Macrovascular complications (doctor)
Steno Diabetes Center – Courses in Clinical Diabetes Care
Table of Contents
Copyright Steno Diabetes Center 2016
Chapter 8: Macrovascular Complications
Chapter 8: Macrovascular Complications
The aim of this chapter is to enable non-specialist doctors to prevent, diagnose and provideappropriate management (including specialist referral where appropriate) for macrovascularcomplications (stroke, ischaemic heart disease, and peripheral vascular disease). The doctorshould be able to apply an evidence-based approach to prevent (through management ofcardiovascular risk factors, including hypertension, dyslipidaemia and smoking), screen andrefer for macrovascular complications, in accordance with appropriate national clinical prac-tice guidelines. The chapter is intended to help foster a multidisciplinary team approach to theprevention, screening, diagnosis and management of macrovascular complications, includingeducation and empowerment of the patient and/or the patient's carer, to prevent, detect andmanage macrovascular diabetes-related complications.
After completing this chapter, learners should be able to:
• Identify risk factors for stroke, ischaemic heart disease and peripheral vascular disease
in clinical practice.
• Understand the rationale for individualised treatment targets for people with diabetes.
• Understand the need for treating dyslipidaemia and hypertension to prevent macrovas-
• Describe local resources available to guide therapeutic decisions.
• Appreciate the importance of screening to enable the prevention and timely treatment
of macrovascular complications.
• Appreciate the psychosocial implications of diabetes complications.
• Value a team-based approach to the prevention and management of chronic macrovas-
• Assess cardiovascular risk for the individual patient.
• Assess patients for symptoms of cardiovascular disease using simple clinical criteria,
whilst recognising the limitations of this approach.
• Appropriately treat patients to reduce risk of macrovascular complications according to
international and national guidelines, in collaboration with the patient.
• Recognise the patients for whom very strict glycaemic and blood pressure control is
Copyright Steno Diabetes Center 2016
Steno Diabetes Center – Courses in Clinical Diabetes Care
• Discuss the risk of non-adherence to treatment with patients.
• Appropriately refer patients with macrovascular complications for specialist investiga-
tion and treatment, according to national guidelines.
• Provide patients with appropriate treatment options to prevent macrovascular compli-
cations, based on the patient's individual risk profile, and in collaboration with the pa-tient.
Copyright Steno Diabetes Center 2016

Ulla Bjerre-Christensen - Head of Education and Chief Physician at Steno Diabetes Center
The content is available online (see https://macrovascularcompdoctor.ibog.steno.dk/
index.php?id=592)
Macrovascular disease is a disease affecting the large (macro) blood vessels in the body, in-cluding the coronary arteries and the principal arteries in the brain and limbs. The centralpathological mechanism in macrovascular disease is the process of atherosclerosis, whichleads to a the narrowing of arterial walls throughout the body Fowler M 2008, resulting inthe cardiovascular complications of diabetes. Cardiovascular disease (CVD) is the major causeof morbidity and mortality for individuals with diabetes and is a large contributor to the di-rect and indirect costs of diabetes. The primary focus is on ischaemic heart disease, strokeand peripheral vascular disease, which are primary endpoints in many CVD outcome stud-ies Emerging Risk Factors Collaboration et al 2011. It is important also not to forget heartfailure, which is a frequent, fatal and often overlooked complication.
Some common conditions that coexist with type 2 diabetes (e.g. lack of physical activity, hy-pertension and dyslipidaemia) are clear risk factors for CVD, and diabetes itself confers anindependent risk. For patients with type 1 or type 2 diabetes, the presence of microvascular
Copyright Steno Diabetes Center 2016
Steno Diabetes Center – Courses in Clinical Diabetes Care
complications indicates an increased risk for CVD. Numerous studies have shown the efficacyof controlling individual cardiovascular risk factors for preventing or slowing the progress ofCVD in people with diabetes. Large benefits result when multiple risk factors are addressedsimultaneously Gaede P et al 2008. There is some evidence that the 10-year risk of coronaryheart disease (CHD) among adults with diabetes in USA has been significantly reduced overthe past decade Ali MK et al 2013.
As most of the risk factors are silent, regular screening for risk factors in patients with dia-betes in a structured way is necessary, and intervention should be aggressive. Furthermore,symptoms can be non-specific, so a high degree of suspicion and a low threshold for referralto a specialist for further investigation is necessary. This chapter wil discuss the risk factorsfor, intervention for, and referrals needed to manage CVD, in accordance with the Ameri-can Diabetes Association guidelines for treatment of diabetes American Diabetes Association2015.
Copyright Steno Diabetes Center 2016
Lesson 1: Cardiovacular Risk Factors in Type 2 Diabetes
Lesson 1: Cardiovacular Risk Factors in
Type 2 Diabetes
Whereas people with uncomplicated type 1 diabetes are considered to have a risk for CVDthat is almost comparable to that of the background population, the presence of microvas-cular complications – in particular diabetic nephropathy or retinopathy – in such people isindicative of an increased CVD risk, such that aggressive intervention against modifiable riskfactors is required. In contrast, most type 2 diabetes patients have other coexisting risk fac-tors for CVD that tend to cluster in patients including: abdominal obesity, high levels of serumtriglycerides, low levels of high-density lipoprotein- (HDL) cholesterol, elevated blood pres-sure, and high fasting glucose levels – which are known collectively as the metabolic syn-drome Alberti KG 2009.
Common risk factors for CVD among people with diabetes include:
• Hypertension• Dyslipidaemia (elevated low-density lipoprotein- [LDL-] cholesterol,
low HDL-cholesterol, elevated triglycerides)
• Smoking• Elevated urinary albumin excretion• Poor glycaemic control• Age
These factors are considered in the sections below.
Hypertension is common among people with diabetes, particularly those with type 2 diabetes.
Its prevalence increases with age and obesity and also depends on ethnicity. As well as beinga major CVD risk factor, it is also a risk factor for microvascular complications. In type 1 dia-betes, the prevalence of essential hypertension (hypertension without a specific, identifiablecause) has a similar to that of the background population, while hypertension in this popula-tion may also occur as a consequence of diabetic kidney disease (diabetic nephropathy).
Blood pressure (BP) should be measured using an appropriately sized cuff at every visit to thediabetes outpatient clinic, for which the patient should be in a seated position, having restedfor at least 5 minutes Handler J 2009. There are several factors can affect BP measurement(Tables 1–2) Campell NR and McKay DW 1999.
