A multicenter randomized trial indicates initial prednisolone treatment for childhood nephrotic syndrome for two months is not inferior to six-month treatment
& 2014 International Society of Nephrology
A multicenter randomized trial indicates initialprednisolone treatment for childhood nephroticsyndrome for two months is not inferior tosix-month treatmentNorishige Yoshikawa1, Koichi Nakanishi1, Mayumi Sako2, Mari S. Oba3, Rintaro Mori4, Erika Ota4,Kenji Ishikura5, Hiroshi Hataya5, Masataka Honda5, Shuichi Ito6, Yuko Shima1, Hiroshi Kaito7,Kandai Nozu7, Hidefumi Nakamura2, Takashi Igarashi8, Yasuo Ohashi9 and Kazumoto Iijima7; for theJapanese Study Group of Kidney Disease in Children10
1Department of Pediatrics, Wakayama Medical University, Wakayama City, Japan; 2Division for Clinical Trials, Clinical Research Center,National Center for Child Health and Development, Tokyo, Japan; 3Department of Biostatistics and Epidemiology, Graduate Schoolof Medicine, Yokohama City University, Yokohama, Japan; 4Department of Health Policy, National Center for Child Health andDevelopment, Tokyo, Japan; 5Department of Nephrology, Tokyo Metropolitan Children's Medical Center, Tokyo, Japan; 6Departmentof Nephrology and Rheumatology, National Center for Child Health and Development, Tokyo, Japan; 7Department of Pediatrics,Kobe University Graduate School of Medicine, Kobe, Japan; 8National Center for Child Health and Development, Tokyo, Japan and9Department of Biostatistics, School of Public Health, The University of Tokyo, Tokyo, Japan
In this multicenter, open-label, randomized controlled trial,
to 6 months of initial therapy in terms of time to onset of
we determined whether 2-month prednisolone therapy for
frequently relapsing nephrotic syndrome.
steroid-sensitive nephrotic syndrome was inferior or not to
Kidney International advance online publication, 23 July 2014;
6-month therapy despite significantly less steroid exposure.
The primary end point was time from start of initial treatment
KEYWORDS: initial treatment; nephrotic syndrome; pediatric nephrology;
to start of frequently relapsing nephrotic syndrome. The pre-
randomized controlled trial; steroid
specified non-inferiority margin was a hazard ratio of 1.3 withone-sided significance of 5%. We randomly assigned 255children with an initial episode of steroid-sensitive nephroticsyndrome to either 2 - or 6-month treatment of which 246
Idiopathic nephrotic syndrome (NS) is a disorder affecting
were eligible for final analysis. The total prednisolone
the kidneys that is mainly characterized by high excretion of
exposure counted both initial and relapse prednisolone
protein in the urine. Pediatric idiopathic NS is understood to
treatment administered over 24 months. Median follow-up in
be the most common cause of primary glomerular diseases,
months was 36.7 in the 2-month and 38.2 in the 6-month
and it frequently occurs in infants aged 2–6 years. Most
treatment group. Time to frequent relaps was similar in both
patients are presumed to have minor glomerular abnor-
groups; however, the median was reached only in the 6-
mality. Cellular immunologic abnormalities are believed to
month group (799 days). The hazard ratio was 0.86 (90%
contribute to the condition, although its pathology remains
confidence interval, 0.64–1.16) and met the non-inferior
unknown. In Europe and the United States, two in 100,000
margin. Time to first relapse was also similar in both groups:
children will develop idiopathic NS in a single yearAn
median day 242 (2-month) and 243 (6-month). Frequency
8-week corticosteroid regimen is the standard initial treat-
and severity of adverse events were similar in both groups.
ment for children with idiopathic NS, as outlined by
Most adverse events were transient and occurred during
the International Study of Kidney Disease in Children
initial or relapse therapy. Thus, 2 months of initial
(ISKDC).Although corticosteroids induce the remission
prednisolone therapy for steroid-sensitive nephrotic
of proteinuria in more than 80% of children with idiopathic
syndrome, despite less prednisolone exposure, is not inferior
NS, B60% undergo proteinuria relapse. Previous researchhas shown that a high number of children undergo frequent
Correspondence: Norishige Yoshikawa, Department of Pediatrics, Wakayama
relapse, and corticosteroid toxicities occur after repeated
Medical University, 811-1 Kimiidera, Wakayama City 641-8510, Japan.
therapyAlthough some controlled studiesand a meta-
ashow that long-term corticosteroid treatment up to
10See appendix.
7 months maximum leads to a longer sustained remission of
Received 4 February 2014; revised 29 May 2014; accepted 5 June 2014
NS than ISKDC-recommended administration, the optimum
Kidney International
N Yoshikawa et al.: RCT for initial prednisolone in childhood NS
dose and duration of initial therapy are still unknown.
