Digoxin toxicity with normal digoxin and serum potassium levels: beware of magnesium, the hidden malefactor
The Journal of Emergency Medicine, Vol. 45, No. 2, pp. e31–e34, 2013
Copyright Ó 2013 Elsevier Inc.
Printed in the USA. All rights reserved
0736-4679/$ - see front matter
DIGOXIN TOXICITY WITH NORMAL DIGOXIN AND SERUM POTASSIUM LEVELS:
BEWARE OF MAGNESIUM, THE HIDDEN MALEFACTOR
Mamatha Punjee Raja Rao, MBBSPrashanth Panduranga, MRCP,† Kadhim Sulaiman, FRCPI,† and
Mahmood Al-Jufaili, FRCPC
*Department of Emergency Medicine and †Department of Cardiology, Royal Hospital, Muscat, Oman
Reprint Address: Mamatha Punjee Raja Rao, MBBS, Department of Emergency Medicine, Royal Hospital, Post Box 1331, Muscat-111,
Sultanate of Oman
, Abstract—Background: In recent years, digoxin use has
the Digitalis Investigation Group trial, the overall inci-
been on the decline, with decreased incidence of digoxin tox-
dence of digoxin toxicity was 2% over a 3-year period
icity. Hence, digoxin toxicity, when it occurs, remains an elu-
. Recently, the incidence of digoxin toxicity has been
sive diagnosis to emergency physicians. Objective: To present
decreasing due to less use of digoxin in heart failure pa-
a case of digoxin toxicity with normal levels of digoxin and
tients, and it remains an elusive diagnosis to emergency
serum potassium, but with severe hypomagnesemia. Case
physicians . We present a case of digoxin toxicity pre-
Report: A 66-year-old woman presented with junctional
senting with junctional tachycardia and ectopic atrial
tachycardia and ectopic atrial tachycardia. She was knownto have congestive cardiac failure on diuretic therapy. Her se-
tachycardia in an elderly patient with congestive cardiac
rum digoxin level was within the normal range (2.4 nmol/L
[normal = 1.9–2.6]) along with a normal serum potassiumlevel (3.9 mmol/L [normal = 3.5–5]). However, there was se-
vere hypomagnesemia (0.39 mmol/L [normal = 0.65–1.25])precipitating
A 66-year-old woman was referred from a health center
sponded well to intravenous magnesium therapy. Conclusion:
to the Emergency Department (ED) with a 1-day history
This case reiterates that digoxin toxicity can occur in patients
of abdominal discomfort, nausea, vomiting, and intermit-
with normal digoxin and potassium levels, and in such pa-
tent palpitations. Her past history was significant for
tients, magnesium needs to be checked and treated to prevent
diabetes, hypertension, severe left ventricular systolic
potentially life-threatening dysrhythmias.
dysfunction, and congestive cardiac failure. She was be-
ing treated for the last 6 months with anti-failure medica-
, Keywords—digoxin toxicity; hypomagnesemia; hypoka-
tions, and her current medications included furosemide
lemia; dysrhythmia
40 mg twice daily, spironolactone 25 mg once daily, di-goxin 0.125 mg once daily, carvedilol 6.25 mg twicedaily, and lisinopril 10 mg once daily, along with metfor-min and calcium supplement.
At presentation, the patient was conscious and ori-
ented with a blood pressure of 145/70 mm Hg, pulse
Digoxin toxicity can be acute, due to overdose, or
rate of 110 beats/min with no gallop, and a clear chest.
