Sullaser.com.br
Australasian Journal of Dermatology (2001)
42, 207–210
Subcutaneous fat necrosis of the newborn
following hypothermia and complicated by pain
and hypercalcaemia
Todd P Wiadrowski and Gillian Marshman
Flinders Medical Centre, Bedford Park, South Australia, Australia
history of the condition is for resolution without scarring. Themost common complication of SCFN is hypercalcaemia,
which has been associated with neonatal death.2 We describe
A female infant was delivered at term with compli-
a child with an overlapping clinical presentation following
cations of severe meconium aspiration and birth
medically induced hypothermia to treat birth asphyxia. In this
asphyxia. Surface cooling was performed in the first
case, the initial clinical features of cold panniculitis progressed
24 hours as part of the management of her birth
to those of SCFN, both clinically and histologically. This
asphyxia. Woody erythema was noted at 24 hours,
patient's case was further complicated by pain and hypercal-
followed by the formation of red–purple nodules on the
6th day. Clinical findings in the first 24 hours were sug-gestive of cold panniculitis. However, clinical and his-
CASE REPORT
tological findings progressed to be in keeping with thediagnosis of subcutaneous fat necrosis of the newborn
A female infant was born at term weighing 4350 g. Standard
(SCFN). Furthermore, the immediate postnatal period
maternal prenatal screens revealed no significant abnormal-
was complicated by pain resistant to treatment with
ities (haemoglobin, group and screen, glucose tolerance test,
opiates. Asymptomatic hypercalcaemia was noted on
rubella serology, syphilis serology, hepatitis B surface anti-
periodic testing at 7 weeks and treated by rehydration,
gen, hepatitis C serology, HIV serology and midstream urine
diuretics, prednisolone, etidronate and a low-calcium
specimen). The mother was noted to have mild hypertension
and -vitamin D diet. A review of the clinical and histo-
with associated oedema and albuminuria in the third
logical findings of the relevant panniculitides occurring
trimester. No medications were taken during the pregnancy.
in the postnatal period is presented, as well as a review
Table 1 details the significant events after delivery and over
of the treatment of hypercalcaemia in SCFN.
the ensuing months. During the first 24 hours, the child was
Key words: cold panniculitis, corticosteroids, etidro-
noted to be hypotensive with cardiogenic shock requiring
nate, infants, opiates, panniculitis.
dopamine, had a pneumothorax, acute renal failure and amild disseminated intravascular coagulation. Within the firsthours of life, a decision was made for paralysis and sedation,with her core temperature kept between 32 and 33°C to treat
her birth asphyxia. Hypothermia was achieved with the useof ice packs applied to the skin and turning off the overhead
Subcutaneous fat necrosis of the newborn (SCFN) is a transi-
heating lamps. Her temperature was monitored via a rectal
ent panniculitis of neonates typically presenting within the
probe. This temperature was held for 24 hours, then raised
first 6 weeks of life. Most reported cases involve infants at full
to 35°C and then 37°C over a 3 day period.
term or post-dates and of normal size for dates, but often with
Approximately 24 hours post-delivery, a pink woody oede-
a history of birth asphyxia, meconium aspiration, cyanosis,
matous change was noted on the infant's thighs and back, as
seizures and hypothermia. An association with maternal
well as petechiae on the right ankle. This progressively wors-
diabetes and pre-eclampsia has been reported.1 The natural
ened over the ensuing 4 days and the buttocks were noted tobe exquisitely tender to touch with grimacing and shrill cry.
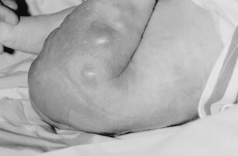
Plaques and nodules formed within these backgroundchanges at 6 days of age. A clinical diagnosis of SCFN was
Correspondence: Dr G Marshman, Dermatology Unit, Department
made (Fig. 1).
of Internal Medicine, Flinders Medical Centre, Flinders Drive, Bedford
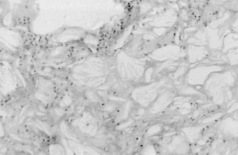
Histology revealed an acute panniculitis with frank fat
Park, SA 5042, Australia.
necrosis and needle-like clefts (Fig. 2), which confirmed the
Todd P Wiadrowski, BM, BS. Gillian Marshman, FACD.
