Powerpoint presentation
Acute Pancreatitis:
• differentiate between categories of acute pancreatitis • list the most common etiologic factors for acute pancreatitis
• differentiate between new and old management concepts of acute
Robin Donohoe Dennison, DNP,
copyright Robin Donohoe Dennison 2015
• Mild (previously referred to as
• Severe (previously referred to as
Acute Pancreatitis
interstitial pancreatitis)
necrotizing pancreatitis)
• Edema with little or no necrosis
• Extensive necrosis of pancreas and
peripancreatic fact
• Hypovolemia as a result of fluid
• Erosion into blood vessels with
Acute Inflammation of the Pancreas
leak into peritoneal cavity
• Usually resolves within 7 days
• SIRS frequently occurs • High complication rate and
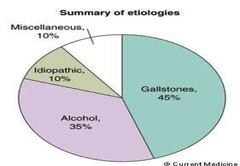
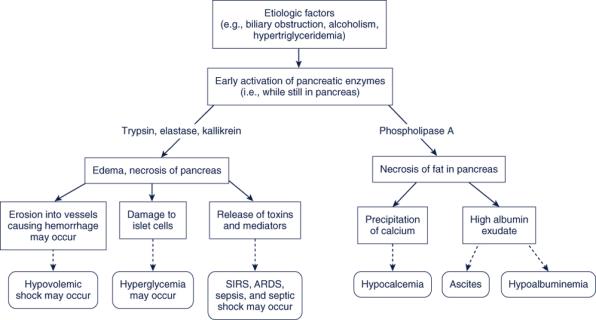
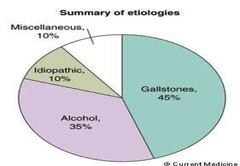
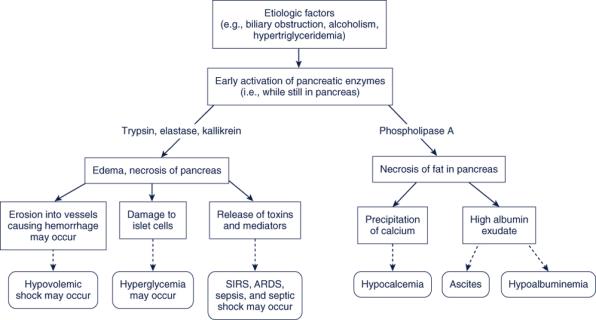
• Obstruction of common bile duct:
• Thiazide diuretics
• Sulfonamides
second most common cause
• Post-endoscopic retrograde
• Azathioprine (Imuran)
cholangiopancreatography (ERCP)
• Alcoholism: most common cause
• Procainamide
• Chronic alcohol intake leads to
• Tetracycline
secretory and structural changes in
the pancreas contributing to duct
• Alcohol increases the amount of
• Hypertriglyceridemia
• Peptic ulcer with perforation
• Pregnancy: third trimester; ectopic pregnancy
• Cancer especially tumors of pancreas or lung
• Ovarian cyst
• Injury to pancreas
• Hypercalcemia
• Lupus erythematosus
• Coxsackievirus B
• Infectious mononucleosis
• Radiation injury
• Viral hepatitis
Dennison, 2013
• Ischemia (e.g., shock and multiple organ dysfunction syndrome) • Post-cardiopulmonary bypass • Infection, sepsis • Hereditary factors • Idiopathic (20% of cases)
Clinical presentation: Subjective
Clinical presentation: Subjective
• May have history of precipitating event
• Associated symptoms
• Abdominal pain
• Abdominal tenderness, guarding
• Precipitating: may occur after a heavy meal, especially if fatty, or a drinking
• Nausea, vomiting, retching
• Palliation: may be eased by leaning forward or fetal position
• Flatulence, diarrhea
• Quality: "boring"
• Region: diffuse in epigastrium but may be in left upper quadrant
• Radiation: to back or flanks • Severity: moderate to very severe • Timing: sudden onset; constant

Clinical presentation: Objective
Clinical presentation: Objective
• Grey Turner's signs or Cullen's sign
may be seen in with hemorrhage
• Hypotension may be seen due to decreased circulating volume due to
• Abdominal distention
effusion or hemorrhagic; may be decreased due to SIRS and/or sepsis
• Decreased bowel sounds
• Fever: usually low-grade (e.g., 37.8-39C)
• Indications of peritoneal irritation:
involuntary guarding during
Jaundice possible if biliary obstruction
palpation of the abdomen
• Epigastric mass may be palpable
especially if pseudocyst
• Ascites may be present
• Steatorrhea (i.e., bulky, pale, foul-
smelling, floating)
SIRS: 30% of patients with acute pancreatitis
Clinical presentation: Objective
have SIRS within 48 hours after admission
• Breath sounds changes: may be diminished due to atelectasis, pleural
• 2 or more of the following
effusion, or ARDS; crackles may also be heard
• Tachycardia (more than 90 beats/min)
• Chvostek's or Trousseau's signs may be positive in hypocalcemia
• Hyperpnea (respiratory rate > 20 breaths/min or PaCO2 < 32 mm Hg)
• Hyperthermia (temperature > 38 C) or hypothermia (temperature < 36 C) • Leukocytosis (WBC count > 12,000 cells/mm3) or leukopenia (WBC count <
4000 cells/mm3 or > 10% bands)
Clinical presentation: Diagnostic
Clinical presentation: Diagnostic
• Lipase: elevated
• Potassium: may be decreased especially if vomiting
• Stays elevated longer than amylase
• Calcium: decreased
• More specific than amylase
• Magnesium: decreased