chronic, when taken for a prolonged period of time. In
Her initial electrocardiogram (ECG) done in the referral
RECEIVED: 22 January 2012; FINAL SUBMISSION RECEIVED: 17 September 2012;ACCEPTED: 22 November 2012
M. P. Raja Rao et al.
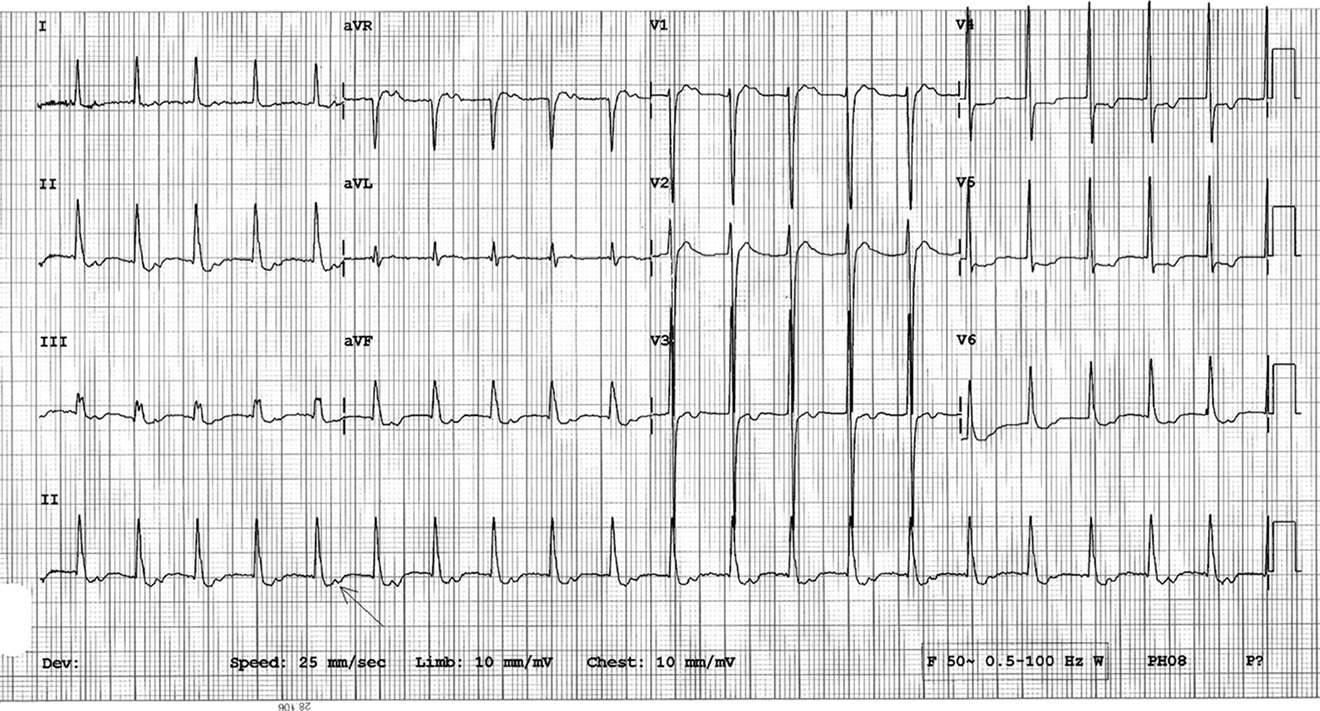
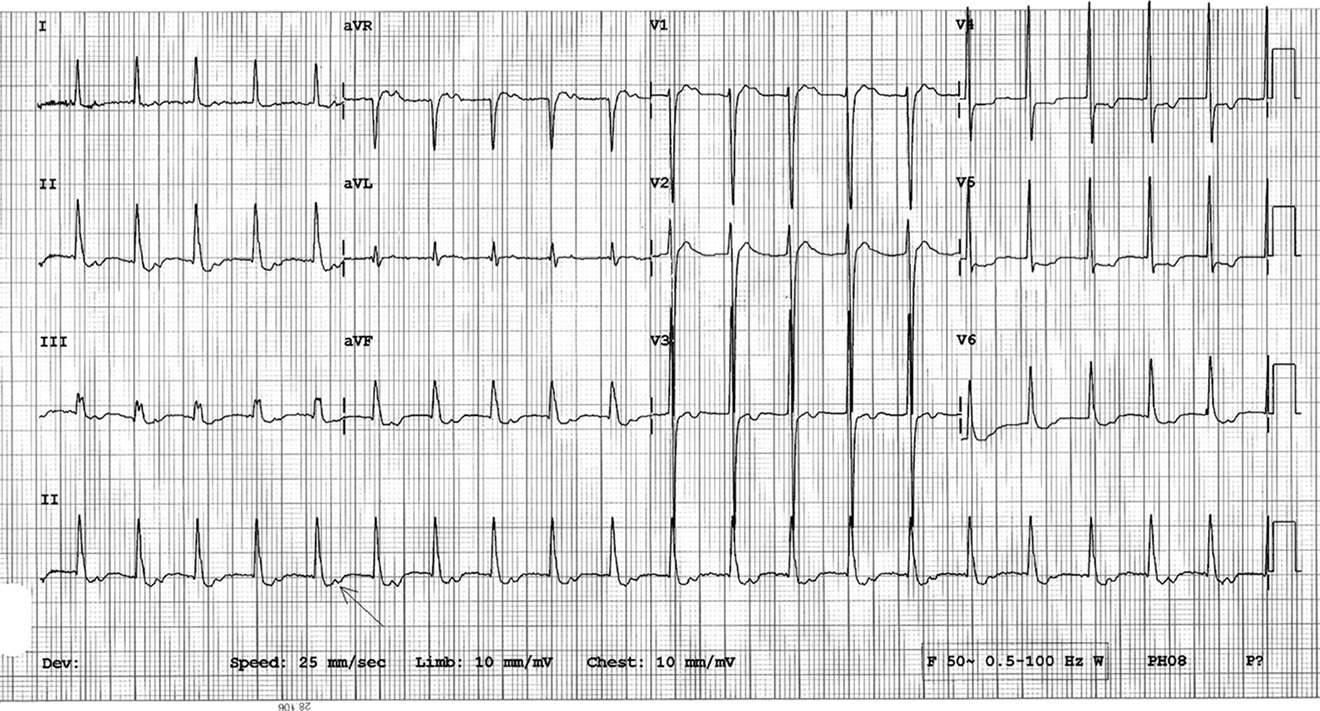
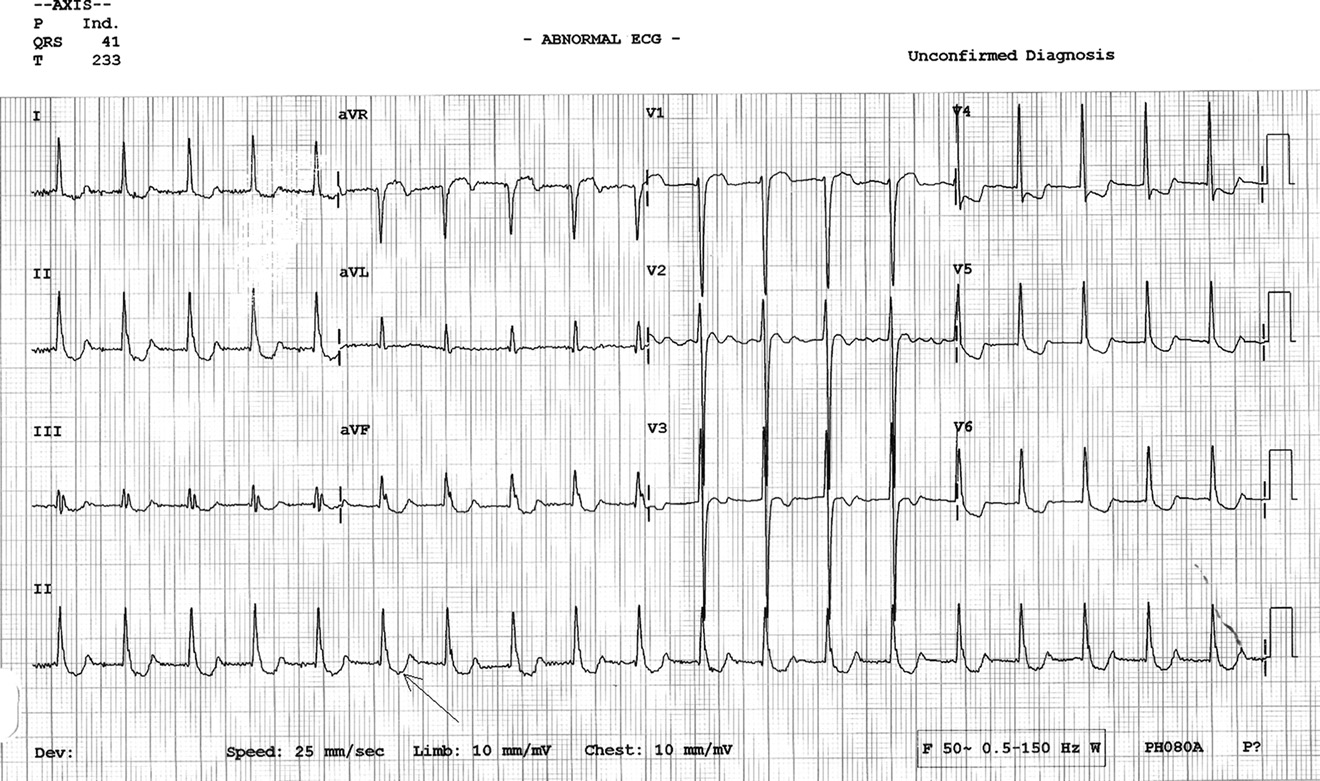
Figure 1. Twelve-lead electrocardiogram demonstrating a narrow QRS tachycardia with a heart rate of 130 beats/min with in-verted P waves falling on T waves (arrow), and upright P in aVR suggestive of a junctional tachycardia.
health center demonstrated narrow QRS tachycardia with
= 1.9–2.6] using Abbott AxSYM analyzer; Abbott Labo-
a heart rate of 130 beats/min with inverted P waves falling
ratories, Abbott Park, IL). Her troponin T was negative,
on T waves and upright P in aVR , arrowheads),
serum potassium was 3.9 mmol/L (normal = 3.5–5), cre-