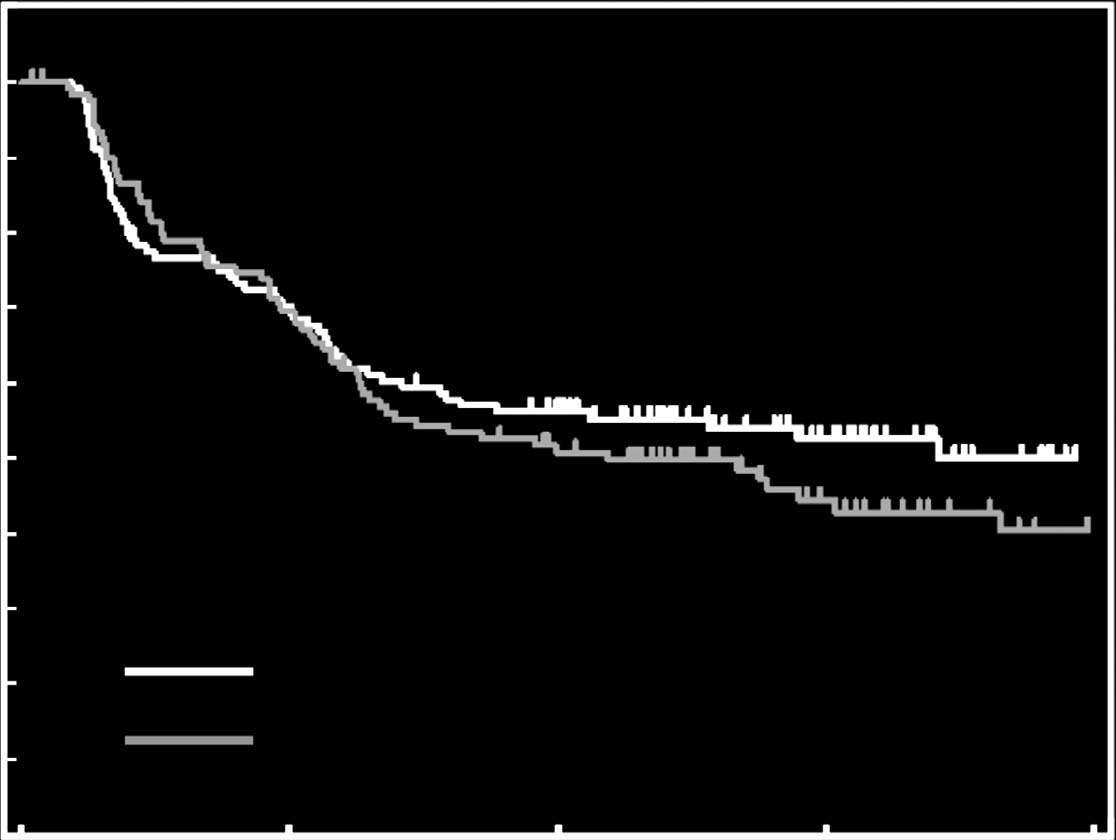
(comprising 45 FRNS [definition 1, 23; definition 2, 22],
A Cochrane review concluded that a well-designed and
and 13 requiring immunosuppressant administration).
adequately powered randomized controlled trial is required
Twenty-one patients required immunosuppressants owing
to establish the optimum dose and duration of treatme
to steroid-dependent or steroid-resistant relapse. Times to
The purpose of this study is to investigate whether 2 months
FRNS were similar in both groups: however, the median
of initial prednisolone therapy (ISKDC regimen) is not
duration of time to FRNS was reached only in the 6-month
inferior to 6 months of initial therapy with an increasing