Submitted 12 September 2000; accepted 6 February 2001.
clinical diagnosis of SCFN.
TP Wiadrowski and G Marshman
Purple nodules formed on erythematous and oedematous
Skin biopsy from sacral nodule demonstrating radially
buttock skin at seven days postnatally.
arranged needle shaped clefts at seven days postnatally (H&E).
Pain was poorly controlled by morphine. Due to continued
was also suggested that etidronate should not be given
difficulties with analgesia and the formation of new plaques
within 2 hours of milk feeds because calcium–drug binding
and nodules, prednisolone was added at a dose of 1 mg/kg per
may occur and reduce absorption. Cisapride (1 mg, orally
day on day 34. This led to a definite improvement in pain
t.d.s.) had already been commenced for the treatment of
control and subjective improvement in the intensity of the
the infant's GOR and this was continued while etidronate
was being administered. Calcium, parathyroid hormone and
Weekly measurements of serum calcium detected hyper-
1,25(OH)2-vitamin D3 levels were 3.49 mmol/L, 0.4 pmol/L
calcaemia at a corrected level of 3.74 mmol/L (normal
(normal range 1.1–6.9 pmol/L) and 55 pmol/L (normal range
range 2.20–2.75 mmol/L) 49 days after delivery. The infant's
50–160 pmol/L), respectively. These levels were taken at the
weight at this time was 4910 g. Intravenous access was
same time as the etidronate was started and it should be noted
particularly difficult to attain in this infant and, therefore,
that the infant had been taking prednisolone for 19 days prior
initial treatment was with oral fluids, frusemide (8 mg, orally
to this. A low-calcium and -vitamin D formula (Locasol) was
b.d.) and spironolactone (5 mg, orally b.d.). Prednisolone was
commenced on day 54 and frusemide and spironolactone were
being administered at a dose of 5 mg on alternate days when
ceased. Etidronate was continued for a total of 8 days treat-
hypercalcaemia was detected and this was then increased to
ment. At this time, calcium levels had normalized.
5 mg, daily.
Prednisolone was weaned over the ensuing 21 days because
After 4 days treatment, as described above, calcium levels
the infant's pain had settled.
were stable, but without significant decline. Etidronate
Locasol was continued for 7 months and, when the
was started at an oral dose of 25 mg, twice daily. Due to the
child was weaned onto solids, a diet low in calcium was
irritant nature of etidronate and the patient's underlying
used initially. This diet consisted of fruit, vegetables, meat,
gastro-oesophageal reflux (GOR), the infant was nursed in
cereals, such as rolled oats and semolina, and avoidance of
an upright position for 30 min following administration. It
dairy products. It was noted that some cereals, in particular
Time-course of presented case
Mid-cavity forceps delivery at term, thin meconium, cord pH 6.97
Apgar score 5, first spontaneous gasp followed this
Endotracheal oxygen, adrenaline, hypothermia-induced paralysis and sedation
Woody pink oedematous change on thighs and back, petechiae of right ankle
Buttocks noted to be tender to touch
Nodules arise within previously erythematous and oedematous areas
Biopsy taken; histology shows needle-shaped clefts in lipocytes and fat necrosis
Cisapride started
Prednisolone added at 1 mg/kg per day with subsequent improvement in pain relief
Hypercalcaemia 3.74 mmol/L corrected, treatment commenced with oral rehydration, frusemide and spironolactone, prednisolone dose increased back to 1 mg/kg per day
Hypercalcaemia 3.49 mmol/L corrected, etidronate 25 mg twice daily; normal vitamin D level
Locasol added, frusemide and spironolactone ceased
Etidronate ceased
Prednisolone ceased
Resolution of most nodules
Subcutaneous fat necrosis of the newborn
baby rice cereals, are fortified with calcium and should be
channel blocker have not been highlighted. In our case, the
avoided. A diet free of restrictions was commenced after
infant's lesions were noted to be painful as nodules began to
arise. Cold panniculitis has been described as having tender
The infant continued to display nodules, predominantly on
nodules in adults6 and it is not unreasonable to expect these
the proximal extremities and back, with slow resolution of
lesions may be tender in infants. Morphine, at doses of 1–2 mg
most of these lesions by 6 months. At 9 months, the firm
four times a day, was administered without complete pain con-
nodules that were present at her previous visit had altered
trol. It was decided to add prednisolone at a dose of 1 mg/kg
little. Magnetic resonance imaging (MRI) was performed.