suggestive of junctional tachycardia. An ECG done in our
atinine was 91 mmol/L (normal = 45–90), calculated glo-
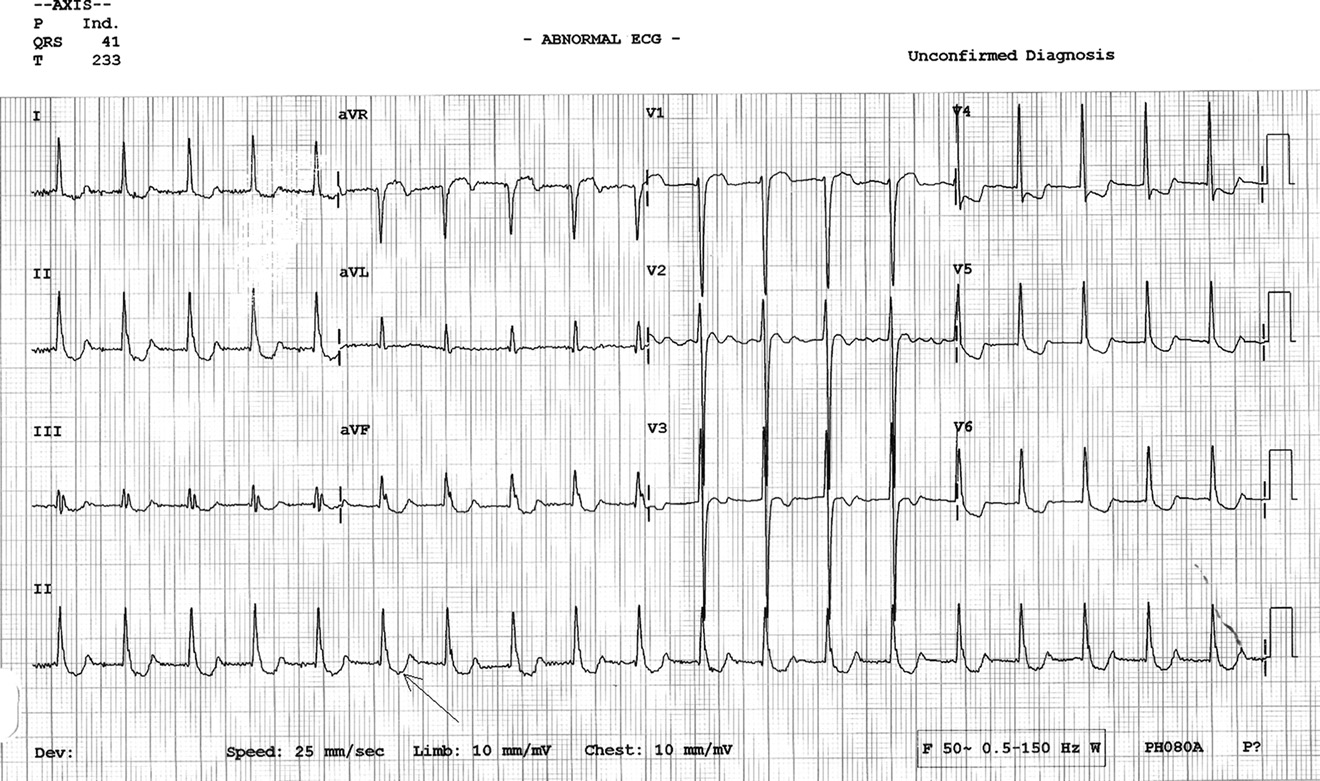
ED demonstrated a narrow QRS tachycardia, peaked P
merular filtration rate (GFR) was 54 mL/min/1.73 m2,
waves with prolonged PR interval at 110 beats/min heart
and brain natriuretic peptide was 2017 pg/mL (normal
rate, and typical ECG signs of the ‘‘digoxin effect'' in the
= 20–285). These results initially ruled out digoxin toxic-
form of a scooped appearance of the asymmetric down-
ity and suggested that the dysrhythmia may be due to un-
sloping ST depression (‘‘reversed tick'' sign) ).
derlying cardiomyopathy. However, in view of the ECG
This ECG was suspicious for an ectopic atrial tachycardia
changes being highly suspicious for digoxin toxicity,
with 1:1 conduction. In view of the patient taking digoxin,
her magnesium and calcium levels were requested. The