group (at 799 days). The hazard ratio (HR) was 0.86 (90%
cumulative dose, and to compare adverse events between
confidence interval (CI), 0.64–1.16; and noninfer-
treatment regimens.
iority of the 2-month group was confirmed significantly, withan HR margin of 1.3 (P ¼ 0.01). Post-hoc analyses showed
that age groups did not affect the median duration of time to
Patient population
FRNS. The HRs (95% CI) were 0.92 (0.59–1.45), 0.86
The study was conducted from September 6, 2007 until
(0.41–1.84), and 0.74 (0.31–1.77) for the age groups 1–5 years,
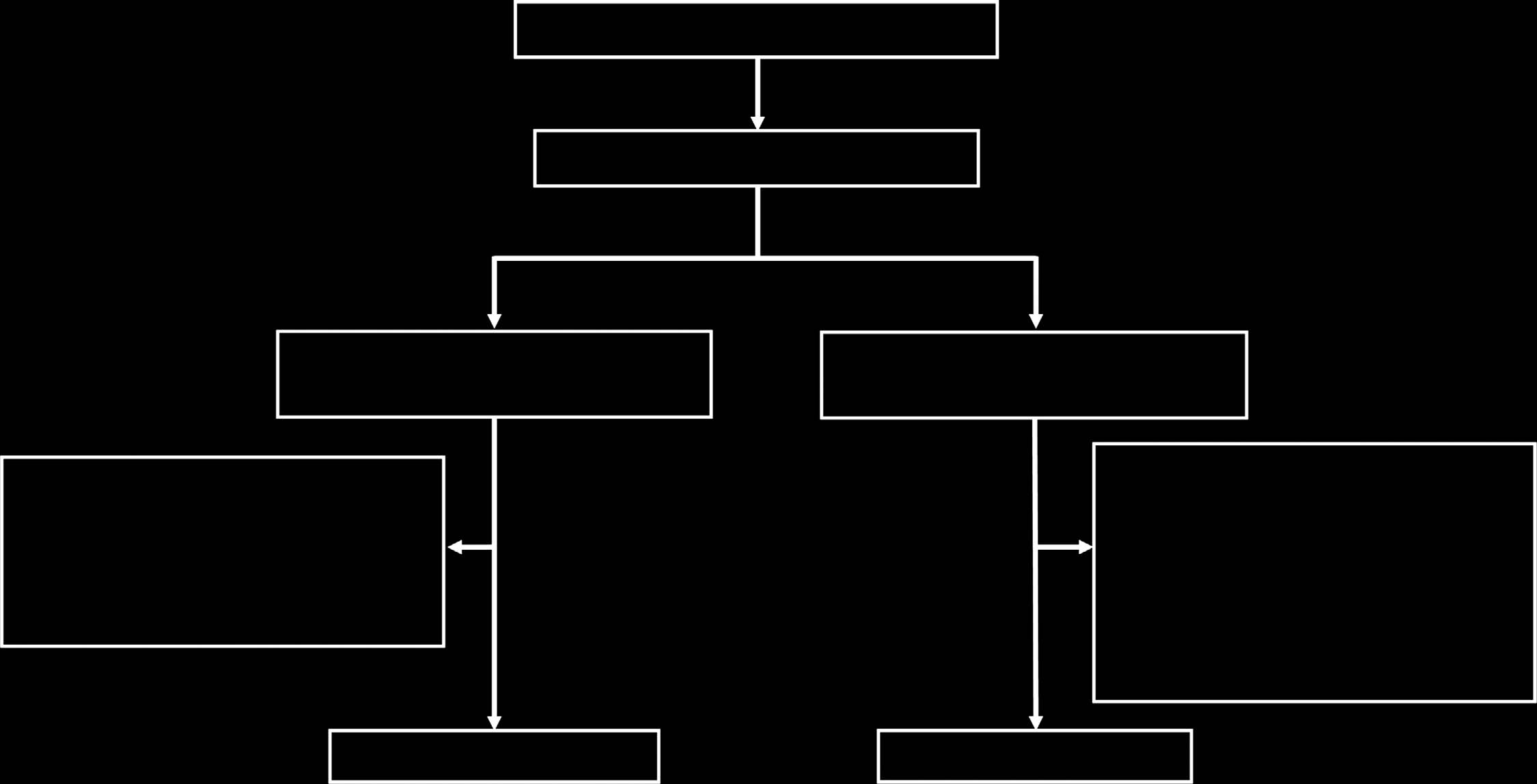
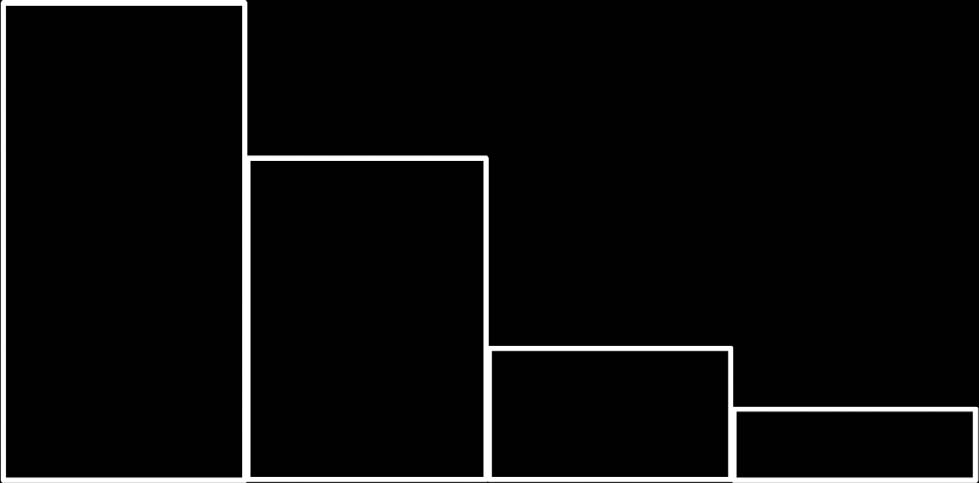
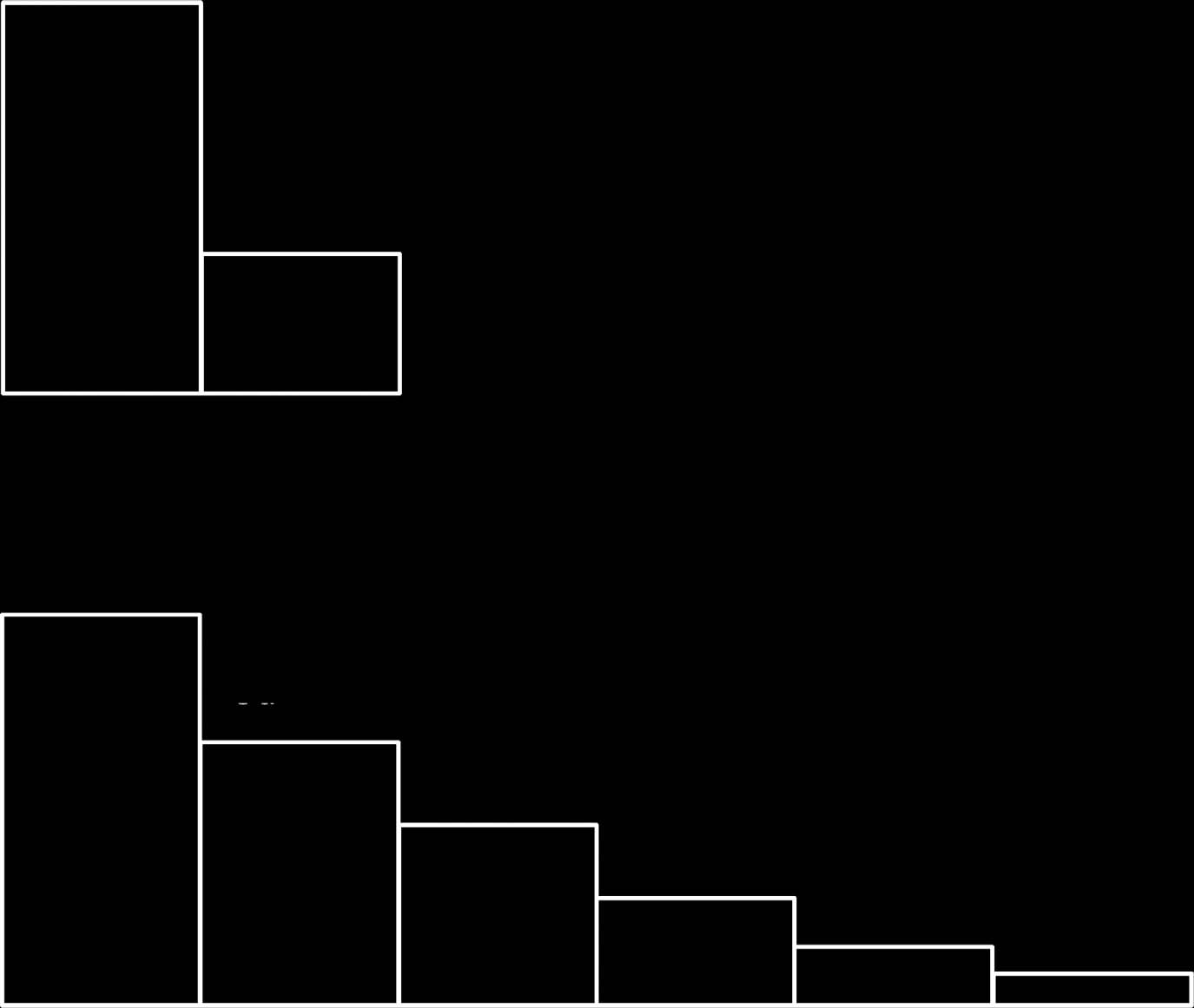
February 8, 2013. shows the trial profile. We assessed
6–10 years, and 11–15 years, respectively.