Copyright Steno Diabetes Center 2016
Steno Diabetes Center – Courses in Clinical Diabetes Care
Table 1
Factors that may influence BP measurement
Copyright Steno Diabetes Center 2016
Lesson 1: Cardiovacular Risk Factors in Type 2 Diabetes
Table 2
Changes, relative to normal blood pressure, that occur with different activities.
Source: Campbell et al. 1999 [8]
A phenomenon known as 'white-coat hypertension' – where BP is elevated when measuredin an office or clinical setting, but is normal outside of this – is seen in up to 25% of somesubjects with high BP. Conversely, 'masked hypertension' – where BP is normal in an office/clinical setting but is elevated when 'out-of-office' – occurs in around 10%. Table 3 shows across-comparison of ‘office' and ‘out-of-office' blood pressure measurements.
Out-of-office measurements have been found to correlate better with CVD outcome than of-fice measurements Hansen TW et al 2005. Any measurements of elevated BP should be con-firmed on a separate occasion. When discrepancies between BP measurements occur, homeblood-pressure monitoring or 24-hour ambulatory blood pressure measurements should alsobe considered if clinically indicated.
Out of office BP
Office Normal True Normotension Masked HT
Elevated White-coat HT
Copyright Steno Diabetes Center 2016
Steno Diabetes Center – Courses in Clinical Diabetes Care
1.2.3. Treatment Targets
Epidemiological analyses have shown that blood pressure levels >115/75 mmHg are asso-ciated with increased cardiovascular event rates and mortality in individuals with diabetes,whereas lower blood pressure levels have also been associated with increased risk ArguedasJa et al 2013 Bangalore S et al 2010. The optimal treatment target is a matter of debate,mostly because of the lack of clinical trials in which patients have been randomised to differ-ent blood pressure levels.
Clinical trials have demonstrated the benefit of lowering blood pressure to <140 mmHg sys-tolic BP and <90 mmHg diastolic BP in individuals with diabetes – namely, the reduction ofcoronary heart disease (CHD) events, stroke, and diabetic kidney disease. It is not clear iflower targets are of benefit. A meta-analysis of randomised trials of adults with type 2 di-abetes that compared intensive blood-pressure targets (upper limit of 130 mmHg systolicand 80 mmHg diastolic BP) to standard targets (upper limit of 140–160 mmHg systolic and85–100 mmHg diastolic BP) found no significant reduction in mortality or non-fatal myocar-dial infarction (MI), but a 35% relative risk reduction in stroke McBrien K et al 2012.
The ACCORD trial examined whether a comparatively lower systolic BP of <120 mmHg, inpatients with type 2 diabetes at high risk for CVD, provided greater cardiovascular protectionthan a systolic BP of 130–140 mmHg ACCORD Study Group et al 2010. The results indicatedthere was no benefit in regard to the primary endpoint (a composite of non-fatal MI, non-fatalstroke, and cardiovascular death), but that there was a significant reduction in the incidenceof stroke.
Currently, most guidelines specify a target systolic BP <140 mmHg or <130 mmHg if stroke orchronic kidney disease is a concern, and if the patient can tolerate the lower blood pressure.
Similarly, diastolic BP should be <90 mmHg although, for some, <80mmHg may be more ap-propriate if tolerated American Diabetes Association 2015.
Copyright Steno Diabetes Center 2016
Lesson 1: Cardiovacular Risk Factors in Type 2 Diabetes
Figure 1
Treatment targets for Blood Pressure
Lifestyle modification consists of restricting sodium intake (<2.3 g/day); reducing excess bodyweight; increasing consumption of fruits, vegetables (8–10 servings per day) and low-fatdairy products (2–3 servings per day); reducing alcohol intake; increasing activity levels; andstopping smoking. If BP is confirmed as ≥140/≥90 mmHg, pharmacological therapy shouldbe initiated, along with lifestyle modification.
Copyright Steno Diabetes Center 2016
Steno Diabetes Center – Courses in Clinical Diabetes Care
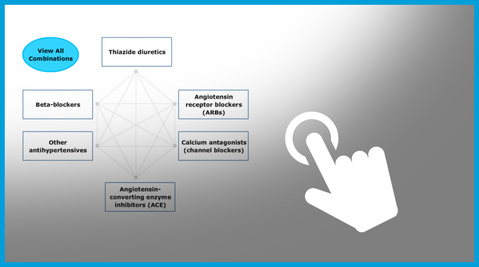
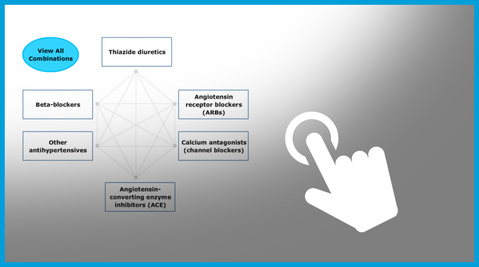
Regimens based on a variety of antihypertensive agents – including angiotensin-convertingenzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), beta blockers, diuretics andcalcium-channel blockers – have been shown to be effective in reducing cardiovascularevents James PA et al 2014. In most patients, combination therapy is needed. Inhibitors ofthe renin–angiotensin system are recommended as first choice, and combination with diuret-ics are often needed to control oedema and blood pressure. ACE inhibitors and ARBs are con-sidered renoprotective, and an ACE inhibitor was shown to have reduced CVD outcomes in atrial of individuals at high risk for CVD, including a large subset with diabetes Estacio RO etal 1998. Figure 1 illustrates some possible combinations of treatment. If needed, amlodipine,metoprolol or thiazide can be added to achieve blood-pressure targets James PA et al 2014.
If the glomerular filtration rate (GFR) is <30 ml/min/1.73 m2, a loop diuretic, rather than athiazide, should be prescribed.
To learn more about the possible combinations of antihypertensive drugs, navigate throughthe interactive graphic below.
Identifying and addressing the barriers to medication adherence (such as cost and side ef-fects) should be a routine practice. If blood pressure remains uncontrolled – i.e. despite con-firmed adherence to optimal doses of at least three antihypertensive agents of different clas-sifications, one of which should be a diuretic – clinicians should consider an evaluation forsecondary forms of hypertension James PA et al 2014.
