the
Systems, Bidford-on-Avon, United Kingdom), a double-ended
host bed, without the aid of air or fluid in dissection, before
spatula (short and long) for stromal tissue delamination (Janach,
suturing the donor button. The theoretical advantages of such
Como, Italy), a Hanna trephine (Moria, Paris, France), forceps for
a technique are: (1) the reduced risk of intraoperative compli-
stromal peeling and for donor button endothelium removal (Ja-
cations such as DM rupture and the formation of a double
nach), and a punch for donor button (Moria). Central and periph-
anterior chamber, and (2) the lower complexity of the DLKP
eric corneal thicknesses were measured using an ultrasonic
procedure, generally demanding greater surgical skills to han-
pachymeter (Ophthasonic, Teknar, St. Louis, MO). The surgical
dle correctly the extremely thin DM– endothelium layer.
procedure started with a 4-mm limbal incision with a precalibrated
The purpose of this prospective study was to evaluate at
diamond knife at the 10-o'clock position. The knife calibration
12 months of follow-up the complication rate, visual out-
was set to the value of the thinnest corneal thickness minus 50 mto spare the endothelium, DM, and a thin deep stromal layer. Then
come, confocal microscopic interface features, and their
a cleavage plane was formed by creating a small stromal pocket
correlation with visual acuity in a cohort of patients treated
with the angulated bevel up. Subsequently, this pocket was en-
with DLKP by manual intracorneal dissection.
larged with the short dissector starting the deep stroma dissection.
The intrastromal cleavage delamination continued with the longdissector to dissect 80% of the stromal extension, or at least
Patients and Methods
extending across an area that covered the central 9-mm diameter.
The deep stromal pocket was filled up with low cohesive and low
Patient Population and Clinical Examinations
molecular weight viscoelastic (IAL-F, Fidia Farmaceutici S.p.A.,Abano Terme, Italy). This kind of viscoelastic was chosen to
Between August 2001, and July 2003, 46 eyes of 45 patients (29
reduce the risk of endothelium perforation during the trephination
males and 17 females; mean age, 35.6⫾14.1 years; range, 6 –70
of recipient button with Hanna trephine. The recipient button was
years) were enrolled consecutively in this prospective noncom-
7.75 mm in 7 cases, 8.00 mm in 31 cases, and 8.25 mm in 8 cases.
parative study. All eyes underwent deep lamellar keratoplasty
A sclerocorneal button stored in organ culture at 31° C and
(DLKP) with intracorneal dissection technique. Criteria for eligi-
provided by the Eye Bank Fondazione Banca degli Occhi del
bility were: (1) corneal pathologic features requiring graft without
Veneto (Venezia-Mestre, Italy) was used for the preparation of the
evidence of endothelial impairment; (2) endothelial cell density
donor cornea in all cases. The donor cornea was trephined from the
more than 1800 cell/mm2; and (3) corneal thickness at the thinnest
endothelial side with Moria punch with a 0.25-mm bigger diameter
Marchini et al 䡠 Deep Lamellar Keratoplasty by Intracorneal Dissection
than the recipient bed. Endothelium and DM were removed from
cluded in the scan. Because the reliability of the Z-scan graphic is
the donor button with dedicated forceps. This was carried out by
influenced by eye movements during the scan period, only reliable
placing the donor button on a sterile plastic support with the
and comparable graphics for each corneal examination were con-
endothelial face up. While a Pierce forceps blocked the button, a
sidered for analysis.
second dedicated forceps peeled out DM and endothelium. Four
Interface was defined as the corneal sublayer located in the
interrupted 10-0 nylon sutures (Ethilon Black, Johnson & Johnson,
posterior stroma with evident discontinuity of the stromal kerato-
St. Stevens Woluwe, Belgium) at 12, 6, 3, and 9 o'clock secured
cyte and extracellular matrix architecture. The interface depth was
the corneal button in the recipient bed. Then, a single continuous
calculated as the distance between the proper interface and the
nylon 10-0 running suture (NU-1, Alcon Laboratories, Inc., Fort
endothelial layer. Each value of interface depth was considered as
Worth, TX) with 20 bites was placed. After removal of the inter-
the average of 3 measurements obtained from 3 reliable Z-scan
rupted suture, intraoperative adjustment of astigmatism was per-
graphics. Interface reflectivity also was calculated as the average
formed using the Maloney keratometer (Duckworth and Kent,
of 3 light reflectance unit values obtained by 3 reliable Z-scan
Baldock, UK). An association of 0.05% formocortal and 0.03%
sulphate gentamicin was instilled topically at the end of the sur-
Mean keratocyte density of anterior and postinterface residual
gery. An extended-wear therapeutic soft contact lens (Protek T&S,
stroma was calculated using the analysis software provided with
Contact Vision, Marcon, Italy) was placed on the cornea and the
the instrument, which allows manual cell count within a selected
eye was patched.
region of interest of standardized dimension (0.1 mm2). Keratocyte
Postoperative therapy included the topical application 6
cell density values of anterior (depth range, 50 –100 m from the
times daily of a corticosteroid-antibiotic solution composed of
basal lamina of epithelium) and residual host stroma (between
0.1% bisodium phosphated betamethasone, 0.4% chloramphen-
endothelium and interface layers) were obtained as an average of
icol, 0.421% tetracycline, and 18 000 000 IU of sodic colis-
5 images per eye.
timethate. Eye drops were tapered within 3 months after surgery
Confocal microscopy was performed before surgery in all eyes
with the following schedule: 6 times daily for 20 days, 5 times
to assess endothelial cell density. Postoperative endothelial cell
daily for 10 days, 4 times daily for 10 days, 3 times daily for 10
count was obtained for each eye at every follow-up examination.
days, 2 times daily for 10 days, once daily for 10 days, and on
The endothelial layer was imaged correctly for all patients. The
alternate days for the final 20 days.
mean of 3 measurements of endothelial cell density was calculated
Suture adjustments were performed when topographic astigma-
using Confoscan 3 dedicated analysis software and performing a
tism was superior to 3.5 diopters (D) within the third and fourth
manual cell count processing within a 0.1-mm2 standardized re-
postoperative week. In case of regression of the effect, postoper-
gion of interest in the central cornea.
ative adjustment was repeated for a maximum of 3 times up to 3months after surgery. Suture removal was performed 6 to 8 months
after surgery.
Statistical analysis was performed with SPSS 10.1 for Windows(SPSS Inc., Chicago, IL). Data were expressed as mean⫾standard
In Vivo Confocal Microscopy
deviation, and a
P value of less than 0.05 was considered statisti-
In vivo confocal microscopy (IVCM) was performed using a
cally significant. Interface depth, interface reflectivity, keratocyte
scanning slit confocal microscope (Confoscan 3). This instrument
density values, topographic astigmatism, SRI and SAI values, and
was equipped with an Achroplan (Zeiss, Oberkochen, Germany)
visual parameters (UCVA, BCVA) at different follow-up exami-
nonapplanating ⫻40 immersion objective lens designed for full-
nations were compared using a 1-way analysis of variance.
thickness examination of the cornea, with a working distance of
Tukey's post hoc test was used to detect statistically significant
1.92 mm and a motorized focusing device. The center of the
differences between values. The correlation between postoperative
cornea was studied during all examinations. A drop of topical
visual parameters and interface depth, interface reflectivity, ker-
anesthetic 0.4% oxybuprocaine chlorohydrate (Novesina, Novartis
atocyte density, and topographic parameters was analyzed using
Farma S.p.A., Origgio, Italy) was instilled before the examination.
The patient was seated in front of the microscope, a chin rest anda forehead support were used, and the patient was asked to fix a
bright object with the contralateral eye to minimize eye movementduring the examination. One drop of 0.2% polyacrylic gel (Vis-
Graft Clarity and Complications
cotirs Gel, CIBA Vision Ophthalmics, Marcon, Venezia, Italy)was applied on the objective tip to serve as an immersion fluid.