she was suspected to have digoxin toxicity, and her blood
calcium level was normal, but the serum magnesium level
was sent for routine blood tests along with digoxin levels.
was low at 0.39 mmol/L (normal = 0.65–1.25). She was
All of the patient's blood investigations were reported as
diagnosed to have digoxin toxicity precipitated by hypo-
normal, including free digoxin level (2.4 nmol/L [normal
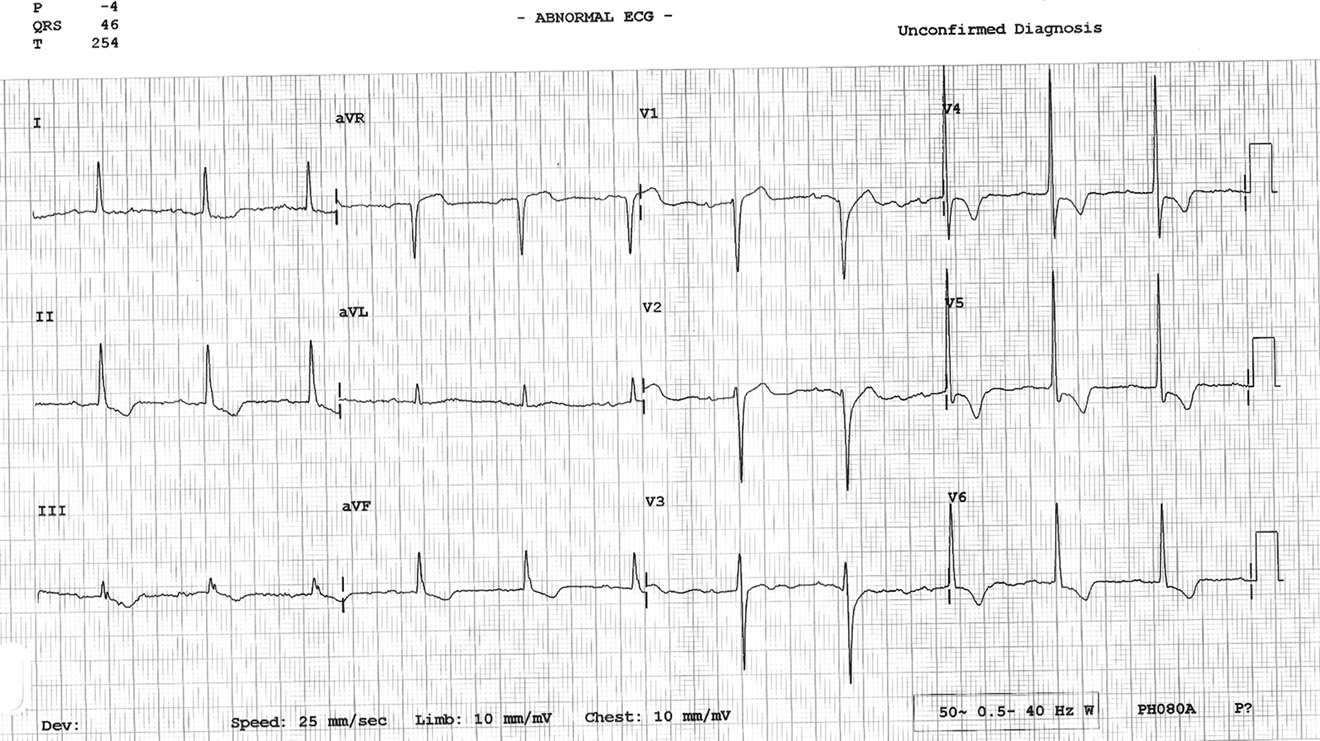
Figure 2. Twelve-lead electrocardiogram (ECG) illustrating a narrow QRS tachycardia, peaked P waves with prolonged PR inter-val at 110 beats/min heart rate, and typical ECG signs of the ‘‘digoxin effect'' in the form of a scooped appearance of the asym-metric down-sloping ST depression (‘‘reversed tick'' sign; arrow). This ECG is suggestive of an ectopic atrial tachycardia with 1:1conduction.
Magnesium and Digoxin Toxicity
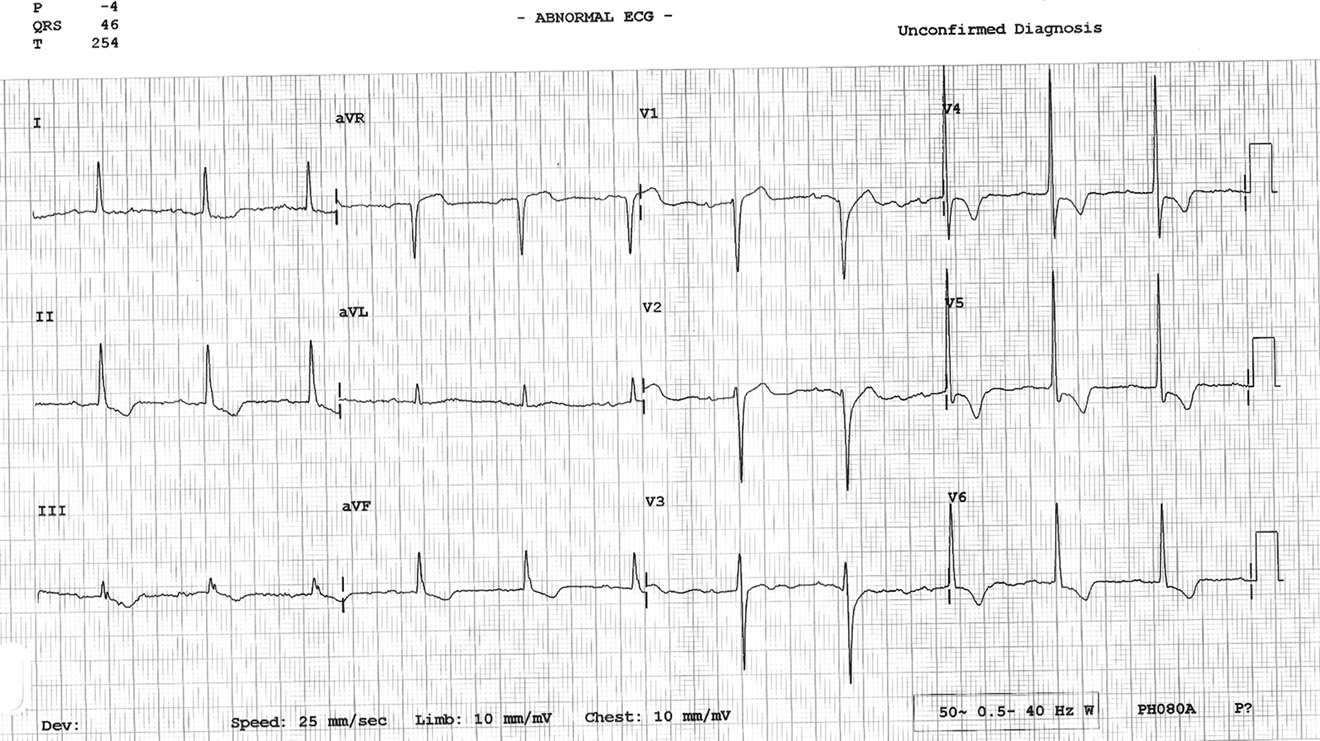