Copyright Steno Diabetes Center 2016
Lesson 1: Cardiovacular Risk Factors in Type 2 Diabetes
Dyslipidaemia is prevalent in diabetes, so screening to establish the patient's lipid profile isrecommended at diagnosis and at age 40 years (or from the onset of microvascular compli-cations), and periodically thereafter, every 1–2 years.
An increasing LDL-cholesterol level is clearly associated with an increasing cardiovascular risk,and outcomes have been shown to be improved if levels are lowered Kearney Pm et al 2008.
Cardiovascular risk is also increased if HDL-cholesterol levels are reduced or if triglyceride lev-els are increased. Severe hypertriglyceridaemia may carry additional risks (e.g. pancreatitis).
Interventions that reduce triglyceride levels have not been shown to improve cardiovascularoutcomes Boden WE et al 2011 Hovingh GK et al 2015. Therefore, LDL-cholesterol is the pri-mary target of lipid-lowering therapy.
Lifestyle modification focuses on the reduction of saturated fat, trans fat and cholesterol in-take, as well as an increased intake of omega-3 fatty acids and viscous fibre, combined withweight loss (if indicated). An increased physical activity should be recommended to help im-prove the lipid profile, and glycaemic control should be optimised WING PR et al 2013.
In type 2 diabetes, treatment with statins reduces CVD both as primary and secondary pre-vention. In type 1 diabetes, the evidence is weaker, but suggests that the benefit is simi-lar Collins R et al 2003, and treatment is recommended in patients with CVD risk factors, andparticularly if microvascular complications are present.
A meta-analyses – including data from the Cholesterol Trialists' study, which included morethan 18,000 patients with diabetes from 14 randomised trials of statin therapy – have demon-strated a 9% reduction in all-cause mortality and a 13% reduction in vascular mortality foreach mmol/l reduction in LDL-cholesterol Kearney Pm et al 2008.
Because most studies have compared statins to placebo, or different doses, rather than incor-porating specific targets, it has been debated whether specific LDL-cholesterol targets shouldbe recommended, or rather a dose-related strategy, using moderate or low intensity statintreatment depending on level of CVD risk. In many cases, an LDL-cholesterol target of <2.6mmol/l (100 mg/dl) in diabetes with CVD risk factors is recommended (as primary preven-tion), and a target of 1.8 mmol/l (70 mg/dl) in patients with diabetes and CVD (as secondaryprevention).
Copyright Steno Diabetes Center 2016
Steno Diabetes Center – Courses in Clinical Diabetes Care
An alternative recommendation that has been suggested is to use a moderate-intensity statinin a dose that reduces LDL-cholesterol by 30–50% (e.g. atorvastatin 10 mg; rosuvastatin 10mg; simvastatin 20–40 mg; pravastatin 40 mg) for primary prevention, and a high-intensitystatin in a dose that reduces LDL-cholesterol by approximately 50% or more (e.g. atorvas-tatin 40–80 mg or rosuvastatin 20 mg) for secondary prevention Stone NJ et al 2014.
Watch the video to learn more about statin therapies for people with diabetes when CVD isabsent.
The content is available online (see https://macrovascularcompdoctor.ibog.steno.dk/
index.php?id=593)
Click on the graphic below to learn more about statin therapies for people with diabetes whenCVD is absent (Table 4) or present (Table 5).
Copyright Steno Diabetes Center 2016
Lesson 1: Cardiovacular Risk Factors in Type 2 Diabetes
ACC and AHA Guidelines
Age 40-75
Age > 75
10 year CV risk <
10-year CV risk ≥
High inten- High intensity*
Moderate intensi-
Source: Stone et al 2014 [22].
Age 21-74
Age > 75
High intensity* Moderate** or high intensity*
High intensity* Moderate** or high intensity*
High intensity* Moderate** or high intensity*
Source: Stone et al 2014 [22]
Although supportive data are weak, the addition of lipid-lowering agents (for example ezetim-ibe) other than statins has been suggested if statins are not tolerated, or are insufficient toreach the desired target, or particularly in those patients with severely elevated triglycerides(where fibrates are recommended to prevent pancreatitis). The effect of fibrates on CVD hasbeen disappointing Keech A et al 2005, although, in contrast, it has been suggested that fi-brates may have an effect on diabetic retinopathy Chew EY et al 2014.
The role of a new and very potent cholesterol-lowering treatment – comprising injectablemonoclonal antibodies known as PCSK9 (proprotein convertase subtilisin-kexin type 9) inhi-bitors – in patients with diabetes has not yet been clarified Sabatine MS et al 2015.
1.4 Smoking
Smoking is a strong yet modifiable risk factor for CVD, both for people with and without dia-betes. Compared with other modifiable risk factors, successful cessation of smoking has thesingle largest effect on cardiovascular mortality Yudkin JS et al 1993. The number of cig-
Copyright Steno Diabetes Center 2016
Steno Diabetes Center – Courses in Clinical Diabetes Care
arettes smoked, the duration of smoking, and the number of years since cessation are allassociated with mortality Al-delaimy WK et al 2002 Chaturvedi N et al 1997. Therefore, alldiabetes patients who smoke should be advised to stop as soon as possible and be given ap-propriate support.
The persistent excretion of albumin in the urine at a rate greater than 30 mg/24 hours isa high-risk marker for CVD in patients with diabetes. Diagnosis of albuminuria requires thedemonstration of an elevated albumin level (indicated by albumin to creatinine ratio) from aspot urine test or a timed collection (for example over 24 hours). Two positive samples, froma total of three tests, collected over a 3–6-month period, are recommended for diagnosis.
Dipstick urine testing for albumin has a high rate of false-negative and false-positive results,so is not recommended for the purpose of diagnosis. Estimation of GFR may be used, in ad-dition, to estimate renal function and determine chronic kidney disease stage, but does notreplace the assessment of urinary albumin status. Treatment of hypertension with an ACEinhibitor or ARB as a first-line agent has been shown to improve cardiovascular outcomesJames PA et al 2014.