The surgical procedure was completed in 45 of 46 eyes, and 2
Two complete confocal examinations of the entire central cor-
intraoperative complications were observed. In 1 eye, a microper-
nea were performed for each eye with a total examination time of
foration of DM occurred during the trephination phase, but this did
less than 5 minutes. The ConfoScan 3 acquires 350 images per
not affect the subsequent surgical steps, leading to the uneventful
examination at a rate of 25 frames per second, and therefore, the
completion of the DLKP procedure. This was because the perfo-
capture time is 14 seconds. The images are stored in memory and
ration was less than 2 mm and out of the optical zone and because
directly saved to the hard drive. Each frame is approximately
the anterior chamber was maintained by an injection of a high
400⫻300 m, with a scanning area of 0.12 mm2. The main
molecular weight viscoelastic. One eye had a bigger perforation
parameters for the sequence acquisition were set using 3 passes,
during stromal dissection phase requiring conversion of the pro-
for each complete corneal examination and a z-axis movement
cedure into PKP. In this case, the DM– endothelium rupture was on
range of 1000 m, giving a theoretical z-axis distance between
the optical zone, and the viscoelastic was unable to maintain the
images in the scans of 10 m. The position on the z-axis of the
anterior chamber. A full-thickness corneal trephination similar
corneal thickness of each image was obtained using the Z-scan
to a standard PKP, followed by the apposition of an entire
function of the instrument. The Z-scan is a graph showing the
corneal button sutured with a single continuous running suture,
depth coordinate (expressed in micrometers) on the z-axis and the
was performed.
level of reflectivity (expressed in arbitrary numerical units, called
Delayed epithelial healing resulting from graft override with
light reflectance units) on the y-axis for each corneal image in-
stromal inflammation, unresponsive to therapy, occurred within 3
Volume 113, Number 8, August 2006
Figure 1. Graph showing the mean postoperative logarithm of the minimum angle of resolution (logMAR) uncorrected visual acuity (UCVA) and
best-corrected visual acuity (BCVA) changes over time after deep lamellar keratoplasty. Each increment of both UCVA and BCVA was significant with
respect to previous time values. Note that the greatest increase of BCVA was between 3 and 6 months, whereas topographical parameters did not show
significant changes at this time point.
months after surgery in 2 eyes. Both eyes were treated with a
provement of both BCVA and UCVA over time, at each follow-up
subsequent PKP. A mild button haziness and edema were recorded
examination, was observed. Notable relationships between speed
in 1 eye 7 months after DLKP. This complication underwent
of recovery of visual acuity and either age or original disease were
complete resolution and normal button transparency was achieved
not observed.
within 7 days of medical treatment (dexamethasone 0.2% eye-
Mean postoperative corneal topographic astigmatism was
drops, 6 times daily for the first week and then tapered during the
6.86⫾3.51 D 15 days after surgery, 3.09⫾1.30 D at 3 months after
following 8 weeks). No other complications occurred in any eyes
eventual suture adjustment, and 2.87⫾0.92 D at 12 months after
over the entire follow-up period.
suture removal. The mean time of suture removal after surgery was
With respect to graft clarity, an interface mild opacity, visible
209⫾62 days. Variations of mean corneal topographic astigma-
at slit-lamp examination, was noted in all cases during the first
tism, SRI, and SAI over the 12-month follow-up are reported in
period after surgery. This slight interface haziness presented
Ninety-one percent of eyes (39 of 43) underwent 1 or
biomicroscopic clinical characteristics of edema that resolved
more (up to 3) suture adjustments between 15 days and 3 months
within 2 to 4 months after DLKP. However, the donor corneal
after surgery. Topographic data at 15 days indicated postoperative
button was found to be biomicroscopically clear in all eyes during
astigmatism before suture adjustment and at 1, 3, and 6 months
the entire follow-up, except in those 2 patients who experienced
after eventual suture adjustments, and at 12 months after suture
the above-mentioned postoperative complications. Epithelial
removal. A significant overall decrease (
P⬍0.001, analysis of
pathologic features, such as epithelial edema or microerosions,
variance) of topographic astigmatism was related to the differences
were not observed in any eye.
between 0.5 to 1 month and 1 to 3 months Surfaceregularity index and SAI postoperative values showed a significanttendency toward decrease (
P ⫽ 0.013 and
P ⫽ 0.004, respectively,
Visual Outcome and Topographic Astigmatism
analysis of variance). However, the comparison at different time
In the 43 eyes observed for 12 months, the average preoperative
points indicated a significant difference only for SRI between 0.5
logMAR BCVA was 0.923⫾0.226, and the mean postoperative
and 12 months and for SAI between 0.5 and 6 to 12 months, as
logMAR BCVA improved to 0.104⫾0.068 at the end of follow-up
(
P⬍0.001). Average logMAR UCVA improved from a preopera-tive value of 1.342⫾0.239 to 0.421⫾0.122 at 12 months after
In Vivo Confocal Microscopy
surgery (
P⬍0.001). In 41 of 43 eyes (95.3%), logMAR BCVA was0.2 or better, whereas in 30 of 43 eyes (69.7%), it was 0.1 or better,
A deep lamellar interface was identified in all examined eyes at all
at 12 months. shows the changes in postoperative BCVA
follow-up examinations. This appeared at confocal examination as
and UCVA during the follow-up. A statistically significant im-
a corneal sublayer with unique morphologic characteristics in the
Marchini et al 䡠 Deep Lamellar Keratoplasty by Intracorneal Dissection
Table 1. Topographic Astigmatism, Surface Regularity Index,
face morphologic features at different postoperative times are
and Surface Asymmetry Index during Follow-up
presented in a typical Z-scan graphic showing the inter-face depth determination is presented in
Mean interface depth (defined as distance from endothelium) at
15 days after surgery was 62.2⫾6.7 m (range, 45–74 m) and
remained stable without significant variations during the entire
follow-up Mean interface reflectivity values at each
examination are reported in Interface reflectivity was
found to be highest at 15 days and at 1 month (95.5⫾15.7 and
84.5⫾8.4 light reflectance units, respectively) and presented asubsequent and progressive decrease, indicating that tissue trans-
D ⫽ diopters.
parency was regained. Statistically significant changes were ob-
*P⬍0.001 between 0.5 and 1 month.
served between 15 days and 1 month and between 3 and 6 months.
†P⬍0.001 between 1 and 3 months.
Morphologically, the cause of the increased reflectivity of the
P ⫽ 0.007 between 0.5 and 12 months.
interface, evidenced in the first period after surgery, was likely to be
P ⫽ 0.020 between 0.5 and 6 months.