255 patients from 90 hospitals (61 general, 7 children's, and22 university hospitals) for eligibility. We randomly assigned
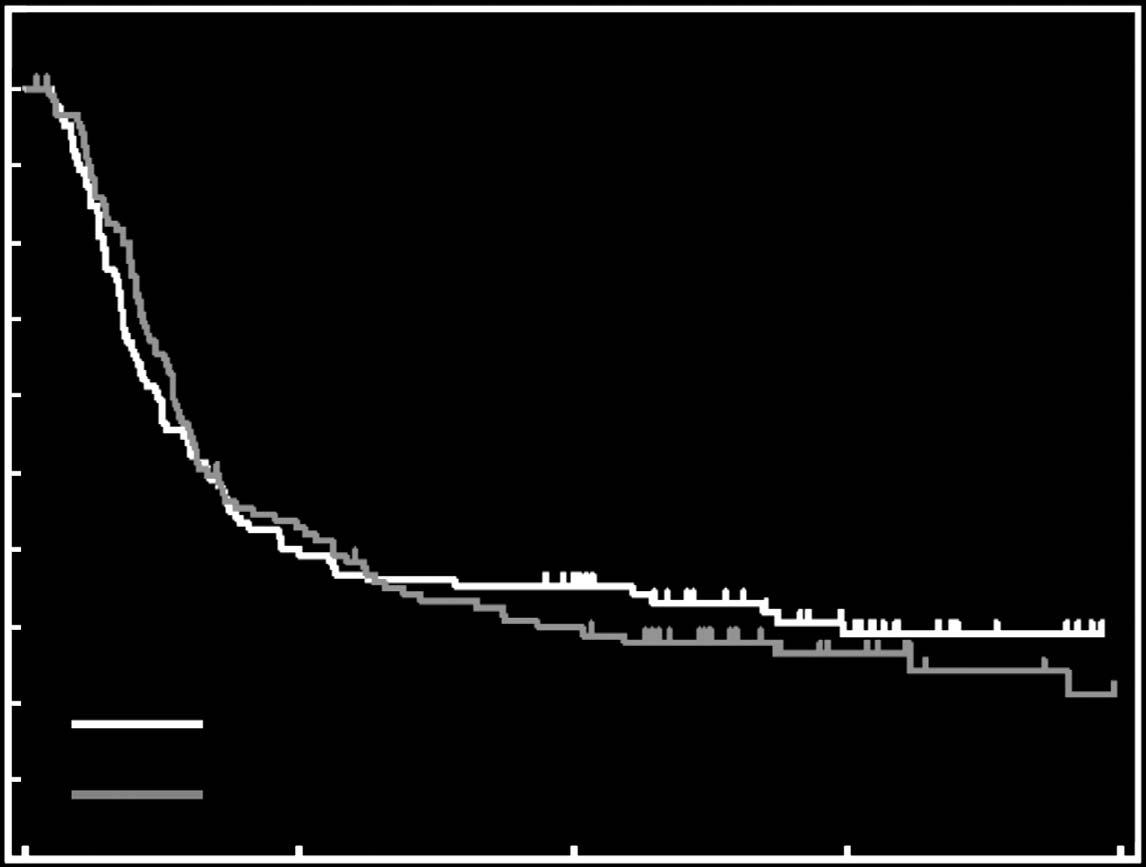
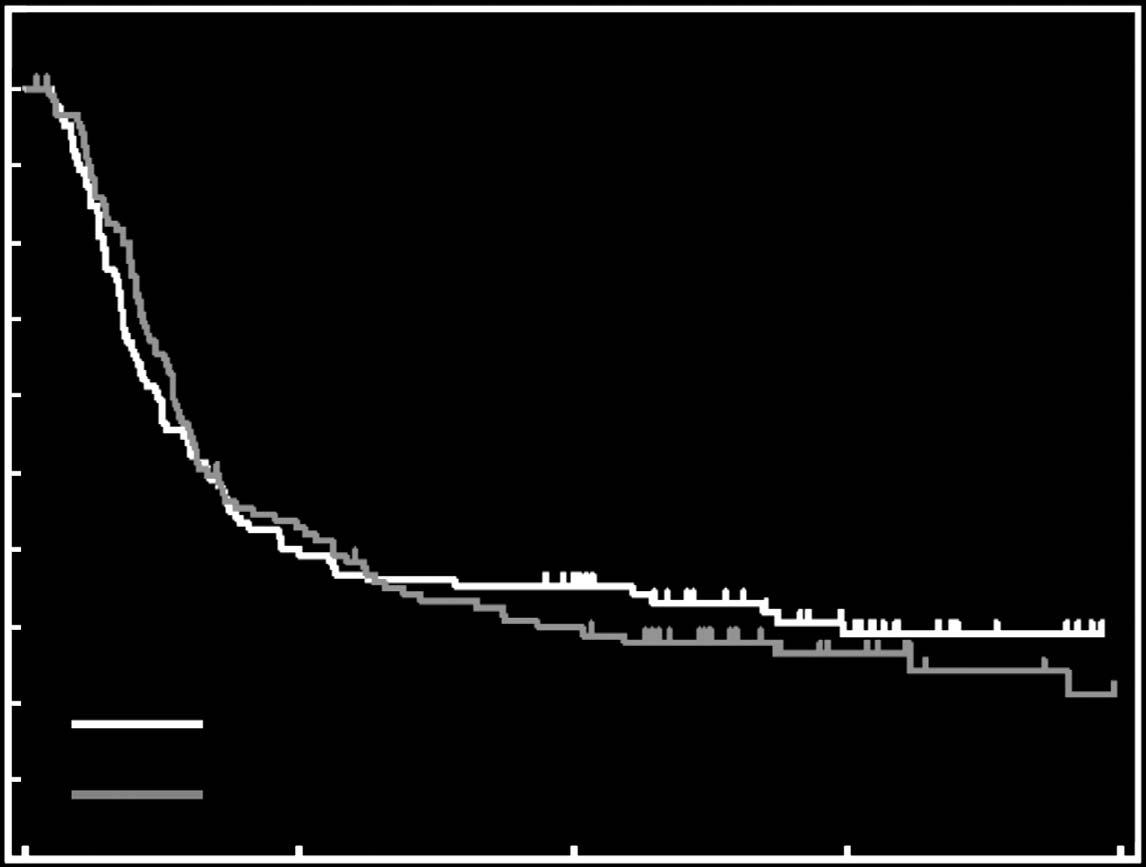
Secondary end points
128 patients to the 2-month prednisolone group and 127
Times to first relapse were similar in both groups: the median
patients to the 6-month prednisolone group. We excluded
was 242 days and 243 days in the 2-month and 6-month
nine patients from the analysis: six did not receive trial
medication because of either early relapse after remission
0.72–1.31; P ¼ 0.86; The number of relapses per
during the initial 4-week prednisolone treatment, or with-
person-year during the trial intervention period was 1.25
drawn consent, and three were excluded owing to a lack of
times in the 2-month group and 1.33 times in the 6-month
participant data. Thus, we analyzed data for 246 patients.