1.6 Antiplatelet Therapy
Antiplatelet therapy is another important aspect of cardiovascular risk reduction that shouldbe addressed. It has been widely shown to be effective as secondary prevention. A recentmeta-analysis demonstrated an 18% reduction in serious cardiovascular events in patientswith CVD taking aspirin Baigent C et al 2009. However, although the benefit as secondaryprevention has been well established, the benefit with regard to primary prevention is lessclear, and the risk of side effects must be taken into account. Antiplatelet therapy with aspirin(acetyl salicylic acid) 75–150 mg /day is recommended as secondary prevention of CVD or, ifaspirin is not tolerated, clopidogrel 75 mg/day. In patients with CVD risk factors but withoutprevious CVD (i.e. for primary prevention), aspirin should be considered if the CVD risk is high(>10% in 10 years), which would correspond to men over 50 years of age, or women over60 years, with additional risk factors Baigent C et al 2009 Pignone M et al 2010. However, insubjects with a low 10-year CV risk (<5%), the risk of bleeding is probably larger than thebenefit.
Copyright Steno Diabetes Center 2016

Lesson 1: Cardiovacular Risk Factors in Type 2 Diabetes
1.7 Glycaemic Control
Whereas several studies have demonstrated an epidemiological association between poor gly-caemic control and an increased risk of CVD Anand SS et al 2012 Stratton IM et al 2000,studies that have investigated the potential of lowering glucose intensively – such as AC-CORD, ADVANCE and VADT – have not convincingly been able to show a benefit, in regard toCVD risk Skyler JS et al 2009; indeed, an increased mortality rate was found in the ACCORDstudy. It has been suggested that this lack of benefit could be due to the adverse effectsof treatment (such as hypoglycaemia, weight gain, or other factors), although this remainsunresolved. It is necessary, therefore, to individualise the glycaemic target according to thepatient's characteristics. Consequently, the target wil be comparatively less stringent for el-derly patients with multiple comorbidities and a high risk for hypoglycaemia, and compara-tively more stringent in younger patients with a short duration of diabetes.
Activate the animation below to learn more about individualising treatment targets on thebasis of patient characteristics.
The content is available online (see https://macrovascularcompdoctor.ibog.steno.dk/
index.php?id=593)
Copyright Steno Diabetes Center 2016
Steno Diabetes Center – Courses in Clinical Diabetes Care
The relationship between glycaemic control, as measured by HbA1c, and risk of macrovascu-lar disease is in contrast to the well-established role of lowering HbA1c in the prevention ofmicrovascular complications. The role of glucose lowering in preventing cardiovascular com-plications in type 2 diabetes was shown in the United Kingdom Prospective Diabetes Study(UKPDS), but this effect was not evident until much later, when the 10-year follow-up re-vealed that the group initially randomised to receive intensive treatment had a lower inci-dence of macrovascular disease Holman PR et al 2008.
Copyright Steno Diabetes Center 2016
Lesson 1: Cardiovacular Risk Factors in Type 2 Diabetes
Figure 3
The Role of Lowering Glucose in CVD Prevention
On the basis of the UKPDS study UK Prospecetive Diabetest Study Group 1998, metformin isregarded as the most appropriate initial pharmacological intervention to be added to lifestylemodification for the treatment of hyperglycaemia in type 2 diabetes, because of its the effect
Copyright Steno Diabetes Center 2016
Steno Diabetes Center – Courses in Clinical Diabetes Care
on CVD and glucose. The data suggest that intensive treatment with metformin results infewer MIs, compared with conventional glucose control, over the same time period.
Figure 4
Mycardial Infarction Hazard Ratio
Most major guidelines describe many different therapeutic options for second-line interven-tion if metformin is inadequate, but although interesting experimental and clinical data havebeen presented, it is not clear if any such intervention has specific CVD benefits.
Copyright Steno Diabetes Center 2016
Lesson 1: Cardiovacular Risk Factors in Type 2 Diabetes
The sodium-glucose co-transporter 2 (SGLT2) inhibitor empagliflozin was found to have apositive effect on the primary composite cardiovascular outcome Zinman B et al 2015, – whichincluded cardiovascular death, MI and stroke (Figure 5). The results showed that the deathrate from cardiovascular causes in type 2 diabetes patients with previous overt CVD was re-duced in the patient group receiving empagliflozin, compared with the control group (38%relative risk reduction). The effect was particularly related to the prevention of heart failure,whereas the risk of stroke and MI was not reduced. It is currently not known if this representsa class effect or a drug effect, nor whether it relates to type 2 diabetes patients without CVD.
Figure 5
Effect of Empagliflozin on Composite Cardiovascular Outcomes
Copyright Steno Diabetes Center 2016
Steno Diabetes Center – Courses in Clinical Diabetes Care
Lesson 2: Cardiovascular Disease
Screening and Management
Although CVD is frequently present in type 2 diabetes, regular screening for CVD is not rec-ommended, as long as the risk factors are being treated, because no benefit from suchscreening has been demonstrated Frye RL et al 2008. The use of screening is intuitively log-ical, because many type 2 patients have silent ischaemic lesions, but this relates, in part, tothe lack of a sensitive, specific, feasible and cost-effective screening method. Thus, rigorous,structured screening for CVD risk factors is mandatory, but regular screening with tests forCVD itself is not. The use of a risk calculator or ‘risk engine' – in which patient risk factorsare entered and an estimated 5- or 10-year risk generated – provides an easy approach forthis. Many examples of risk engines are available online, such as the one developed from theUKPDS Pignone M et al 2010. It should be noted, however, that these have been derived andvalidated mainly in populations of European or North American origin, and the risk may differin populations from outside these regions.
2.2 Screening Tests
In patients with diabetes, a low threshold for referral for further investigations is required,given the frequent lack of typical symptoms of ischaemia among such patients, despite thepresence of significant ischaemic disease, and the often non-specific symptoms like dysp-noea or fatigue related to exercise. It is recommended that patients with typical or atypicalsymptoms, or an abnormal resting electrocardiogram, are referred for further invasive inves-tigations. Beyond this, the topic of screening for CVD (as opposed to screening for risk fac-tors) in patients with diabetes is a controversial one. Several options have been proposed forthe purpose of screening to determine which patients should be referred for further invasivetests; these include stress testing, myocardial scintigraphy, coronary artery calcium scoring,computed tomography (CT) angiography and biomarkers. However, given the invasive natureof these tests – which have not yet proven beneficial or safe – and the high cost associatedwith some of the testing modalities, no particular screening method has been recommendedfor the diabetes patients who are without symptoms or signs of cardiovascular disease.