储P ⫽ 0.003 between 0.5 and 12 months (analysis of variance–Tukey post
interface edema presenting an accumulation of reflective interface
fluid, rather than cellular activation or interface scarring
Mean anterior and postinterface stromal keratocyte density
values at every examination are shown in No statistically
cornea represented by evident discontinuity of stromal cellular and
significant changes in anterior and posterior mean cell density
extracellular architecture of the overlying and underlying rear
were observed during the follow-up period. Eyes with keratoco-
stroma, absence of distinguishable keratocytes, presence of homo-
nus, but not those affected by other diseases, showed that the
geneous reflectivity, variable transparency, and possible presence
stromal layers underlying the interface (i.e., host residual stromal
of bright microdots. In vivo confocal microscopy images of inter-
tissue) presented hyporeflexive streaks. shows a sequence
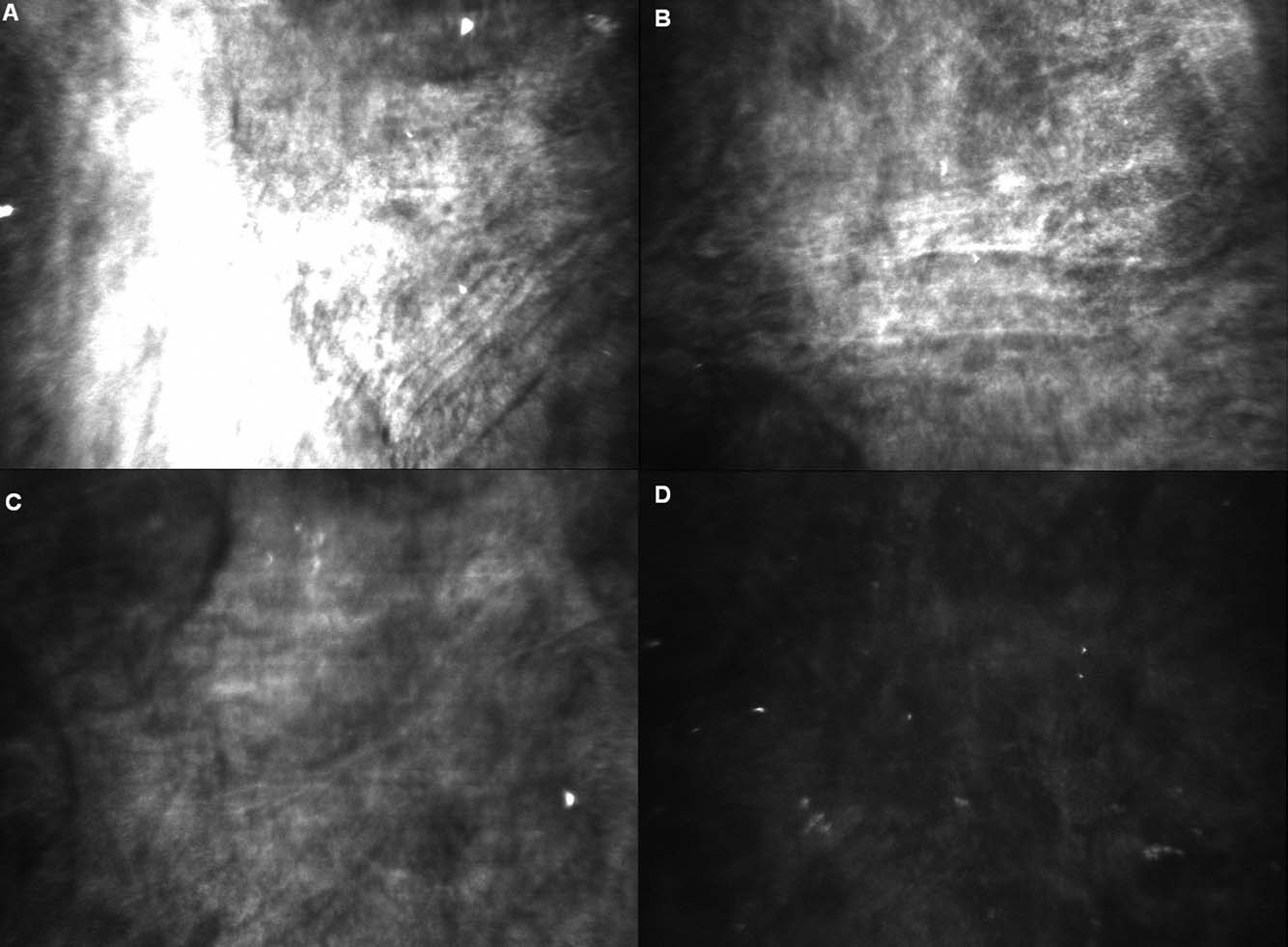
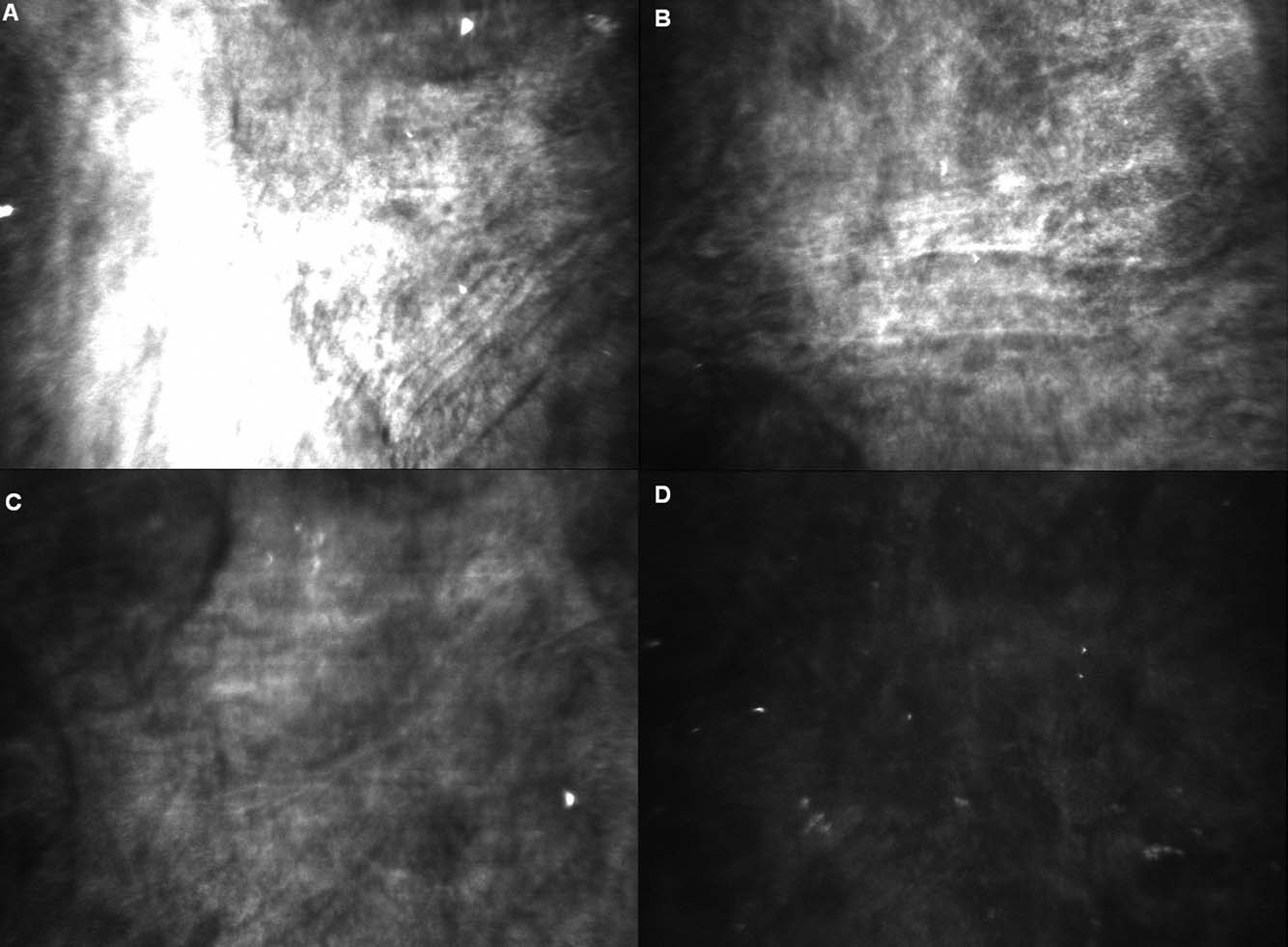
Figure 2. Confocal images of the interface of the same patient at (A) 15 days, (B) 3 months, (C) 6 months, and (D) 12 months after deep lamellar
keratoplasty. Note the progressive reduction of haziness and brightness, associated with the recovery of transparency: keratocytes became visible from
adjacent layers, as well as some bright microinclusions similar to those visible in LASIK interfaces.