The patient was admitted and was treated with intrave-
Hypokalemia or hypomagnesemia sensitize the myo-
nous magnesium sulfate 2 g in 100 mL saline over 60
cardium to digoxin even when digoxin levels are within
min. The digoxin was discontinued. After 1 h of infusion,
the normal range (Lanoxin product information; Aspen
her rhythm changed to sinus with a heart rate of 70 beats/
Pharma, St. Leonards, NSW, Australia). Digoxin directly
min and a prolonged PR interval ). The P wave
inhibits sodium-potassium ATPase pump in the mem-
morphology was different between the second ECG and
brane of cardiac myocyte, causing an increase in intra-
third ECG, suggesting that her second ECG showed ec-
cellular sodium and calcium (through a sodium and
topic atrial tachycardia. A further magnesium sulfate in-
calcium exchanger) with subsequent increase in myocar-
fusion of 5 g (approximately 40 mEq) in 500 mL saline
dial contractility Hypokalemia increases digoxin
was given for 24 h. Repeat serum magnesium at 6 h
cardiac sensitivity because potassium and digoxin com-
was 0.67 mmol/L. Her thyroid-stimulating hormone level
pete for the same ATPase-binding site . This leads
was normal. The patient was discharged after 72 h of ob-
to a decrease in atrioventricular (AV) node conduction,
servation, with no recurrence of any dysrhythmia. At dis-
and an increase in automaticity (increased intracellular
charge, digoxin level was 1.4 nmol/L and magnesium
calcium) and ectopic pacemaker activity. In addition,
level was 1.1 mmol/L.
there is an increase in vagal tone (inhibits sodium-potassium ATPase pump in vagal afferent fibers), caus-
ing bradycardia and AV blocks. Magnesium is a cofactorof the sodium-potassium ATPase pump . Hypomagne-
In a relatively recent study, digoxin toxicity was identi-
semia increases myocardial digoxin uptake, further in-
fied in 0.04% of all admissions . The incidence rate
hibiting sodium-potassium ATPase pump activity
for digoxin toxicity-related admissions was 48 per
Hypomagnesemia is associated with hypokalemia in
100,000 prescriptions, which corresponds to 1.94 admis-
40–60% and hypocalcemia in 40% of toxicity cases
sions for toxicity per 1000 treatment-years. Women had
However, hypomagnesemia can produce intracellu-
a 1.4-fold higher risk of intoxication than men. In patients
lar potassium depletion in the presence of normal serum
taking digoxin in recommended doses (0.125 to 0.25 mg
potassium levels . It is known that long-term digoxin
once daily), digoxin toxicity can occur when they are ex-
users often have hypokalemia or hypomagnesemia, pre-
posed to precipitating factors such as hypokalemia, hypo-
sumably due to diuretic usage in patients with congestive
magnesemia, or hypothyroidism, even though the serum
heart failure .