group, and the ratio was 0.94 (95% CI, 0.71–1.22; P ¼ 0.65,
Median follow-up was 36.7 months in the 2-month group
The median cumulative dose of prednisolone
(interquartile range 27.8–46.4 months) and 38.2 months in
during the 2-year trial period in the 2-month group was
the 6-month group (interquartile range 28.6–48.5 months).
also significantly lower than in the 6-month group (4621.9
There was no difference in characteristics between the two
[interquartile range ¼ 2191.3–7472.5] vs. 6484.8 [inter-
quartile range ¼ 3701.0–9577.9], Po0.001).
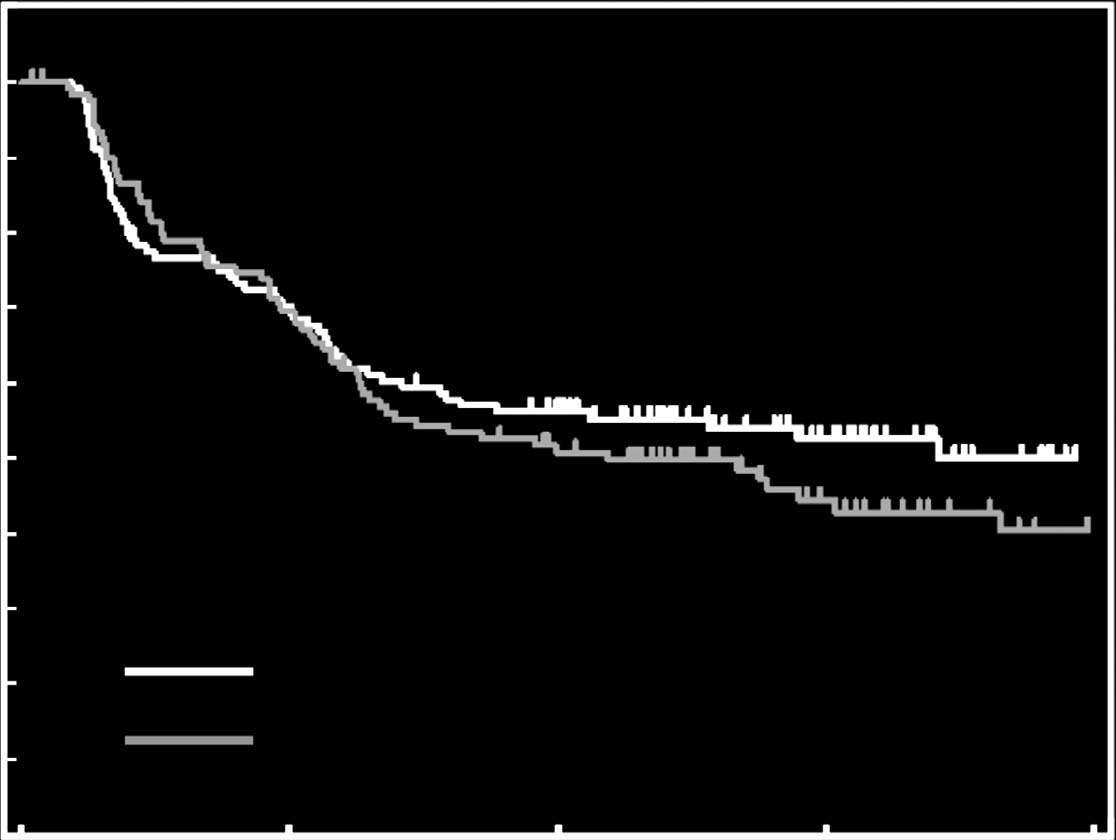
Primary end point
The primary end point was defined as the duration from
Frequency and severity of adverse events were similar in both
start of initial treatment to diagnosis of frequently relapsing
groups Most adverse events were transient and
nephrotic syndrome (FRNS), or ‘time to FRNS'. By the end
occurred during initial therapy or relapse therapy. In our
of the 24-month intervention period, we observed 54 events
study, steroid dependency did not greatly affect the occur-
in the 2-month group (comprising 46 FRNS [definition 1, 28;
rence of adverse events. Two patients in the 2-month group
definition 2, 18], and 8 requiring immunosuppressant
had severe adverse events requiring hospitalization. One
administration) and 58 events in the 6-month group
patient discontinued because of acute kidney failure during
255 Patients assessed for eligibility
255 Patients randomly assigned
128 Patients assigned to
127 Patients assigned to
2-month prednisolone
6-month prednisolone
2 Early relapse after remission
3 Early relapse after remission
during the initial 4-week
during the initial 4-week
1 Withdrew consent before
1 No follow-up data available
allocated trial medication 2 No follow-up data available
124 Patients analyzed
122 Patients analyzed
Figure 1 Trial profile.
Kidney International
N Yoshikawa et al.: RCT for initial prednisolone in childhood NS
Table 1 Baseline characteristics
2-Month prednisolone (n ¼ 124)
6-Month prednisolone (n ¼ 122)
Age, mean (s.d.), years
Blood pressure, mean (s.d.), mm Hg
Serum albumin, mean (s.d.), g/l
Quarterly distribution of disease onset, n (%)
Duration from the first episode to remission, mean (s.d.), days
Abbreviation: s.d., standard deviation.