Volume 113, Number 8, August 2006
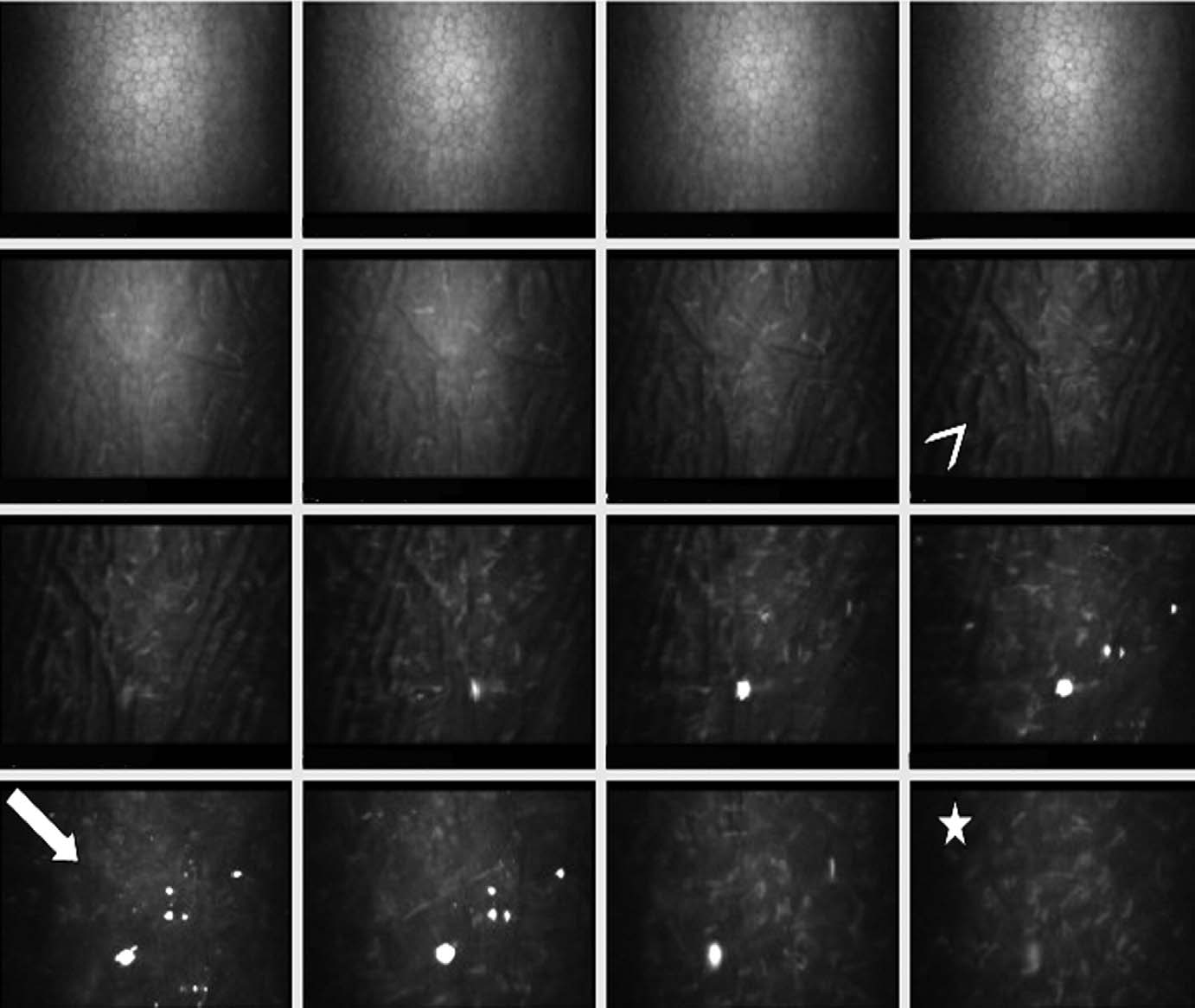
Figure 3. Z-scan graphic showing interface depth determination: 3 consecutive Z-scan graphics of a confocal scan 15 days after surgery. Endothelial and
epithelial reflectivity peaks were visible in the left and right edge of each graphic, respectively. A preendothelial high reflective peak representing the
interface reflectivity spike was visible (arrow). The green band on the second curve represents the z-axis distance between the interface and the endothelial
layer.
of images of the posterior corneal layers, including interface, after
BCVA and topographic astigmatism, SRI, and SAI up to 1 month
DLKP for keratoconus.
after surgery. Best-corrected visual acuity and interface reflectivity
Endothelial cell density values recorded over the follow-up are
values showed a significant negative correlation starting from 6
shown in Mean preoperative endothelial cell density was
months Other tested parameters did not show a signif-
2565⫾512 cell/mm2, whereas it was 2210⫾489 cell/mm2 at 15
icant correlation with visual acuity at the follow-up time points.
days after surgery (cell loss with respect to preoperative values,13.8%; P⬍0.001) and 2135⫾501 cell/mm2 at 1 month (cell losswith respect to 15-day values, 3.4%; P ⫽ 0.048). Ensuing changes
that were detected were not significant.
Several authors have reported a favorable visual outcome
after Recent results of comparison studiessuggest that DKLP can be considered as a safe alternative to
Uncorrected visual acuity showed a significant negative correla-tion with topographic astigmatism during the entire follow-up. A
PKP in the treatment of different anterior corneal pathologic
significant negative correlation between UCVA, SRI, and SAI
characteristics with stromal opacity and in keratoco-
were detected only up to 1 month and 3 months, respectively
In addition to comparable results in terms of
A significant negative correlation was observed between
visual recovery, DLKP presents several advantages with
Table 2. Interface Reflectivity, Interface Depth, and Mean Anterior and Posterior Keratocyte Density Changes over Follow-up
Time (mos)
Statistically significant changes were observed for interface reflectivity only between 0.5 and 1 month and 3 to 6 months after surgery.
Postoperative endothelial cell density showed a slightly significant decline between 0.5 and 1 month. A greater endothelial cell loss was observed betweenpreoperative and 0.5-month postoperative values (see text).
*P⬍0.001 between 0.5 and 1 month (Tukey post hoc test).
†P⬍0.001 between 3 and 6 months (Tukey post hoc test).
‡P ⫽ 0.048 between 0.5 and 1 month (Tukey post hoc test).