Copyright Steno Diabetes Center 2016
Lesson 2: Cardiovascular Disease Screening and Management
Figure 6
Recommendations for referring patients for further tests for cardiovascular disease
2.3 Treatment of Established Coronary Artery Disease
For the treatment of established CVD in patients with diabetes, and acute or chronic is-chaemic lesions and complex multi-vessel disease, coronary artery bypass grafting (CABG) ispreferred to percutaneous coronary intervention (PCI). Otherwise, treatment is the same asfor patients without diabetes, although more aggressive risk-factor management is indicated.
In general, for patients with established CVD and diabetes, treatment of risk factors shouldbe in accordance with what has been outlined in the preceding sections – namely, treatmentwith statins; antiplatelet therapy; and blood pressure control, including treatment with anACE inhibitor or ARB and mineralocorticoid receptor antagonist in case of heart failure, aswell as a beta blocker for at least 2 years after an MI. In patients with type 2 diabetes, therecent EMPA-REG study suggests that SGLT2 inhibition is also beneficial.
Copyright Steno Diabetes Center 2016
Steno Diabetes Center – Courses in Clinical Diabetes Care
Lesson 3: Multifactorial Approach to
Cardiovascular Disease
The benefits of a treatment strategy that comprises aggressive management of multiple car-diovascular risk factors simultaneously (i.e. a multifactorial approach) were demonstrated inthe Steno 2 study Gaede P et al 2008 Gaede P et al 2003. This study investigated a groupof patients at high risk of CVD, and compared the intensive management of risk factors (tar-geting lower lipid levels and HbA1c, with blood pressure control using ACE inhibitors), withthe standard treatment targets that were current at that time. Patients also received adviceregarding diet and exercise and smoking cessation and were prescribed antiplatelet therapy.
After 7.8 years of follow-up, there was a reduction in a composite endpoint of CVD and anabsolute reduction of 20% in the primary endpoint in the intensively treated group, comparedwith the standard treatment group. At the end of the study, all participants were followed upby their GP.
They were again followed up at 13 years from study entry and, despite very similar risk-factorprofiles at this point in both groups and there was stil a significant difference in outcomes.
There was a 20% absolute reduction in mortality in the intensively treated group, comparedwith the standard treatment group, indicating that treatment of five patients is needed toprevent one death. Half of the group receiving standard treatment had died at the 13-yearfollow-up (Figure 7). After 13 years there had been fewer CVD deaths within the multifactorialtreatment group (intensive therapy) compared with the conventional therapy group Gaede Pet al 2008. These findings demonstrate the clear benefit of targeting multiple CVD risk factorssimultaneously, and the importance of starting treatment as early as possible.
The content is available online (see https://macrovascularcompdoctor.ibog.steno.dk/
index.php?id=595)
3.2 Patient Engagement in Multifactorial Risk-factor Management
A multifactorial approach to managing the risks associated with CVD implies that patientsand providers are well equipped to manage a complicated medication regimen in conjunctionwith lifestyle modifications. For many patients, managing the complexities of a multi-therapystrategy can be a challenge, for a variety of reasons.
Copyright Steno Diabetes Center 2016
Lesson 3: Multifactorial Approach to Cardiovascular Disease
Several classes of factors related to adherence to long-term medication regimens have beenidentified, including Ickovics JR et al 1997 Haynes RB et al 2002 Dunbar-Jacob J et al 2003Yiannakopoulou E Ch et al 2005:
• Patient Factors – These include age, physical and cognitive capacity, illness percep-
tion, health literacy, and mental health.
• Socioeconomic Factors – These include social support, social stigma, and socioeco-
nomic status.
• Therapy Factors – These include patient friendliness of the regimen, adverse effects,
drug effectiveness, drug type, shapes and sizes of tablets, and duration of treatment.
• Disease Factors – These include symptom prominence, disease severity, duration of
the disease, and clinical improvement.
• Health Care Delivery Factors – These include wait times for appointments or med-
ications, drug supply, HCP relationship, and barriers to accessing care.
3.2.2 Assisting Patients with the Medication Management Process
HCPs can undertake a number of steps to assist patients who are receiving multiple drugtherapy regimens in managing the medication process. Depending on the individual charac-teristics of the patient, these steps may include Marek KD and Antle L 2008:
• Completing a medication reconciliation• Determining ability to procure medication• Ensuring patients have sufficient medication knowledge• Evaluating physical ability• Assessing cognitive capacity• Identifying intentional non-adherence• Conducting ongoing monitoring
To learn more about medication management, navigate through the interactive graphic be-low.
Copyright Steno Diabetes Center 2016

Steno Diabetes Center – Courses in Clinical Diabetes Care
This may not be necessary for all patients, but becomes important as patients ageand their treatment for comorbid conditions increases. Data suggest that prescribingproviders are often unaware of the prescribed medications that patients are taking BaratI et al 2001 Bonner CJ and Carr B 2002 Fineman B and DeFelice C 1992 Torrible SJ andHogan DB 1997. Multiple studies have demonstrated that 10–74% of medications pre-scribed for older adults are inappropriate Aparasu PR and Sitzman SJ 1999 Bloom JA etal 1993 Zhan C et al 2001. A medical reconciliation session may help simplify a patient'sdrug regimen and prevent potentially adverse drug interactions. Over-the-counter (OTC)medication and traditional medicine use should also be assessed during this step.
Copyright Steno Diabetes Center 2016
Lesson 3: Multifactorial Approach to Cardiovascular Disease
Not fil ing or refil ing prescriptions is a common cause of medication non-adherence.
There are a variety of reasons that people omit to procure their necessary medications,but cost is often a cause. Chronically il adults are more likely to experience the financialburdens associated with covering out-of-pocket costs for their prescription medicines,and therefore cut back on medications and use fewer medicines per month than areprescribed Heisler M et al 2004 Piettet JD et al 2004 Mojtabai R and Olfson M 2003. Asimple question or two about how a patient procures their medication may provide someinsight into any financial or logistical barriers that a patient may be experiencing, andprovide an opportunity to discuss possible responses to these barriers. For instance, tryasking:
• "Please tell me a little about how and where you obtain and refill prescriptions?"• "How do you typically pay for medications?"• "Do you ever miss medication doses due to lack of money?"
Patient education is a key intervention to assist patients with medication management.