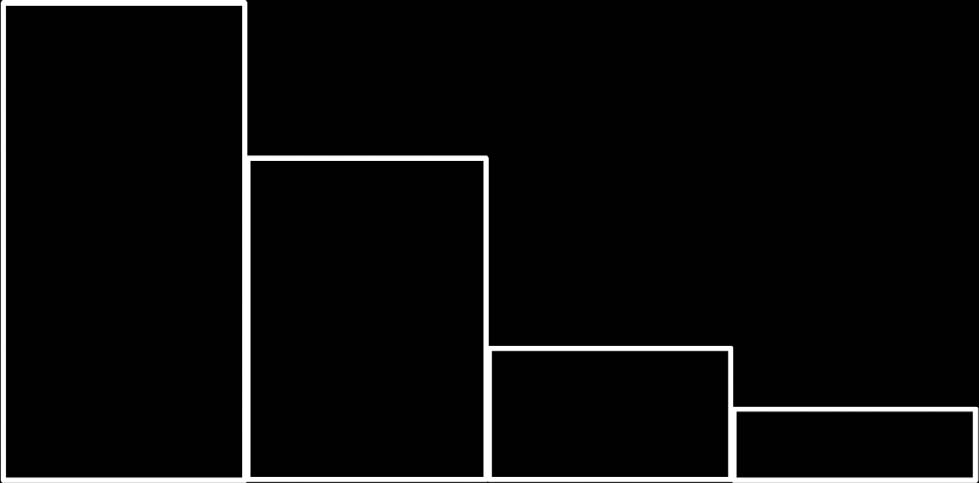
HR for FRNS: 0.86 (90% Cl, 0.64–1.16)
HR for times to first relapse: 0.97
(95% Cl, 0.72–1.31; P =0.86)
Non-inferiority with HR margin 1.3
of 2-month group: P = 0.01
Relapse-free rate 0.3
2-Month prednisolone
Non- frequent relapse rate
2-Month prednisolone
6-Month prednisolone
6-Month prednisolone
2-Month group 124
2-Month group 124
6-Month group 122
6-Month group 122
Figure 2 Kaplan–Meier estimates of time to frequently relapsingnephrotic syndrome (FRNS). HR, hazard ratio.
Figure 3 Kaplan–Meier estimates of time to first relapse.
HR, hazard ratio.
relapse (month 10) and recovered in 22 days. Another patient
of prednisolone. Symptoms disappeared on the same day of
had pneumonia with influenza infection on the last date
onset without further treatment.
of the 2-month prednisolone treatment and recovered in10 days. Height standard deviation scores show a significant
decrease in growth at 2 months of follow-up compared with
Extension of initial steroid treatment for more than 3 months
baseline (Po0.003). In both groups, this was restored within
to decrease the risk of relapse in children with steroid-
9 months after initial treatment commenced. Notably, one
sensitive (SS) NS has been widely described in previous
patient in the 6-month group was diagnosed with possible
studHowever, 80–90% of children diagnosed with
adrenal insufficiency owing to steroid withdrawal according
SSNS who are given new corticosteroid treatments continue
to clinical symptoms (mild headache and mild nausea) when
to relapse, and B50% relapse frequently.Therefore, initial
the patient switched to trial medication after the initial dose
approaches to SSNS therapy are likely to be substantially
Kidney International
N Yoshikawa et al.: RCT for initial prednisolone in childhood NS
Table 2 Number of relapses
Duration of observation
The number of relapses
Ratio of the number
(per person-year)
2-Month prednisolone
6-Month prednisolone
Abbreviation: CI, confidence interval.
Table 3 Adverse events during the 24-month trial
still required to determine the most effective duration and
intervention perioda
dosage regimen for initial SSNS.
A key strength of our trial is its unique design. This is a
multicenter, randomized, controlled trial for noninferiority
that compares the efficacy of the 2-month ISKDC regimen
with a 6-month, long-term prednisolone regimen. The mostimportant clinical objective of initial treatment of SSNS is to
Cushingoid appearance
prevent frequent relapses. Consequently, the primary end
Cushing (moon face)b
point was set to time to FRNS rather than initial relapses.
Our data from several analyses consistently support
Adrenal insufficiency
noninferiority of the ISKDC regimen. In the current trial, aHR threshold of 1.3 for noninferiority of the primary end
point is slightly high given the feasible study size. However,
the posterior probability that a HR would be smaller than1.1 and 1.2 (HRs that are commonly used as an upper
Severe infections
equivalence margin) was 91 and 97%, respectively.
In our trial, noninferiority was found in FRNS (primary
Acute kidney failurec
end point) and first relapse (secondary end point) between
the ISKDC and 6-month regimens. This means that manypatients relapse even while taking tapering-dose prednisolone
Increased laboratory data
(Previous studies vary in their observation of
(frequent) relapses from either the start or end of initial
therapyHowever, if analyses are performed from the end
Abbreviations: AST, aspartate aminotransferase; ALT, alanine aminotransferase.
a
of initial therapy, relapses during tapering-dose prednisolone
Data are expressed as the number of events.
bMultiple reports were recorded for these adverse events.
cannot be counted, possibly resulting in an inadequate
cSevere adverse events requiring hospitalization.
interpretation. Therefore, we selected observations primarilyfrom the start of initial therapy. In our study design, steroid-dependent NS was predicted to occur more frequentlybecause of its definition in the 6-month regimen. This is
different.Our results demonstrate that extending initial
one reason why we selected FRNS as a primary end point,
steroid treatment, and even increasing the total dose of
and not steroid-dependent NS. In fact, time to steroid-
prednisolone (2240 vs. 3885 mg/m2), does not improve
dependent NS was significantly higher in the ISKDC regimen
clinical outcomes (time to FRNS, time to first relapse, the
group (data not shown).
number of relapses, total prednisolone dose, and adverse
No significant difference in adverse events was observed
events) for pediatric NS. Our results add to the Cochrane
between the two regimens in our large-scale trial, which is a
review by Hodgson et al.by comparing treatment regimens
similar finding to previous small-scale Most adverse
of 2 vs. 6 months.
events were transient and occurred during initial or relapse
Our findings build on a 2013 study from the Netherlands.
therapy. However, because the ISKDC regimen is generally
This well-designed, randomized, double-blind, placebo-con-
less likely to cause adverse events owing to the lower dosage
trolled trial of children with NS clearly showed no
and the shorter duration, its use can be recommended.