Marchini et al 䡠 Deep Lamellar Keratoplasty by Intracorneal Dissection
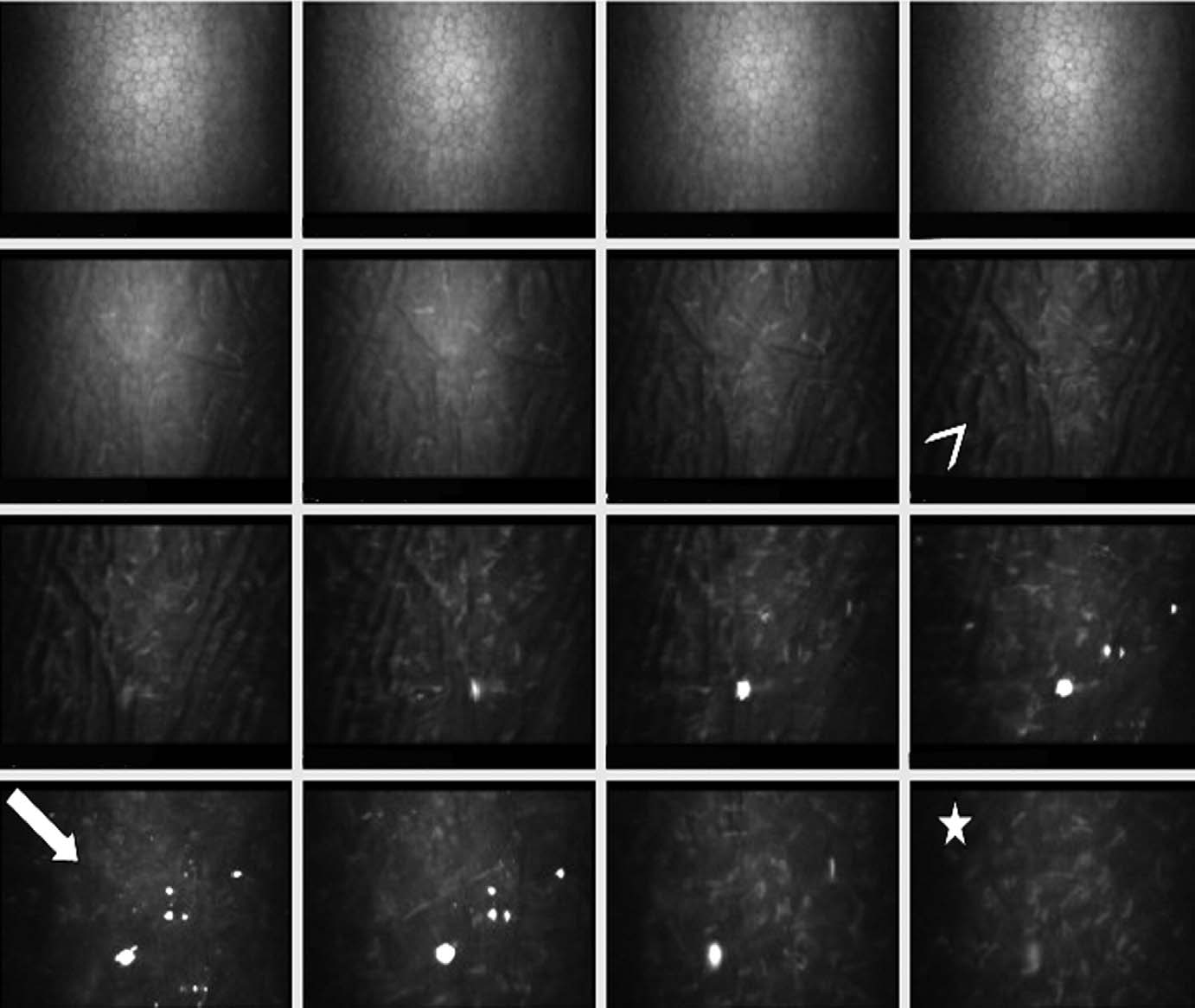
Figure 4. Sequential confocal scan images of the central cornea 12 months after deep lamellar keratoplasty for keratoconus. The images represent different
corneal layers on the z-axis starting from the endothelial plane toward the posterior stroma (from top left to bottom right). The endothelial layer was
evident in the sequence (first line) on top (⬎1 endothelial image was captured). The posterior residual host stromal bed was clearly imaged in the following
frames, and typical stromal keratoconus hyporeflexive striae were visible within keratocytes and extracellular architecture (arrowhead). Preinterface and
postinterface stromal layers were imaged in the following frames of third and fourth lines. The proper interface (arrow) presented absence of distinguishable
keratocytes and presence of bright microinclusions that extend toward the layer adjacent to the interface. Note that the interface was optically clear with
low reflectivity. The last 2 frames of the fourth line indicated that the initial posterior stromal layers of donor button evidenced normal architecture of
keratocytes and extracellular tissue transparency (star).
respect to PKP, mainly linked to the preservation of corneal
well-trained in corneal grafts. It is still an evolving technique,
host endothelium, leading to a lower risk of endothelial
lacks a standardization of procedures in the different indicating
rejection and late endothelial as well as a greater
pathologic characteristics, lacks long-term (years) results, and
availability of donor corneas that do not need perfectly
presents potential interface haze or irregularity, with the ensu-
healthy endothelium and high endothelial cell density to be
ing related negative influences on visual Inter-
suitable for corneal grafting. Other favorable aspects con-
face scarring leading to poor visual acuity represents one of
cerning DLKP are represented by a faster stabilization of
the greatest reservations that has limited the applications of
the wound, leading to earlier suture and a lower
LKP in the The deeper interface obtained
risk of open sky surgery-related complications such as en-
with new DLKP techniques has not been associated with
dophthalmitis. However, different theoretical disadvantages
a significant incidence of opacification and irregularity
are thought to influence DLKP procedures. Deep lamellar
occurring at the level of donor– host corneal lamellar
keratoplasty is technically difficult, demanding a surgeon
This aspect may affect the better visual
Volume 113, Number 8, August 2006
Table 3. Pearson's Correlation between Logarithm of the Minimum Angle of Resolution Uncorrected and Best-Corrected Visual
Acuity with Parameters That Showed Significant Correlation at a Minimum of 1 Follow-up Visit
Time (mos)
r ⫽ ⫺0.700
r ⫽ ⫺0.780
r ⫽ ⫺0.647
r ⫽ ⫺0.513
r ⫽ ⫺0.695
r ⫽ ⫺0.491
r ⫽ ⫺0.370
r ⫽ ⫺0.21
r ⫽ ⫺0.253
r ⫽ ⫺0.218
P ⫽ 0.011
r ⫽ ⫺0.308
r ⫽ ⫺0.491
r ⫽ ⫺0.345
r ⫽ ⫺0.268
r ⫽ ⫺0.207
P ⫽ 0.037
P ⫽ 0.001
P ⫽ 0.019
r ⫽ ⫺0.695
r ⫽ ⫺0.352
r ⫽ 0.270
r ⫽ 0.220
r ⫽ 0.218
r ⫽ ⫺0.561
r ⫽ ⫺0.540
r ⫽ ⫺0.235
r ⫽ ⫺0.198
r ⫽ ⫺0.203
r ⫽ ⫺0.602
r ⫽ ⫺0.405
r ⫽ ⫺0.222
r ⫽ ⫺0.232
r ⫽ ⫺0.212
P ⫽ 0.009
r ⫽ ⫺0.104
r ⫽ ⫺0.073
r ⫽ ⫺0.273
r ⫽ ⫺0.734
r ⫽ ⫺0.945
P ⫽ 0.047
BCVA ⫽ best corrected visual acuity; NS ⫽ not significant; SAI ⫽ surface asymmetry index; SRI ⫽ surface regularity index; UCVA ⫽ uncorrected visualacuity.
acuity results of DLKP, which presents values comparable
On the basis of the above-mentioned observations, we
with those after
performed a standardized surgical technique for lamellar
A possible explanation for the better interface transpar-
dissection with the aim of obtaining a reproducible DLKP,
ency of DLKP over traditional LKP may be the smooth host
using spatula-mediated manual deep delamination by which
surface obtained by separating DM from the deepest stroma
an intended host stromal residual layer of approximately 50
and the very slight optical disturbance of the donor stromal
m is left undissected above the DM–endothelial layer.