• Albumin: decreased
• Glucose: elevated if endocrine function of the pancreas is
• BUN: may be elevated due to hypovolemia
• AST, ALT, LDH, alkaline phosphatase, bilirubin: elevated in liver or
• Triglycerides: may be elevated
• Amylase: usually elevated to greater than 3x normal
• Peaks at 4-24 hours after onset of symptoms; usually returns to normal
• May not be elevated if pancreatitis is due to hypertryiglyceremia
Clinical presentation: Diagnostic
Clinical presentation: Diagnostic
• Stool: increase in fecal fat
• Decreased with hemorrhage • Elevated with hemoconcentration due to third-spacing
• ECG: may suggest MI (e.g., ST-T wave elevations)
• WBC: usually elevated with left shift
• Arterial blood gases
• May show left pleural effusion, elevated left hemidiaphragm, left atelectasis
• Metabolic acidosis
• May show pulmonary complications of pancreatitis (e.g., atelectasis,
pneumonia, ARDS, pleural effusion)
Respiratory complications may cause respiratory acidosis and hypoxemia
• Flat plate of abdomen
• May show cause (e.g., cholelithiasis)
• May show ileus and bowel dilation
Amylase: usually elevated
• May show calcified pancreatic stones
Clinical presentation: Diagnostic
Balthazar and Ranson's system for grading
pancreatitis by CT findings
• May show delayed gastric emptying
Grade A: Normal pancreas
May show enlargement of duodenum
• May show presence of dilated loop of smooth bowel adjacent to the pancreas
• Grade B: Focal or diffuse enlargement of pancreas
• Abdominal ultrasound: may show pancreatic swelling, edema,
• Grade C: Mild peripancreatic inflammatory changes
gallstone, pseudocyst, or peripancreatic fluid collections
• Grade D: Fluid collection in a single location
• Grade E: Multiple fluid collections or gas within the pancreas or
• May show enlargement, edema, or necrosis of the pancreas
peripancreatic inflammation
• May show complications of pancreatitis (e.g., pancreatic pseudocyst or
Clinical presentation: Diagnostic
Ranson's Prognostic Criteria
• At the time of admission or
• MRI: shows inflammatory changes within the pancreas
• Mild or Severe
• Age over 55 years
• WBC over 16,000/mm3
• Endoscopic retrograde cholecystopancreatography (ERCP)
• Mild: scores only 1-2
• Serum glucose greater than 200
Contraindicated in acute pancreatitis
Severe: scores more than
• Serum lactate dehydrogenase (LDH)
Remember that pancreatitis is a complication of this study
greater than 350 units/L
• Used more often in chronic pancreatitis; identifies ductal changes or calculi
• Serum aspartate aminotransferase
(AST) greater than 250 units/L
• HIDA scan: may identify hepatocellular disease from biliary
• 0 to 2 : 2% mortality
• After 48 hours
obstruction as cause of pancreatitis
• 3 to 4 : 15% mortality
• Hct drop greater than 10%
• Increase in BUN greater than 5 mg/dL
5 to 6 : 40% mortality
Peritoneal lavage: positive for blood if hemorrhage
• 7 to 8 : 100% mortality
• Calcium less than 8 mg/dL
• Base deficit greater than 4 mEq/L
• Estimated fluid sequestration greater
• PaO2 less than 60 mm Hg
Maintain airway, oxygenation, ventilation
• Elevate head of bed 30-45 especially if ascites restricts
diaphragmatic excursion
Collaborative management
• Administer oxygen as necessary to maintain SaO2 94% unless
• In patients with COPD, administer oxygen to achieve a SaO2 of 90% by pulse
• Monitor SaO2 closely and evaluate work of breathing in detection of
development of atelectasis and/or ARDS
Maintain adequate circulating volume and fluid
Decrease release of and destruction by
and electrolyte balance
pancreatic enzymes
• Administer crystalloids and colloids as required to restore circulating
blood volume: 5-10 ml/kg/hr
• Assist with treatment of cause
• Hemodynamic monitoring may be necessary
• Alcohol cessation if alcohol related
• Cholecystectomy after resolution of pancreatitis if caused by cholelithiasis