per day. This had a synergistic effect with morphine, giving
Calcification was not present. The MRI appearances were of
complete pain control with doses of morphine that were pre-
septate lesions composed of soft tissue and lipid. The nodules
viously insufficient. There was also some subjective improve-
are stable and asymptomatic and further biopsy has not been
ment in the erythema overlying the nodules as well as a
decrease in nodule size. We believe that the use of predniso-lone should be strongly considered over the short-term in
cases complicated by painful lesions. Evidence is lacking as to whether this changes the overall disease course or
Subcutaneous fat necrosis of the newborn is an uncommon
transient panniculitis seen in term to post-term neonates that
Hypercalcaemia complicating SCFN is well recognized, but
usually resolves without scarring. Lesions often develop on
the pathogenesis is yet to be fully determined. Hypercalcaemia
skin that initially appears oedematous prior to the formation
occurs between 2 and 16 weeks, most commonly at 6–7
of red–purple nodules and plaques.1,3 The nodular lesions of
weeks.7 Clinically, the most common feature is failure to thrive
SCFN may present during the first 6 weeks, with one study
(90%), followed by fever, vomiting, feeding difficulties,
reporting 45% of lesions arising in the first week of life.4 A dif-
irritability and listlessness. Mortality from hypercalcaemia
ferential diagnosis would include sclerema neonatorum (SN)
complicating SCFN has been estimated at 15%.2 Because the
and cold panniculitis, as outlined in Table 2.
child may have been discharged by the time these features
Our patient was noted to have pink woody oedematous skin
arise, education of the parents to recognize these symptoms
on the thighs and back 24 hours after delivery. The distribution
and report this to the managing physician is essential. To the
of these areas corresponded to the areas of application of the
best of our knowledge there are no specific guidelines for
ice packs used to lower the child's core temperature.
routine monitoring of serum calcium levels in these cases. For
Therefore, these features could be in keeping with cold pan-
our patient, it was decided to perform weekly investigations
niculitis. However, at 6 days post-delivery, nodules were noted
of serum calcium and albumin levels until 16 weeks of age.
that steadily increased in size. These nodules were biopsied
Once a diagnosis of hypercalcaemia has been made, treat-
and demonstrated features in keeping with SCFN. Therefore,
ment options considered are outlined in Table 3.11 It is nec-
while we have clinical and histological evidence of SCFN, the
essary to stress the importance of adequate hydration in the
lack of a biopsy specimen of the earliest lesion allows us only
treatment of hypercalcaemia. Rehydration with a resultant
to speculate that, on clinical grounds, the infant either had an
increase in intravascular volume will increase glomerular
atypical presentation of SCFN or that this is a case of cold
filtration rate and increase renal calcium clearance.12
panniculitis progressing to SCFN.
Loop diuretics are used to achieve increased calcium
Painful lesions that proved to be difficult to control with
excretion by inhibiting calcium reabsorption and preventing
opiate analgesia complicated the course of our case. An infant
volume overload secondary to the rehydration. Thiazide
with painful SCFN requiring the use of morphine has been
diuretics should not be used because they increase distal
reported following the maternal use of amlodipine.10 Painful
tubular reabsorption of calcium and, therefore, may aggravate
lesions in cases of SCFN without the maternal use of a calcium
the process.