improvement in clinical outcomes when the initial predni-
A limitation of our trial is the open-label design, which
solone treatment was extended from 3 to 6 months without
may have introduced preconception bias. However, as our
an increasing cumulative dose.However, despite the results
trial design is a noninferiority trial with regular visits, and
of this trial, the most effective duration and dosage of
relapses are measured objectively, we cannot assume positive
prednisolone treatment for an initial episode of SSNS is still
placebo effects. Therefore, the open-label design of this study
under debate.Although our study has demonstrated that
may have limited impact on preconception bias. Moreover,
increasing the total dose in 2-month or 6-month regimens
the results of this trial may partially be due to the relatively
does not improve clinical outcomes, further investigation is
high rate of relapse compared with other studies.The high
Kidney International
N Yoshikawa et al.: RCT for initial prednisolone in childhood NS
rate of relapse may be owing to our definition of relapse
and the Declaration of Istanbul, and adhered to the International
(proteinuria 2 þ or higher). It still remains unknown
Conference on Harmonisation Guidelines on Good Clinical
whether long prednisolone therapy consisting of a dose of
60 mg/m2 per day for 6 weeks, followed by alternate-daydoses of 40 mg/m2 per 2 days for 6 weeks, is more effective
against time to FRNS compared with the ISKDC regimen
Patients were randomly assigned to either the 2-month or 6-month
for treating idiopathic NS. In our study, only one patient
group in a 1:1 ratio at the Japan Clinical Research Support Unit. We
withdrew consent. A low rate of consent withdrawal is
applied a minimization method using a computer-generated
common in Japan.Cultural differences between countries
sequence (SAS PROC PLAN) with age (1–10 years or 11–15 years),sex, and institution as adjustment (stratification) factors. Patients,
may account for variations in rates of consent withdrawal.
patients' guardians, treating physicians, and individuals assessing
In our study, steroid sensitivity was confirmed by day 21
outcomes and analyzing data were not blinded to the patients'
in order to ensure time for eligibility screening. Generally,
treatment assignments. Apart from the trial statistician and the
remission after 3 weeks is uncommon.Therefore, as the
data-monitoring committee, all treating physicians and other
effect of early confirmation of steroid sensitivity was slight,
investigators remained blinded to the trial results until follow-up
we decided to confirm steroid sensitivity by day 21.
was completed.
We conducted a meta-analysis to address the differences
between corticosteroid regimens in children with an initial
episode of SSNS. We searched randomized controlled trials
The first patient was randomized in September 2007, and the last
that compared durations of steroid therapy in children and