• Fluid sequestration: abdominal hypertension, abdominal compartment
• Discontinuance of offending drug if drug induced
• Statins, niacin, fibrates, and/or omega-3 fatty acids if related to
• Monitor sodium, calcium, potassium, magnesium, and phosphate
hypertriglyceridemia
Administer calcium replacement orally or intravenous as prescribed
• Administer potassium replacement as prescribed • Restrict sodium to 500 mg/daily for patients with ascites
• Measure abdominal girth daily for patients with ascites • Weigh daily at same time on same scale
Decrease release of and destruction by
Decrease release of and destruction by
pancreatic enzymes
pancreatic enzymes
• Maintain NPO status during acute phase and with any recurrence of
• Keep environment free of food odors
• Perform mouth care with water or normal saline only; do not use
• Insert nasogastric tube and maintain suction to keep stomach
alcohol-containing or flavored mouthwash or toothpaste
decompressed and inhibit secretion of pancreatic juices
• Administer drugs to decrease pancreatic enzymes
• Octreotide acetate (Sandostatin) 50 mcg/hr IV for 72 hours in the early stage
of AP could prevent the development of SAP
• H2 receptor antagonists IV: no longer recommended
Decrease release of and destruction by
Prevent and treat pain and discomfort
pancreatic enzymes
• Maintain bedrest; encourage knee flexing while in supine position to
• Perform peritoneal lavage: may be used for severe pancreatitis
relax abdominal muscles
• Performed percutaneous or via laparotomy
• Maintain quiet environment, comfortable temperature, dim lighting
• Intraperitoneal space is rinsed with lavage fluid to remove toxic substances
released from the pancreas
• Administer analgesics
• May be done for 2-3 days
• Opiates (fentanyl, hydromorphone, morphine)
• Technique is the same as for peritoneal dialysis for renal failure
• PCA preferred
• HOWEVER: the lavage of the peritoneal cavity in patients with severe acute
pancreatitis does not appear to confer a clinical benefit.
• Dong, Z., Petrov, M. S., Xu, J., Shanbhag, S., Windsor, J. A., & Pang, S. (2010). Peritoneal
lavage for severe acute pancreatitis: A systematic review of randomised trials. World J
Surg, 34(9), 2103-2108. doi: 10.1007/s00268-010-0665-3
Prevent and treat pain and discomfort
Note: though meperidine (Demerol) for
• Consider neurolytic block of celiac plexus for severe persistent pain
years has been considered the analgesic
• Utilize nonpharmacologic pain relief methods (e.g., imagery,
of choice in acute pancreatitis, recent
• Treat nausea with prescribed antiemetics; perform mouth care after
studies show no significant difference
emesis should it occur
• Ensure adequate sleep and rest
between morphine and meperidine in
• Consider increase in pain as ominous: may indicate pancreatic
necrosis, abscess formation, or hemorrhage
the degree of spasm of the sphincter of Oddi
Administer appropriate nutritional support
Prevent and monitor for infection
considering restrictions • Administer nutritional support parenterally during acute phase of illness
• Antibiotics that effectively penetrate the pancreatic tissue and provide
• Administer enteral nutrition below the duodenum after ileus is resolved
good coverage against gram-negative enteric and anaerobic organisms
(e.g., imipenem/cilastatin [Primaxin], ofloxacin [Floxin], metronidazole
Elemental (i.e., Vivonex)
[Flagyl]) may be prescribed.
• Below the ligament of Treitz (e.g., jejunostomy tube)
Clear liquids or elemental diet such as Vivonex after inflammation subsides
If there is no improvement after 1 week, a CT-guided aspiration may be
(pain subsides, serum amylase normal) low fat, full liquids eventually
performed. Bacteria found present in the aspirate suggests pancreatic
necrosis with infection and indicates the need for surgery.