The patient's knowledge of drugs is positively associated with adherence Amsten JH et al1997 Yilmaz MB et al 2005 Lin EH et al 1995. Research suggests that learning is more ef-fective if the information is explicit, organised in lists, and in a logical order. Instructionsthat align well with the patient's routine for taking medications are better rememberedMorrow D et al 1991; a combination of both oral and written formats has been identifiedas being of the most help Martens KH et al 1998.
Evaluating physical ability
Poor vision and low manual dexterity are associated with poor medication self-manage-ment Ruscin JM and Semla TP 1996 Lorenc L and Branthwaite A 1993. HCPs are encour-aged to assess whether or not a patient is able to properly read medication labels andhas the appropriate strength and dexterity to open containers. This can be done simplyby asking them to read a label or to open a container. This is especially important for old-er people and patients with existing diabetes-related complications such as retinopathyand neuropathy.
Copyright Steno Diabetes Center 2016
Steno Diabetes Center – Courses in Clinical Diabetes Care
Assessing cognitive capacity
Poor cognition is associated both with over- and under-adherence to a prescribed med-ication regimen Salas M et al 2001 Maddigan SL et al 2003 Raji MA et al 2004. Forget-ting is a major reason for the omission of medication doses Dolce JJ et al 1991 Conn Vet al 1994 Pettinger MB et al 1999. To assess cognitive capacity, try asking patients "Howoften during a week do you forget to take your medication?"
It may be helpful to have patients indicate how often they take their medications on anexercise sheet about medication adherence. Click on the pdf below to download a med-ication adherence exercise sheet.
If a patient indicates they have a habit of forgetting, engage them in a conversationabout strategies for improving their recollection. Possible solutions may include:
• Development of memory cues tailored to the patient's lifestyle.
• Storing medicines in a special place, and associating medicine taking with a daily
event or routine, such as a mealtime.
• Compliance aids, such as pill boxes and pill organisers.
• Medication schedules, calendars and checklists, especially in combination with ed-
ucation and use of a pill box.
Identifying intentional non-adherence
In a study of chronically il people who were starting a new treatment found that almosta third did not take their medication as prescribed, and that this was deliberate, for halfof the time Barber N et al 2004. Perceptions of the seriousness of their illness and vul-nerability to complications were significantly related to medication adherence Kiortsis DNet al 2000 Connelly CE 1993 McDonald-Miszczak L et al 2004. A major reason that olderadults skip doses or stop taking their medicines is related to the side effects of medica-tion Barber N et al 2004 Kiortsis DN et al 2000. It is important to ascertain a person'smotivation for choosing to take or not to take their medicine. Once the motivating fac-tors have been identified, HCPs can collaborate with patients to identify strategies forimproving adherence. Involving patients in the process of decision making can improveself-efficacy Edworthy SM and Devins GM 1999.
Copyright Steno Diabetes Center 2016
Lesson 3: Multifactorial Approach to Cardiovascular Disease
Conducting ongoing monitoring
Monitoring medication adherence is an ongoing process. One study found that only 31%of people with type 2 diabetes who were prescribed an oral hypoglycaemic adhered totheir medication regimen Donnan PT et al 2002. In another study, people on oral hypo-glycaemic medications were non-adherent for an average of 64.7 days per year Lin EH etal 2004. Since adherence to a medication regimen for type 2 diabetes is strongly associ-ated with metabolic control, interventions related to monitoring and improving adherenceare critical. Continuous monitoring may include:
• Assessing medication adherence• Evaluating medication side effects• Determining medication effectiveness
Copyright Steno Diabetes Center 2016
Steno Diabetes Center – Courses in Clinical Diabetes Care
Copyright Steno Diabetes Center 2016
Summary
Cardiovascular disease (CVD) is the major cause of morbidity and mortality for individuals
with diabetes and is a large contributor to the direct and indirect costs of diabetes. Most type
2 diabetes patients have other co-existing risk factors for CVD, such as: abdominal obesity,
high serum triglycerides, low HDL-cholesterol, and elevated blood pressure. Together with el-
evated glucose levels, these are known collectively as the metabolic syndrome. Strict control
of cardiovascular risk factors, such as smoking, hypertension (and microalbuminuria), dys-
lipidaemia, glycaemic control, and treatment with antiplateletagents, is necessary to reduce
the risk of cardiovascular disease, although the desired treatment targets vary among indi-
viduals. The best outcomes come from a multifactorial approach, where multiple risk factors
are treated simultaneously, an approach that has been proven to reduce both cardiovascular
events and mortality.
Copyright Steno Diabetes Center 2016
Steno Diabetes Center – Courses in Clinical Diabetes Care
1. Fowler M. Microvascular and Macrovascular Complications of Diabetes. Clinical Diabetes
2. Emerging Risk Factors Collaboration et al. Diabetes mellitus, fasting glucose, and risk
of cause-specific death. N Engl J Med 2011; 364: 829-41
3. Gaede P et al. Effect of a multifactorial intervention on mortality in type 2 diabetes. N
Engl J Med 2008; 358: 580-91
4. Ali MK et al. Achievement of goals in U.S. Diabetes Care, 1999-2010. N Engl J Med
5. American Diabetes Association. Standards of Medical Care in Diabetes—2015. (9) Mi-
crovascular complications and foot care. Diabetes Care 2015; 38, Suppl 1: S58-66
6. Alberti KG et al. Harmonizing the metabolic syndrome: a joint interim statement of the
International Diabetes Federation Task Force on Epidemiology and Prevention; Nation-al Heart, Lung, and Blood Institute; American Heart Association; World Heart Federa-tion; International Atherosclerosis Society; and International Association for the Studyof Obesity. Circulation 2009; 120: 1640-5