However, it has not been established clearly in
When performing a dissection in a nontrephined cornea, it is
literature which reasons are responsible for the different
easier to extend the cleavage plane on the entire corneal area
behavior affecting interface transparency of corneal tissues
creating a wide pocket, which allows a better apposition of
occurring either after LKP or DLKP. A recent report doc-
the donor button on the recipient bed even in presence of
umented that separation may occur between the anterior
more advanced ectasic pathologic features.
banded and the posterior nonbanded layer of DM in some
In the present study, we prospectively evaluated visual
cases during DLKP.Several techniques of stromal dissec-
results, complications rate and interface morphology, over a
tion down to DM have been proposed over the past years to
12-month follow-up period in eyes that underwent DLKP
facilitate a safe and efficient deep stromal
by intracorneal dissection for keratoconus (34 eyes) or
The original article by followed by other stud-
anterior stromal opacity (12 eyes). The main outcome mea-
described air injection into the stromal bed. Other
sures chosen for this study were specifically related to the
proposed delamination methods include hydrodelamination,
parameters for evaluating donor– host interface characteris-
in which a saline solution is used as a dissecting
tics of the graft. The potential for interface haze, although
viscoelastic dissection alone or after air injection into the
minimal, is considered to be a possible occurrence interfer-
anterior and the recent big bubble technique
ing negatively with visual performance in any kind of
based on air injection into the paracentral corneal stroma
corneal lamellar grafts; therefore, an objective method for
after partial-thickness Although providing
interface evaluation seemed to us as to be an important issue
smoother surfaces, baring the DM as a surgical goal requires
for at least 2 reasons. First, although a recent study of DLKP
that the surgeon deals with a very thin layer of residual host
reported interface opacification as a relatively infrequent
cornea (less than 40 m), resulting in a variable incidence
complication (incidence of 8% in the reported 25-patient
(between 0% and 39%) of DM Sugita
to our knowledge, quantitative methods have not
and Kondo, when comparing patients in whom the DM was
been used to measure interface transparency, and this has
exposed with patients who retained some portion of non-
been evaluated by using subjective slit-lamp biomicroscopic
pathologic deep stroma left during surgery, reported that no
examination. In fact, interface haziness should not be con-
differences in visual acuity and endothelial cell density were
sidered as a discrete parameter (i.e., present or not present),
found in a prospective study during a 12-month
but as a continuous variable inducing optical disturbance,
It is possible, although not clearly proven in literature, that
which may interfere differently with visual performance
intentional sparing from dissection of a thin layer of healthy
with a dependence on opacity location, quantity, and homo-
rear stroma during deep lamellar grafts may provide the
geneity. Moreover, the visual acuity obtained in previous
advantage of reducing the risk of DM puncture, allowing
studies of DLKP was correlated with interface transparency,
surgeons to perform the delicate phase of deep delamination
which may be a factor influencing visual acuity over time.
in a simpler manner.
Second, DLKP using deep delamination but without baring
Marchini et al 䡠 Deep Lamellar Keratoplasty by Intracorneal Dissection
DM theoretically may present greater problems of interface
(DM exposed or some deep stromal layers left undissected
optical quality (being somewhat similar in principle of
above the endothelium). Moreover, Shimazaki et in their
interface haze generation to LKP) than DLKP with DM
DLKP series for corneal pathologic features, except from
keratoconus, with 24-month follow-up observed that visual
In vivo confocal microscopy has been used widely in
acuity stabilized within 6 months after surgery and that no
recent years as a valid diagnostic technique for the in vivo
significant differences were observed during follow-up be-
microscopic imaging of corneal structure, both in healthy
tween these values and PKP group visual acuity score.
and pathologic One of the fields of application in
However, in our patients, visual recovery was slow and
which IVCM was shown to be a potentially useful tool is
progressive, with continuous increments over time, as
that of corneal refractive In vivo confocal mi-
croscopy has been used to evaluate corneal structure and
The results of this study thus indicate that visual acuity
morphologic features in LASIK-treated Spe-
outcomes, obtained with intentional sparing of the most
cifically, IVCM has been shown to be effective in the
posterior stromal layers, are comparable with other DLKP
microscopic imaging of the LASIK flap–stroma interface,
techniques baring the DM, confirming the observation by
allowing identification of the interface layer, which is char-
Sugita and but that visual recovery requires at least
acterized by the presence of microscopic interface bright
6 to 12 months to reach satisfactory levels. Over the 12-
variable reflectivity (low to
month follow-up, we evaluated topographical parameters
and disappearance of keratocytes around the wound inter-
and interface microscopic morphologic parameters that
In addition, IVCM allowed flap thickness and
could affect visual performance over time.
residual stromal thickness measurements by using confocal
Although starting from mean postoperative values of
microscopy sequences providing light intensity profiles or
nearly 7 D, before suture adjustment, the average topo-
Z-scan graphics, through the z-axis (anteroposterior) dis-
graphic cylinder at the end of follow-up was less than 3 D
tance calculation between the identified interface layer and
after suture removal. Final astigmatism in our series was
comparable with or slightly lower than other reported data
In our study, IVCM was used to evaluate interface pa-
results obtained using and these findings
rameters (depth and reflectivity), as well as keratocyte and
confirm the efficacy of suture adjustment to control astig-
endothelial cell density over a 12-month follow-up. We also
matism occurring after as was observed for
evaluated the clinical outcome (complication rate and visual
Topographic index SRI, a measure of local fluc-
acuity) and topographic parameters that could affect visual
tuations in central corneal power, and SAI, a measure of the
results. Correlations between visual outcome and detected
differences in corneal power at every ring over the entire
topographic and confocal microscopy interface data also
cornea, evaluated at all follow-up examinations, tended to
were investigated.
decrease over time. Surface regularity index and SAI values
In our series of 46 eyes, 2 DM intraoperative ruptures
observed at 12 months corresponded to results reported in
occurred during the delamination phase. The larger rupture
other studies of and
required conversion into PKP. Two other DLKP procedures
To our knowledge, this study is the first investigation
failed after surgery because of delayed epithelial healing
reporting corneal confocal microscopic morphologic and
resulting from graft override with severe stromal inflamma-
interface features in DLKP. As previously explained for
tion and needed subsequent PKP within 5 months of the first
LASIK, IVCM allowed easy identification of the interface
surgical procedure. The eyes that underwent PKP were
layer in DLKP corneas. Deep stromal interface appeared as
excluded from data analysis. The incidence of DM split in
an atypical stromal layer characterized by discontinuity of
our group was 4%, and this frequency is consistent with the
tissue and cellular stromal architecture, absence or reduced
most favorable outcome reported in previous stud-
density of keratocytes, and variable background extracellu-
Recent reports from Watson et and from
lar reflectivity. Data obtained from averaged Z-scan inter-
Shimazaki et aldocumented a DM rupture in 15% of the
face depth measurements revealed that the mean depth
eyes treated with DLKP with DM exposure. The relatively
(distance of the interface from the endothelium) was 60 m
lower incidence of DM breaks that occurred in our study
(range, 45–74 m) 2 weeks after surgery and remained
may be related to the presence of the deepest stromal layers
unchanged over the entire follow-up period. These results
left undissected above the endothelium, which may protect
indicate a reliable depth standardization achievable with the
DM from surgical damage during the dissection phase.
technique used. This presumably suggests that significant
The logMAR UCVA and BCVA after surgery improved
processes of stromal remodeling or deep stromal rethicken-
to average values of 0.421 and 0.104, respectively, at 12
ing behind the interface do not take place in DLKP. More-
months. The logMAR BCVA was 0.2 or better in 95% of
over, in corneas that underwent surgery for keratoconus, the
eyes, and 0.1 or better in 70% of eyes at the end of follow-up.