Avoid alcohol and food high in fat
Monitor for clinical indications of abscess formation
• Increase in abdominal pain
• Administer fat-soluble vitamins, thiamine, folic acid
• Monitor serum glucose levels closely and administer glucose or insulin as
• Leukocytosis
Prepare patient for surgical measures for
Prepare patient for surgical measures for
relief of pancreatitis if necessary
relief of pancreatitis if necessary
• During acute phase, surgery is performed only if absolutely necessary
• Pancreatic resection/total
• Cholecystectomy if bile reflux is the cause of pancreatitis
Used if pancreas and/or other organs
Drainage and removal of abscess or pseudocysts
• Pancreatic pseudocysts occur when digestive juices break through the normal
• Total pancreatectomy
ducts of the pancreas and collect in spaced lined by fibroblasts and surfaces
• Results in diabetes and other metabolic
of adjacent organs
• Islet cell autotransplantation is
sometimes performed
• Segmental pancreatic
autotransplantation is sometimes performed: part of viable pancreatic tissue reimplanted following total pancreatectomy
Maintain normal serum glucose levels
Assess for alcohol withdrawal syndrome
• Monitor serum glucose levels closely
• If present, administer sedatives (e.g. chlordiazepoxide [Librium]) as
• Administer insulin as indicated and prescribed
Most drugs used for this purpose including chlordiazepoxide (Librium) have
Maintain constant infusion rate of TPN or enteral feedings
potential for liver toxicity; dosage is adjusted and liver function studies are monitored
• Avoid alcohol-containing mouthwash or medications
Monitor for complications
Monitor for complications
• Hypoglycemia or hyperglycemia
• Disseminated intravascular
• Pseudocysts: collection of inflammatory debris, pancreatic
• Hypocalcemia
coagulation (DIC)
secretions, and necrotic tissue; may cause compression of portal vein and bile duct or rupture and peritonitis and sepsis
• DVT, PE: SCD
• Causes pain or ache in abdomen, feeling of bloating, or poor digestion
• Acute renal failure
• Treatment: nothing for small cysts or drainage by surgical, endoscopic, or
percutaneous approach for larger cysts
Pancreatic fistula: communication between the pancreas and the skin; pancreatic secretions drain onto the skin
• Treatment : replacement of fluids and electrolytes; octreotide

• Andris, A. (2010). Pancreatitis: understanding the disease and implications for
care. AACN Adv Crit Care, 21(2), 195-204.
• de-Madaria, E. (2014). Fluid therapy in acute pancreatitis - Aggressive or
adequate? Time for reappraisal. Pancreatology, 14(6), 433-435.
• Dennison, R. D. [2013]. Pass CCRN! [4 ed]. Philadelphia: Elsevier. • Kramer, C., & Jeffery, A. (2014). Pancreatitis in children. Crit Care Nurse, 34(4), 43-
• Marchiondo, K. (2010). Acute pancreatitis. Medsurg Nurs, 19(1), 54-55. • Schepers, N. J., Besselink, M. G. H., van Santvoort, H. C., Bakker, O. J., & Bruno, M.
J. (2013). Early management of acute pancreatitis. Best Practice & Research
Clinical Gastroenterology, 27(2013), 727-743.
• Siow, E. (2008). Enteral versus parenteral nutrition for acute pancreatitis. Crit Care
Nurse, 28(4), 19-25, 27-31; quiz 32.
• Wang, S., Feng, X., Li, S., Liu, C., Xu, B., Bai, B., . . Zhao, Q. (2014). The ability of
current scoring systems in differentiating transient and persistent organ failure in
patients with acute pancreatitis. J Crit Care, 29(4), 693 e697-611.
1. Which of the following would be appropriate for
2. Which of the following would be a serious complication
pain management of a patient with acute pancreatitis?
of overhydration of a patient with acute pancreatitis?
(more than one may be correct)
(more than one may be correct)
a. pancreatic necrosis
b. intraabdominal hypertension
c. acute renal failure
d. hydromorphone
d. pulmonary edema
Source: http://nwchicagoaacn.org/wp-content/uploads/2015/03/Acute-Pancreatitis.pdf
dk;kZy; lsukuh] gkWdQkslZeq[;ky; Hkksiky Øekad@lsukuh@gkWd@D;w0,e0@423 @14] fnukad 20 @08@14 iqfyl egkfuns'kd e-iz- }kjk fuEukafdr lkexzh ds fy, fuekZrk @iznk;drkZvksa ls eksgjcan fufonk vkekaf=r dh tkrh gS%& dsEkks¶ykbZtMkaxjh Vh&'kVZ ¼jkm.M usd o dkWyj½ 1&lkexzh dh ek=k vko';drkuqlkj deh@o f) dh tk ldrh gSA 2&fufonk fuEukuqlkj jgsxh ¼v½ rduhdh fufonk ¼c½ foRrh; fufonkA 3&izR;sd vkbZVe dh rduhdh ,o afoRrh; fufonk,a vyx&vyx eksgjcan fyQkQs esa jgsxhA 4&fufonk
February 16, 1996 / Vol. 45 / No. RR-1 Defining the Public Health Impact Streptococcus pneumoniae : Report of a Working Group U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Centers for Disease Control and Prevention (CDC) Atlanta, Georgia 30333 The MMWR series of publications is published by the Epidemiology Program Office,Centers for Disease Control and Prevention (CDC), Public Health Service, U.S. Depart-ment of Health and Human Services, Atlanta, GA 30333.