7. Handler J. The importance of accurate blood pressure measurement. Perm J 2009; 13:
8. Campbell NR and McKay DW. Accurate blood pressure measurement: why does it mat-
ter? CMAJ 1999; 161: 277-8
9. Hansen TW et al. Ambulatory blood pressure and mortality: a population-based study.
Hypertension 2005; 45: 499-504
10. Arguedas JA et al. Blood pressure targets for hypertension in people with diabetes mel-
litus. Cochrane Database Syst Rev 2013; 10: CD008277
11. Bangalore S et al. J-curve revisited: An analysis of blood pressure and cardiovascular
events in the Treating to New Targets (TNT) Trial. Eur Heart J 2010; 31: 2897-908
12. McBrien K et al. Intensive and Standard Blood Pressure Targets in Patients With Type
2 Diabetes Mellitus: Systematic Review and Meta-analysis. Arch Intern Med 2012; 172:1296-303
13. ACCORD Study Group et al. Effects of medical therapies on retinopathy progression in
type 2 diabetes. N Engl J Med 2010; 363: 233-44
14. James PA et al. 2014 evidence-based guideline for the management of high blood pres-
sure in adults: report from the panel members appointed to the Eighth Joint NationalCommittee (JNC 8). JAMA 2014; 311: 507-20
15. Estacio RO et al. The effect of nisoldipine as compared with enalapril on cardiovascular
outcomes in patients with non-insulin-dependent diabetes and hypertension. N Engl JMed 1998; 338: 645-52
16. Mancia G et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension:
the Task Force for the management of arterial hypertension of the European Societyof Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens2013; 31: 1281-357
17. Cholesterol Treatment Trialists' (CTT) Collaborators et al. Efficacy of cholesterol-lower-
ing therapy in 18,686 people with diabetes in 14 randomised trials of statins: a meta-analysis. Lancet 2008; 371: 117-25
Copyright Steno Diabetes Center 2016
18. AIM-HIGH Investigators et al. Niacin in patients with low HDL cholesterol levels receiv-
ing intensive statin therapy. N Engl J Med 2011; 365: 2255-67
19. Hovingh GK et al. Cholesterol ester transfer protein inhibition by TA-8995 in patients
with mild dyslipidaemia (TULIP): a randomised, double-blind, placebo-controlled phase2 trial. Lancet 2015; 386: 452-60
20. Look AHEAD Research Group et al. Cardiovascular effects of intensive lifestyle inter-
vention in type 2 diabetes. N Engl J Med 2013; 369: 145-54
21. Collins R et al. MRC/BHF Heart Protection Study of cholesterol-lowering with simvas-
tatin in 5963 people with diabetes: a randomised placebo-controlled trial. Lancet 2003;361: 2005-16
22. Stone NJ et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce
atherosclerotic cardiovascular risk in adults: a report of the American College of Cardi-ology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129 (25, Suppl 2): S1-45
23. Keech A et al. Effects of long-term fenofibrate therapy on cardiovascular events in 9795
people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial.
Lancet 2005; 366: 1849-61
24. Chew EY et al. The effects of medical management on the progression of diabetic
retinopathy in persons with type 2 diabetes: the Action to Control Cardiovascular Riskin Diabetes (ACCORD) Eye Study. Ophthalmology 2014; 121: 2443-51
25. Sabatine MS et al. Efficacy and safety of evolocumab in reducing lipids and cardiovas-
cular events. N Engl J Med 2015; 372: 1500-9
26. Yudkin JS. How can we best prolong life? Benefits of coronary risk factor reduction in
non-diabetic and diabetic subjects. BMJ 1993; 306: 1313-8
27. Al-Delaimy WK et al. Smoking and risk of coronary heart disease among women with
type 2 diabetes mellitus. Arch Intern Med 2002; 162: 273-9
28. Chaturvedi N et al. Which features of smoking determine mortality risk in former ciga-
rette smokers with diabetes? The World Health Organization Multinational Study Group.
Diabetes Care 1997; 20: 1266-72
29. Antithrombotic Trialists' (ATT) Collaboration et al. Aspirin in the primary and secondary
prevention of vascular disease: collaborative meta-analysis of individual participant da-ta from randomised trials. Lancet 2009; 373: 1849-60
30. Pignone M et al. Aspirin for primary prevention of cardiovascular events in people with
diabetes: a position statement of the American Diabetes Association, a scientific state-ment of the American Heart Association, and an expert consensus document of theAmerican College of Cardiology Foundation. Circulation 2010; 121: 2694-701
31. Anand SS et al. Glucose levels are associated with cardiovascular disease and death in
an international cohort of normal glycaemic and dysglycaemic men and women: theEpiDREAM cohort study. Eur J Prev Cardiol 2012; 19: 755-64
32. Stratton IM et al. Association of glycaemia with macrovascular and microvascular com-
plications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 2000;321: 405-12
33. Skyler JS et al. Intensive glycemic control and the prevention of cardiovascular events:
implications of the ACCORD, ADVANCE, and VA diabetes trials: a position statement ofthe American Diabetes Association and a scientific statement of the American Collegeof Cardiology Foundation and the American Heart Association. Circulation 2009; 119:351-7
Copyright Steno Diabetes Center 2016
Steno Diabetes Center – Courses in Clinical Diabetes Care
34. Inzucchi SE et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-
centered approach: update to a position statement of the American Diabetes Associa-tion and the European Association for the Study of Diabetes. Diabetes Care 2015; 38:140-9
35. Holman RR et al. 10-year follow-up of intensive glucose control in type 2 diabetes. N
Engl J Med 2008; 359: 1577-89
36. Effect of intensive blood-glucose control with metformin on complications in overweight
patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS)Group. Lancet 1998; 352: 854-65
37. Zinman B et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Dia-
betes. N Engl J Med 2015; 373: 2117-28
38. BARI 2D Study Group et al. A randomized trial of therapies for type 2 diabetes and
coronary artery disease. N Engl J Med 2009; 360: 2503-15
39. Gaede P et al. Multifactorial intervention and cardiovascular disease in patients with
type 2 diabetes. N Engl J Med 2003; 348: 383-93
40. Ickovics JR and Meisler AW. Adherence in AIDS clinical trials: a framework for clinical
research and clinical care. J Clin Epidemiol 1997; 50: 385-91
41. Haynes RB et al. Helping patients follow prescribed treatment: clinical applications. JA-
MA 2002; 288: 2880-3
42. Dunbar-Jacob J et al. Medication adherence in persons with cardiovascular disease. J
Cardiovasc Nurs 2003; 18: 209-18
43. Yiannakopoulou ECh et al. Adherence to antihypertensive treatment: a critical factor
for blood pressure control. Eur J Cardiovasc Prev Rehabil 2005; 12: 243-9
44. Marek KD and Antle L. 2008. Medication Management of the Community-Dwelling Old-
er Adult. In RG Hughes, ed. Patient Safety and Quality: An Evidence-Based Handbookfor Nurses. Rockville, MD: Agency for Healthcare Research and Quality.