Differential diagnosis of subcutaneous fat necrosis of the newborn1,3,5–9
Subcutaneous fat necrosis
Cold panniculitis
Sclerema neonatorum
Full term/post-dates
Predisposing factors � Maternal diabetes, hypertension
No maternal factors
No maternal factors
� Birth asphyxia, meconium aspiration, cyanosis, Cold stress
Uneventful delivery
seizures, hypothermia
Within 72 hours of exposure
Within the first week
Red, blue nodules on trunk, buttock, arms, face,
Red, blue induration � plaques
Diffuse yellow–white � nodules,
sparing the genitalia, palms and soles
Fat necrosis, foreign body giant cells, lymphocytic
Lobular panniculitis, mixed
Needle-shaped clefts in
infiltrate, radially arranged needle-shaped clefts
infiltrate, no needle-shaped
lipocytes, nil to mild
inflammatory infiltrate or fatnecrosis, septa widened by oedema
Generally very good; hypercalcaemia carries a 15% Excellent
Poor, 75% mortality
TP Wiadrowski and G Marshman
Management of an infant with subcutaneous fat necrosis of the newborn11–14
Education of parents regarding disease and symptoms and signs of hypercalcaemia (failure to thrive, fever, vomiting,feeding difficulties, irritability and listlessness); protect areas of panniculitis from trauma plus dressings for ulceration
Weekly serum calcium and albumin levels to 16 weeks of age; rehydration, dietary vitamin D and calcium restriction,frusemide and prednisolone; consider etidronate if other measures fail
Opiates, prednisolone
Prednisolone is used in the treatment of hypercalcaemia,
failed. Normal serum calcium levels were subsequently main-
particularly in cases associated with haematogenous malig-
tained with dietary measures.
nancy or cases of 1,25(OH)2-vitamin D3 excess, such assarcoidosis. It has been suggested that the pathogenesis ofhypercalcaemia in SCFN may be similar to that of sarcoidosis
and, therefore, prednisolone would have a role in its treatment.
1. Fretzin DF, Arias AM. Sclerema neonatorum and subcutaneous
In our case, prednisolone was administered for 15 days prior
fat necrosis of the newborn. Pediatr. Dermatol. 1987; 4: 112–22.
to the onset of hypercalcaemia. This may suggest that either
2. Norwood Galloway A, Lebwohl M, Phelps RG, Raucher H.
the dose was inadequate, that prednisolone alone is unable
Subcutaneous fat necrosis of the newborn with hypercalcemia.
to treat hypercalcaemia associated with SCFN or that
J. Am. Acad. Dermatol. 1987; 16: 435–9.
the pathogenesis is unrelated or only partially related to the
3. Atherton DJ. The neonate. In: Champion RH, Burton JL, Burns
production of 1,25(OH)
DA, Breathnach SM (eds). Textbook of Dermatology, Vol. 1, 6th edn.
2-vitamin D3. We can only comment
Oxford: Blackwell Science, 1998; 449–518.
that, in our case, hypercalcaemia occurred despite the use of
4. Burden AD, Krafchik BR. Subcutaneous fat necrosis of the new-
prednisolone and that vitamin D3 levels, when taken, were
born: A review of 11 cases. Pediatr. Dermatol. 1999; 16: 384–7.
5. Black MM, Cunliffe WJ. Subcutaneous fat. In: Champion RH,
Etidronate is a member of the bisphosphonate group of
Burton JL, Burns DA, Breathnach SM (eds). Textbook of
drugs that are known to decrease bone resorption. Etidronate
Dermatology, Vol. 3, 6th edn. Oxford: Blackwell Science, 1998;
has been reported to be successful in the management hyper-
6. Bondi EE, Margolis DJ, Lazarus GS. Panniculitis. In: Freedberg
calcaemia associated with SCFN13 and, due to the resistant
IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI,
nature of the hypercalcaemia to first-line treatments described
Fitzpatrick TB (eds). Fitzpatrick's Dermatology in General
above, this was embarked upon. The dose used was 5 mg/kg,
Medicine, Vol. 1, 5th edn. New York: McGraw-Hill, 1999; 1275–89.
which was in keeping with the previous report. The use of
7. Hicks MJ, Levy ML, Alexander J, Flaitz CM. Subcutaneous fat
bisphosphonates, while effective in our case, should not be
necrosis of the newborn and hypercalcemia: Case report and
embarked on lightly because their effect on bone production,
review of the literature. Pediatr. Dermatol. 1993; 10: 271–6.