images of residual stromal bed showed a characteristic
These findings are similar to those of other studies investigat-
presence of hyporeflexive linear striae that were
ing visual outcome after DLKP for keratoconus and other
present before surgery, which have been shown to be typical
anterior corneal pathologic As already men-
confocal microscopic features of panstromal involvement in
tioned, Sugita and Kondo, in their clinical report on DLKP
This aspect further confirms that the deep
that included 120 eyes with various corneal diseases other
stroma under the interface persists without significant mor-
than keratoconus, found that there were no differences in
phologic changes, to the extent observable by IVCM. How-
BCVA at 12 months between the 2 subgroups of patients
ever, it was reported previously that recurrent corneal ecta-
Volume 113, Number 8, August 2006
sia after DLKP for keratoconus is a rare but potential
could clarify if such scarring phenomena may affect deep
late-onset complication that may be related to donor or host
stromal interfaces at late postoperative periods. In the
and IVCM assessment of preinterface and postint-
present study, interface morphologic features at 6 and, par-
erface stromal morphologic features and thickness could
ticularly, at 12 months after surgery showed a stromal layer
improve the understanding of stromal changes in case of
with low reflectivity and lack of keratocyte cells. These
recurrent keratoconus. Interface morphologic features and
features were similar to normal LASIK interface micro-
reflectivity showed notable variations during the year of
scopic morphologic Anterior and posterior
follow-up as opposed to host residual stromal layers. Mean
stroma (behind the interface) did not show significant opaci-
interface reflectivity values were highest at 2
fication, loss of transparency of the extracellular lamellae,
weeks and 1 month and showed a continuous decrease over
or relevant keratocyte activation or inflammation. Anterior
time, reaching reflectivity levels comparable with normal
and posterior keratocyte density were within normal limits
rear stromal values at 12 months. In all cases, no (or rare)
without significant changes over the 12-month follow-up.
distinguishable keratocytes or myofibroblasts were detected
Thus, the only corneal sublayer that evidenced variations in
within the interface layers. Interface brightness apparently
transparency was the proper donor– host interface. Epithe-
was the result of extracellular diffuse and discretely homo-
lial morphologic features, nerve fiber regeneration, and but-
geneous reflectivity, compatible with edematous fluid accu-
ton stromal cellular architecture were not investigated in
mulation. This interface extracellular opacity tended to clar-
this study, but could be interesting parameters to evaluate in
ify over months demonstrating a progressive gain of
future studies to understand more thoroughly the micro-
transparency of the stroma at the interface layer. The reab-
scopic behavior of tissues in DLKP-transplanted corneas.
sorption of interface fluid is the hypothesis that best de-
By using the surgical technique presented in our study, a
scribes the reduction of interface reflectivity observed in our
certain degree of interface opacity occurring within the first
study, and apparently no visible scarring features mediated
months after surgery was a constant behavior of DLKP
by activated keratocytes or myofibroblast were found at the
wound healing and should not be considered a complica-
interface level during the follow-up period. However, further
tion. We did not observe severe or persistent interface
in vivo micromorphologic studies, with a longer follow-up,
opacity limiting the recovery of visual acuity. Also, slit-
BCVARef lectiv ity
Figure 5. Graph showing changes over the 12-month follow-up period of 2 main parameters that were correlated with best-corrected visual acuity
(BCVA), reported in logarithm of the minimum angle of resolution units. Interface reflectivity and topographic astigmatism values were reported in a log10
scale. Note that BCVA continued to improve between 3 and 12 months, whereas astigmatism appeared stable In contrast, during the same
period interface reflectivity showed a decrease, statistically significant between 3 and 6 months
Marchini et al 䡠 Deep Lamellar Keratoplasty by Intracorneal Dissection
lamp examination allowed the visualization of a mild inter-
present significant functional correlation with visual perfor-
face haziness mainly up to 3 months after surgery. How-
mance after surgery.
ever, biomicroscopic evaluation was not effective in
After the 3-month follow-up, no eyes had substantial
detecting a fine degree of opacity (at 6 months after surgery,
irregular astigmatism (severely interfering with the visual
almost all interfaces appeared clear at slit lamp) and did not
acuity), but progressive reduction of interface reflectivity
permit quantification or grading of this interface parameter
was correlated with subsequent BCVA increases up to 1
as objectively as IVCM.
year after surgery. In vivo confocal microscopy is a nonin-
Correlation analysis of visual with other measured pa-
vasive method for quantitative evaluation of interface trans-
rameters showed that interface reflectivity presents a signif-
parency in lamellar grafts that could be applied in the other
icant negative correlation with BCVA starting from 3
DLKP techniques to find possible differences.
months, when the effect of astigmatism and topographicparameters was reduced. In fact, a significant negative cor-relation was detected between UCVA and topographic
astigmatism during the entire follow-up as expected, andbetween UCVA and SRI and SAI up to 1 and 3 months,
1. Shimazaki J. The evolution of lamellar keratoplasty. Curr
respectively. As opposed to BCVA, which showed only
Opin Ophthalmol 2000;11:217–23.
slight but significant negative correlations with topographic
2. Sugita J, Kondo J. Deep lamellar keratoplasty with complete
astigmatism, SRI and SAI during the first month after sur-
removal of pathological stroma for vision improvement. Br J
gery showed significant correlations, suggesting that the
Ophthalmol 1997;81:184 – 8.
reduction of astigmatism and the amelioration of topo-
3. Saini JS, Jain AK, Sukhija J, Saroha V. Indications and
outcome of optical partial thickness lamellar keratoplasty.
graphic indexes after suture adjustment decrease the influ-
ence of these parameters on corrected visual acuity. How-
4. Richard JM, Paton D, Gasset AR. A comparison of penetrat-
ever, we detected significant correlation between BCVA
ing keratoplasty and lamellar keratoplasty in the surgical man-
and interface reflectivity only between 3 and 12 months.
agement of keratoconus. Am J Ophthalmol 1978;86:807–11.
This may indicate that interface transparency plays a role in
5. Lyons CJ, McCartney AC, Kirkness CM, et al. Granular
visual recovery, which becomes more evident when the ef-
corneal dystrophy: visual results and pattern of recurrence
fects of other influencing parameters, such as irregular astig-
after lamellar or penetrating keratoplasty. Ophthalmology
matism, have been controlled. As summarized in
average BCVA continued to increase after the stabilization of
6. Benson WH, Goosey CB, Prager TC, Goosey JD. Visual
improvement as a function of time after lamellar keratoplasty
astigmatism at 3 months, with a parallel decrease of interface
for keratoconus. Am J Ophthalmol 1993;116:207–11.
7. Shimazaki J, Shimmura S, Ishioka M, Tsubota K. Randomized
In our series, endothelial cell density showed a signifi-
clinical trial of deep lamellar keratoplasty vs penetrating ker-
cant reduction between preoperative values and those ob-
atoplasty. Am J Ophthalmol 2002;134:159 – 65.
tained 15 days after surgery (13.8% cell loss) and a further
8. Melles GR, Lander F, Rietveld FJR, et al. A new surgical
decrease between 15 days and 1 month (3.4% cell loss), but
technique for deep stromal, anterior lamellar keratoplasty. Br J
further significant decreases were not observed. These re-
sults are consistent with other studies that reported that
9. Trimarchi F, Poppi E, Klersy C, Piacentini C. Deep lamellar
keratoplasty. Ophthalmologica 2001;215:389 –93.
DLKP reduces endothelial cell density by approximately
10. Jain S, Azar DT. New lamellar keratoplasty techniques: pos-
10% at 1 by half as much as and that
terior keratoplasty and deep lamellar keratoplasty. Curr Opin
endothelial cell loss occurs principally during the first post-
Ophthalmol 2001;12:262– 8.
operative period, followed by a physiological cell decre-
11. Archila EA. Deep lamellar keratoplasty dissection of host tissue
ment Deep lamellar keratoplasty induces a lower
with intrastromal air injection. Cornea 1984 – 85;3:217– 8.
postoperative endothelial cell loss, does not lead to an
12. Price FW Jr. Air lamellar keratoplasty. Refract Corneal Surg
accelerated endothelial decrement, and theoretically is free
1989;5:240 –3.
from endothelial rejection, thus presenting the advantage
13. Chau GK, Dilly SA, Sheard CE, Rostron CK. Deep lamellar
of lower risk of graft failure resulting from endothelial
keratoplasty on air with lyophilized tissue. Br J Ophthalmol1992;76:646 –50.