45. Barat I et al. Drug therapy in the elderly: what doctors believe and patients actually
do. Br J Clin Pharmacol 2001; 51: 615-22
46. Bonner CJ and Carr B. Medication compliance problems in general practice: detection
and intervention by pharmacists and doctors. Aust J Rural Health 2002; 10: 33-8
47. Fineman B and DeFelice C. A study of medication compliance. Home Healthc Nurse
48. Torrible SJ and Hogan DB. Medication use and rural seniors. Who really knows what
they are taking? Can Fam Physician 1997; 43: 893-8
49. Aparasu RR and Sitzman SJ. Inappropriate prescribing for elderly outpatients. Am J
Health Syst Pharm 1999; 56: 433-9
50. Bloom JA et al. Potentially undesirable prescribing and drug use among the elderly.
Measurable and remediable. Can Fam Physician 1993; 39: 2337-45
51. Zhan C et al. Potentially inappropriate medication use in the community-dwelling elder-
ly: findings from the 1996 Medical Expenditure Panel Survey. Jama 2001; 286: 2823-9
52. Heisler M et al. Clinician identification of chronically il patients who have problems pay-
ing for prescription medications. Am J Med 2004; 116: 753-8
53. Piette JD et al. Cost-related medication underuse among chronically il adults: the treat-
ments people forgo, how often, and who is at risk. Am J Public Health 2004; 94: 1782-7
54. Mojtabai R and Olfson M. Medication costs, adherence, and health outcomes among
Medicare beneficiaries. Health Aff (Millwood) 2003; 22: 220-9
55. Arnsten JH et al. Determinants of compliance with anticoagulation: A case-control
study. Am J Med 1997; 103: 11-7
Copyright Steno Diabetes Center 2016
56. Yilmaz MB et al. Being well-informed about statin is associated with continuous adher-
ence and reaching targets. Cardiovasc Drugs Ther 2005; 19: 437-40
57. Lin EH et al. The role of the primary care physician in patients' adherence to antide-
pressant therapy. Med Care 1995; 33: 67-74
58. Morrow D et al. Elders' schema for taking medication: implications for instruction de-
sign. J Gerontol 1991; 46: P378-85
59. Martens KH. An ethnographic study of the process of medication discharge education
(MDE). J Adv Nurs 1998; 27: 341-8
60. Ruscin JM and Semla TP. Assessment of medication management skills in older outpa-
tients. Ann Pharmacother 1996; 30: 1083-8
61. Lorenc L and Branthwaite A. Are older adults less compliant with prescribed medication
than younger adults? Br J Clin Psychol 1993; 32 ( Pt 4): 485-92
62. Salas M et al. Impaired cognitive function and compliance with antihypertensive drugs
in elderly: the Rotterdam Study. Clin Pharmacol Ther 2001; 70: 561-6
63. Maddigan SL et al. Predictors of older adults' capacity for medication management in a
self-medication program: a retrospective chart review. J Aging Health 2003; 15: 332-52
64. Raji MA et al. Ethnic differences in antihypertensive medication use in the elderly. Ann
Pharmacother 2004; 38: 209-14
65. Dolce JJ et al. Medication adherence patterns in chronic obstructive pulmonary disease.
Chest 1991; 99: 837-41
66. Conn V et al. Cognitive impairment and medication adherence. J Gerontol Nurs 1994;
67. Pettinger MB et al. Compliance to multiple interventions in a high risk population. Ann
Epidemiol 1999; 9: 408-18
68. Barber N et al. Patients' problems with new medication for chronic conditions. Qual Saf
Health Care 2004; 13: 172-5
69. Kiortsis DN et al. Factors associated with low compliance with lipid-lowering drugs in
hyperlipidemic patients. J Clin Pharm Ther 2000; 25: 445-51
70. Connelly CE. An empirical study of a model of self-care in chronic illness. Clin Nurse
Spec 1993; 7: 247-53
71. McDonald-Miszczak L et al. A pilot study examining older adults' beliefs related to med-
ication adherence: the BERMA survey. J Aging Health 2004; 16: 591-614
72. Edworthy SM and Devins GM. Improving medication adherence through patient educa-
tion distinguishing between appropriate and inappropriate utilization. Patient EducationStudy Group. J Rheumatol 1999; 26: 1793-801
73. Donnan PT et al. Adherence to prescribed oral hypoglycaemic medication in a popula-
tion of patients with Type 2 diabetes: a retrospective cohort study. Diabet Med 2002;19: 279-84
74. Lin EH et al. Relationship of depression and diabetes self-care, medication adherence,
and preventive care. Diabetes Care 2004; 27: 2154-60
Copyright Steno Diabetes Center 2016
Steno Diabetes Center – Courses in Clinical Diabetes Care
Acronyms and Abbreviations
ACE – Angiotensin-Converting Enzyme
ADA - American Diabetes Association
AHA - antihyperglycaemic agents
ARB - Angiotensin II Receptor Blocker
ASA - American Stroke Association
BP – blood pressure
CHD – coronary heart disease
CVD - cardiovascular disease
HbA1c - glycated haemoglobin
HCP - healthcare professional
HDL - high-density lipoprotein
LDL - low-density lipoprotein
MI - myocardial infarction
SGLT - sodium-glucose co-transporter
TIA - transient ischaemic attack
WHO - World Health Organization
Copyright Steno Diabetes Center 2016
Source: https://macrovascularcompdoctor.ibog.steno.dk/fileadmin/indhold/EBook/macrovascularcompdoctor.ibog.steno.dk.pdf
The Fair Labor Standards Act Exemptions and the Pharmaceuticals Industry: Are Sales Representatives Entitled to Overtime?Steven I. Locke Follow this and additional works at: Part of the nd the Recommended CitationSteven I. Locke (2009) "The Fair Labor Standards Act Exemptions and the Pharmaceuticals Industry: Are Sales RepresentativesEntitled to Overtime?," Barry Law Review: Vol. 13: Iss. 1, Article 1.Available at:
ADVANCES IN NEUROPSYCHIATRY Neuropsychiatry of the basal ganglia J Neurol Neurosurg Psychiatry 2002;72:12–21 This review aims to relate recent findings describing the parts of the basal ganglia closest to limbic role and neural connectivity of the basal ganglia to the structures and that are involved in cognitive and clinical neuropsychiatry of basal ganglia movement