8. Lewis A, Cowen P, Rodda C, Dyall Smith D. Subcutaneous fat
growth plates and mineralization is yet to be clarified.14
necrosis of the newborn complicated by hypercalcaemia and
However, once etidronate was started, calcium levels fell to
thrombocytopenia. Australas. J. Dermatol. 1992; 33: 141–4.
normal, at which time etidronate was ceased.
9. Weedon D. Panniculitis. In: Skin Pathology. Edinburgh: Churchill
A low-calcium and -vitamin D3 formula should also be
Livingstone, 1997; 441–56.
added at the earliest possible stage and would optimally
10. Rosbotham JL, Johnson A, Haque KN, Holden CA. Painful sub-
have been best used in association with the initial treatments
cutaneous fat necrosis of the newborn associated with intra-
as described above if it had been readily available at our
partum use of a calcium channel blocker. Clin. Exp. Dermatol.
1998; 23: 19–21.
11. Ghirri P, Bottone U, Coccoli L, Bernardini M, Vuerich M, Cuttano
In conclusion, we present a case with early clinical features
A, Riparbelli C, Pellegrinetti G, Boldrini A. Symptomatic hyper-
in keeping with cold panniculitis, but an overall clinical and
calcemia in the first months of life: Calcium-regulating hormones
histological picture of SCFN. This case was unusual in that it
and treatment. J. Endocrinol. Invest. 1999; 22: 349–53.
was complicated by significant pain in the infant only partially
12. Wood AJJ. Management of acute hypercalcaemia. N. Engl. J. Med.
controlled with opiate anaesthesia. Oral prednisolone
1992; 326: 1196–203.
13. Rice AM, Rivkees SA. Etidronate therapy for hypercalcemia in
appeared to act synergistically with morphine to control this
subcutaneous fat necrosis of the newborn. J. Pediatr. 1999; 134:
infant's pain and should be considered for use in similar cases.
In this case, etidronate was used with success over an 8 day
14. Shoemaker LR. Expanding role of bisphosphonate therapy in
course to control hypercalcaemia when first-line treatment
children. J. Pediatr. 1999; 134: 264–7.
Source: http://sullaser.com.br/downloads/criolipolise-j.1440-0960.2001.00519.x.pdf
Efecto a nivel celular y molecular de agentes antitumoralesCellular and molecular effect of antitumor agents Silvia Ramírez-Sánchez*, Gildardo Rivera* La biología celular y molecular es un área de investigación de gran impacto y rápido creci-miento, la cual se ha convertido en un punto esencial para el desarrollo de nuevos agentes quimioterapéuticos con niveles bajos de toxicidad, particularmente para el cáncer. Aunque la era de la quimioterapia comenzó en los años 40, actualmente es necesario desarrollar nuevas terapias antitumorales que permitan tener un tratamiento apropiado para cada paciente y tipo de tumor, siendo necesaria la identificación de componentes celulares y moleculares involucrados en los procesos de carcinogénesis, para el desarrollo de agentes quimioterapéu-ticos que intervengan en la restauración o destrucción selectiva de las células cancerígenas. Actualmente, se ha demostrado que ciertos medicamentos, como los antibióticos (tetracic-linas, sulfonamidas y b-lactamas) y otros compuestos químicos (quinoxalinas) que son uti-
Treatment of Patients who decline transfusion of Blood Components and/or Blood Products November 2008 Page 1 of 23Page 1 of 23 Title: Treatment of Patients who decline transfusion of Blood Components and/or Blood Products Reference Number: Corp09/003 Implementation Date: This policy will be implemented after being signed off by the Chief Executive Review date: This policy will be reviewed one year after the effective date and thereafter every two years Responsible Officer: The officer responsible for reviewing this policy is the Haemovigilance Practitioner on behalf of the Hospital Transfusion Committee This policy has been developed within the context of Equality and Human Rights statutory obligations and requirements.