14. Amayem AF, Anwar M. Fluid lamellar keratoplasty in kera-
In conclusion, our study documented that morphologic
toconus. Ophthalmology 2000;107:76 –9, discussion 80.
characteristics of the donor– host interface after DLKP, as-
15. Manche EE, Holland GN, Maloney RK. Deep lamellar kera-
sessed by means of IVCM, present significant functional
toplasty using viscoelastic dissection. Arch Ophthalmol 1999;
correlation with visual performance after surgery.
Deep lamellar keratoplasty by intracorneal dissection, in
16. Anwar M, Teichmann KD. Big-bubble technique to bare De-
our series, resulted in a good visual improvement, compa-
scemet's membrane in anterior lamellar keratoplasty. J Cata-
rable with PKP or other DLKP techniques, and presented a
ract Refract Surg 2002;28:398 – 403.
17. Panda A, Bageshwar LM, Ray M, et al. Deep lamellar kera-
limited incidence of intraoperative complications (DM rup-
toplasty versus penetrating keratoplasty for corneal lesions.
ture). Visual recovery takes several months, and astigmatism
and interface transparency are the main factors involved. Our
18. Watson SL, Ramsay A, Dart JK, et al. Comparison of deep
study documented that morphologic characteristics of the
lamellar keratoplasty and penetrating keratoplasty in patients
donor– host interface after DLKP, assessed by IVCM,
with keratoconus. Ophthalmology 2004;111:1676 – 82.
Volume 113, Number 8, August 2006
19. Hirano K, Sugita J, Kobayashi M. Separation of corneal
29. Javaloy Estan J, Vidal MT, Quinto A, et al. Quality assess-
stroma and Descemet's membrane during deep lamellar ker-
ment model of 3 different microkeratomes through confocal
atoplasty. Cornea 2002;21:196 –9.
microscopy. J Cataract Refract Surg 2004;30:1300 –9.
20. Anwar M, Teichmann KD. Deep lamellar keratoplasty: surgical
30. Tsubota K, Kaido M, Monden Y, et al. A new surgical
techniques for anterior lamellar keratoplasty with and without
technique for deep lamellar keratoplasty with single running
baring of Descemet's membrane. Cornea 2002;21:374 – 83.
suture adjustment. Am J Ophthalmol 1998;126:1– 8.
21. Jalbert I, Stapleton F, Papas E, et al. In vivo confocal micros-
31. Karabatsas CH, Cook SD, Figueiredo FC, et al. Combined
copy of the human cornea. Br J Ophthalmol 2003;87:225–36.
interrupted and continuous versus single continuous adjust-
22. Tervo T, Moilanen J. In vivo confocal microscopy for evalu-
able suturing in penetrating keratoplasty: a prospective, ran-
ation of wound healing following corneal refractive surgery.
domized study of induced astigmatism during the first post-
Prog Retin Eye Res 2003;22:339 –58.
operative year. Ophthalmology 1998;105:1991– 8.
23. Avunduk AM, Senft CJ, Emerah S, et al. Corneal healing after
32. Shimazaki J, Shimmura S, Tsubota K. Intraoperative versus
uncomplicated LASIK and its relationship to refractive
postoperative suture adjustment after penetrating keratoplasty.
changes: a six-month prospective confocal study. Invest Oph-
Cornea 1998;17:590 – 4.
thalmol Vis Sci 2004;45:1334 –9.
33. Seitz B, Langenbucher A, Kuchle M, Naumann GO. Impact of
24. Dawson DG, Holley GP, Geroski DH, et al. Ex vivo confocal
graft diameter on corneal power and the regularity of postk-
microscopy of human LASIK corneas with histologic and
eratoplasty astigmatism before and after suture removal. Oph-
ultrastructural correlation. Ophthalmology 2005;112:634 – 44.
25. Perez-Gomez I, Efron N. Confocal microscopic evaluation of
particles at the corneal flap interface after myopic laser in situ
34. Hollingsworth JG, Efron N. Observations of banding patterns
keratomileusis. J Cataract Refract Surg 2003;29:1373–7.
(Vogt striae) in keratoconus: a confocal microscopy study.
26. Erie JC, Hodge DO, Bourne WM. Confocal microscopy eval-
Cornea 2005;24:162– 6.
uation of stromal ablation depth after myopic laser in situ
35. Patel N, Mearza A, Rostron CK, Chow J. Corneal ectasia
keratomileusis and photorefractive keratectomy. J Cataract
following deep lamellar keratoplasty [letter]. Br J Ophthalmol
Refract Surg 2004;30:321–5.
2003;87:799 – 800.
27. Vesaluoma M, Perez-Santonja J, Petroll WM, et al. Corneal
36. Van Dooren BT, Mulder PG, Nieuwendaal CP, et al. Endo-
stromal changes induced by myopic LASIK. Invest Ophthalmol
thelial cell density after deep anterior lamellar keratoplasty
Vis Sci 2000;41:369 –76.
(Melles technique). Am J Ophthalmol 2004;137:397– 400.
28. Erie JC, Nau CB, McLaren JW, et al. Long-term keratocyte
37. Morris E, Kirwan JF, Sujatha S, Rostron CK. Corneal endo-
deficits in the corneal stroma after LASIK. Ophthalmology
thelial specular microscopy following deep lamellar kerato-
2004;111:1356 – 61.
plasty with lyophilised tissue. Eye 1998;12:619 –22.
Source: http://www.innovamed.ru/var/files/articles/DLKP.pdf
International Journal of Oral & Maxillofacial Pathology. 2012;3(3):56-60 ISSN 2231 – 2250 Available online at http://www.journalgateway.com or www.ijomp.org Case Report Intraosseous Transmigration of Impacted Canines: Report of Five Cases Sulabha AN, Sachin Deshpande, Sameer C Abstract Transmigration is rare and unusual anomaly involving the intraosseous migration of impacted tooth across midline regardless of the distance. This occurs almost exclusively with mandibular canines. Etiology is still unclear and is not well documented in the literature. Transmigration can occur as isolated finding or in association with other findings such as dentigerous cyst, odontomas, impactions of other teeth etc. Transmigrated canines are particularly significant due to aesthetic and functional importance. Early radiographic examination of the patient is important for the treatment. More documentation of this anomaly and future studies may lead to a better understanding of this rare anomaly, its etiology and improvement of the classification criteria. This paper presents five cases of transmigration of mandibular canines of which two were associated with dentigerous cyst, one associated with bodily rotation of canine, one associated with absence of third molars on right side. Keywords: Impacted Canine;Tooth Migration;Transmigration;Intraosseous;Dentigerous Cyst; Observation. Sulabha AN, Sachin Deshpande, Sameer C. Intraosseous Transmigration of Impacted Canines: Report of Five Cases. International Journal of Oral and Maxillofacial Pathology; 2012:3(3):56-60. ©International Journal of Oral and Maxillofacial Pathology. Published by Publishing Division, Celesta Software Private Limited. All Rights Reserved.
C H A P T E R 3 3-D US Imaging of the Carotid Arteries Aaron Fenster, Grace Parraga, Anthony Landry, Bernard Chiu, Michaela Egger,and J. David Spence Determining the severity of carotid atherosclerotic stenosis has been an importantstep in establishing patient management pathways and identifying patients who canbenefit from carotid endarterectomy versus those who should be treated using life-style and pharmaceutical interventions. Recently a number of research groups havedeveloped phenotypes other than carotid stenosis using noninvasive imaging. Mon-itoring carotid plaque progression/regression and identifying vulnerable orhigh-risk plaques that can lead to thrombogenic events using noninvasive imagingtools now involve multiple disciplines and multiple modalities, including imageprocessing.