digoxin level is within normal limits . In addition,
Even though this patient had several risk factors for di-
drug-to-drug interactions can increase digoxin level
goxin toxicity, including elderly age, female gender, and
(e.g., quinidine, verapamil, spironolactone, flecainide,
a moderately reduced GFR, it was the diuretic-induced
amiodarone, erythromycin, clarithromycin) and cause di-
hypomagnesemia that precipitated digoxin-induced junc-
goxin toxicity Furthermore, elderly age, female gen-
tional and atrial tachycardia. This patient did not manifest
der, low muscle mass, and reduced GFR can predispose to
serum hypokalemia due to the co-administration of
digoxin toxicity in patients taking a normal recommen-
a potassium-sparing diuretic and angiotensin-converting
enzyme inhibitor. However, it is possible that the
Figure 3. Twelve-lead ECG post-magnesium sulfate infusion for digoxin-induced dysrhythmia demonstrating sinus rhythm witha heart rate of 70 beats/min and prolonged PR interval with ST depression suggestive of digoxin effect.
M. P. Raja Rao et al.
hypomagnesemia was associated with intracellular potas-
sium depletion, leading to digoxin-related dysrhythmiasEnhanced automaticity and impaired conduction
This case reiterates that digoxin toxicity can occur in pa-
are the hallmarks of digitalis toxicity Digoxin can
tients with normal digoxin and potassium levels, and in
cause any type of dysrhythmia, but especially the follow-
such patients, magnesium must be monitored and treated
ing: frequent premature ventricular complexes; atrial fi-
to prevent potentially life-threatening dysrhythmias.
brillation with slow, regular ventricular rate or completeAV block; non-paroxysmal junctional tachycardia; atrial
tachycardia with block; and bidirectional ventriculartachycardia .
Normal levels of serum digoxin and the absence of hy-
pokalemia (the most common precipitant of digoxin-
induced dysrhythmias) initially led to the conclusion
that the dysrhythmias may be due to underlying cardiomy-
opathy. However, magnesium was found to be very low
and magnesium replacement resulted in conversion to si-
nus rhythm without the need for any anti-dysrhythmic
agents. Management of digoxin toxicity involves with-
drawal of the medication as well as administration of
digoxin-specific Fab antibodies for life-threatening car-
diovascular compromise . In addition, it is
necessary to treat precipitating conditions such as
replacement of electrolyte deficiencies. In the patient
presented here, treatment of hypomagnesemia resulted
in conversion of atrial tachycardia to sinus rhythm
without the need for Fab antibodies. Magnesium therapy
9. Mercader MA, Bader Y. Internet diagnosis of digitalis toxicity. BMJ
requires monitoring of serum levels and is contra-
Case Rep 2009;pii: bcr09.2008.0918, doi: 10.1136/bcr.09.2008.
0918. Epub 2009 Apr 7.
indicated in patients with bradycardia or AV block, or
severe renal failure.
Source: http://www.supplements.annemergmed.com/sites/default/files/2-SR-Rao-Digoxin.pdf
BY SZILVIA HICKMAN NATURAL SKIN CARE to prevent damage to the body diminishes the skin's structural support and decreases ANTIOXIDANTS WORK before it actually happens. its elasticity, resilience and suppleness, leads to They protect and nurture cells naturally, combating inflammation, and is the source of liver spots and poor
ENDOMINE – DIABETIC BLOOD TEST RESULTS DATA MINING PROJECT PLAN ENDOMINE DIABETIC TREATMENT KNOWLEDGE EXTRACTION FROM BLOOD TEST DATA OF JGH ENDOCRINOLOGY DEPARTMENT Projet # …. Auteur : Fodil Belghait - ETS Date of issue: Mai 7th 2013