patient in January 2011. Follow-up started at diagnosis and was
reported the number of FRNS cases within 2 years (see the
truncated when the last enrolled patients finished the 24-month
Supplementary Information online for a detailed search
strategy). Meta-analysis of our study and five stud
All patients diagnosed with a first episode of idiopathic NS
showed a risk ratio (long vs short) of 0.99 (95% CI,
started initial therapy of 60 mg/m2 oral prednisolone in three
0.68–1.44, see Supplementary Figure 2A online), whereas
divided doses (maximum of 80 mg/day) daily for 4 weeks. Patientsunderwent a screening examination and were registered after their
meta-analysis of our study and the published studies only
eligibility, including remission, was verified. Participants switched to
showed an risk ratio of 1.15 (95% CI: 0.95–1.40, Supple-
trial medication after initial doses of prednisolone were given
mentary Figure 2B online). This result might indicate that
If participants relapsed after remission during the initial
long-term treatment is not superior but almost equivalent to
4-week prednisolone treatment, they were excluded.
Trial medication consisted of initial treatment regimens and
In conclusion, our study shows that extending initial
relapse treatment, and was completed within a total of 24 months in
prednisolone treatment from 2 to 6 months with an increas-
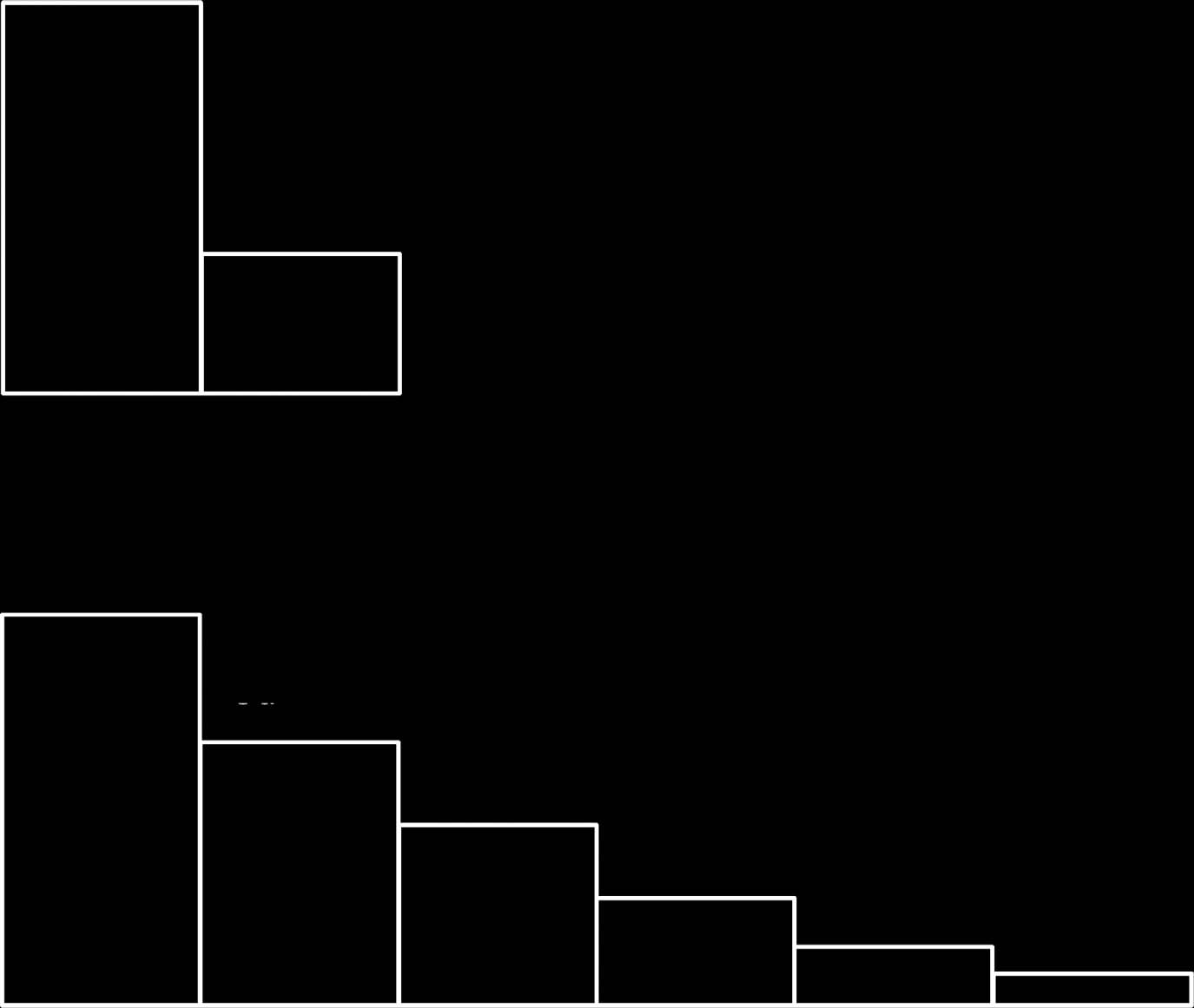
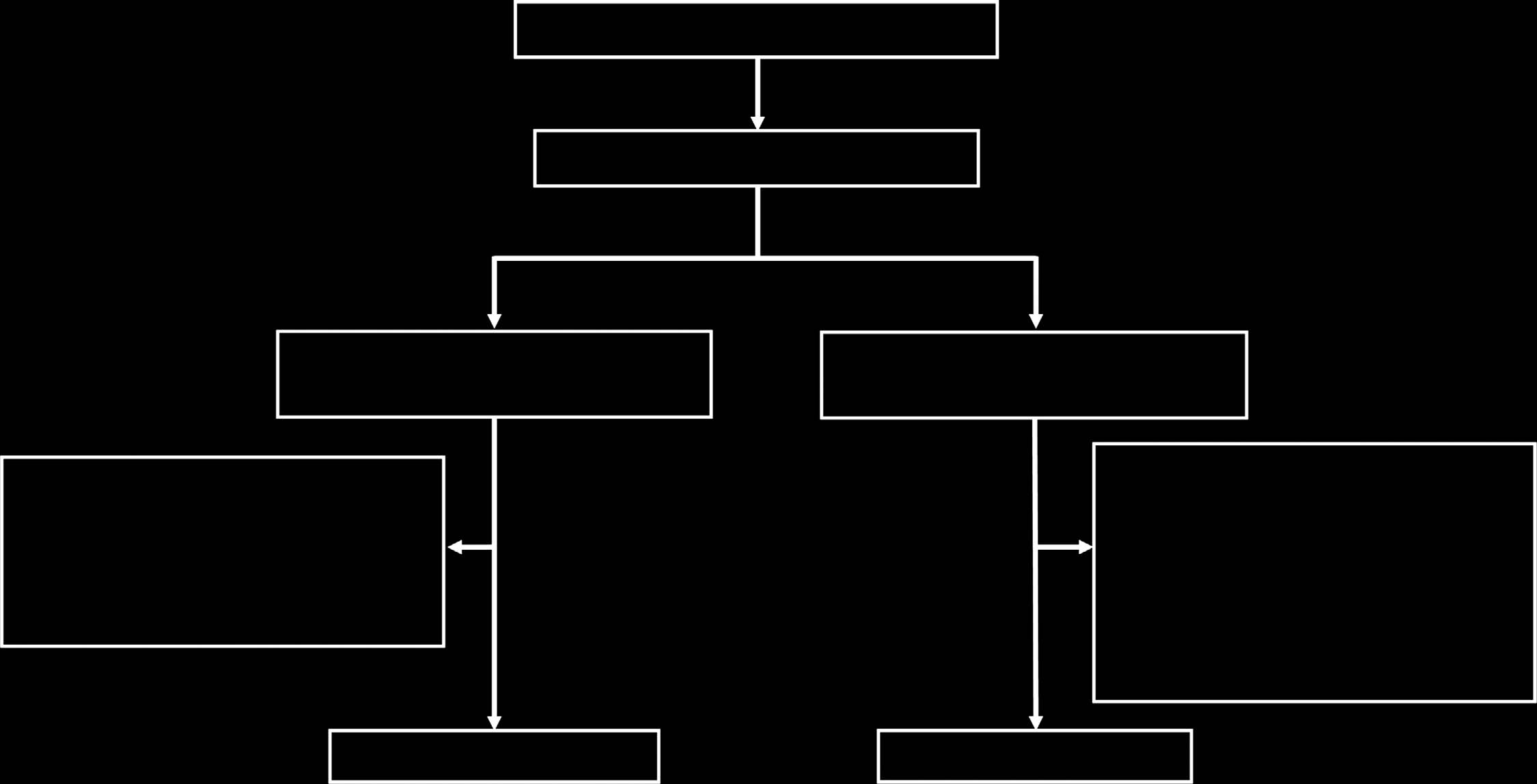
both groups and 5). The duration of long-term
ing dose does not improve clinical outcomes for pediatric NS.
prednisolone treatment was set to 6 months, which is consistent
The original ISKDC regimen is not inferior to 6 months of
with recommendations from a non-Japanese randomized controlled
initial therapy with an increasing cumulative dose. We assert
The cumulative dose of initial treatment was 2240 mg/m2
that the ISKDC regimen is recommended as an initial
(2-month group) and 3885 mg/m2 (6-month group). Participants
treatment for pediatric idiopathic NS.
2-Month prednisolone
Cumulative dose: 2240 mg
MATERIALS AND METHODSStudy design and patientsWe conducted a multicenter, randomized, noninferiority, open-labeltrial at 90 hospitals in Japan and compared prednisolone treatmentof 2 months (ISKDC regimen) with 6 months for children witha first episode of idiopathic NS. We diagnosed idiopathic NS and
remission according to the ISKDC.NS was defined as a urinary
protein–creatinine ratio X1.8 and albumin levels p25 g/l in serum.
Remission was defined as a negative dipstick analysis for 3
6-Month prednisolone
consecutive days. Patients aged 1–15 years with a first episode of
Cumulative dose: 3885 mg
idiopathic NS were eligible if they had remission within 3 weeks ofprednisolone administration. Patients were ineligible if they hadsecondary NS, renal insufficiency defined as creatinine clearance ofp60 ml/min per 1.73 m2, active infections, poorly controlledhypertension, severe liver dysfunction, pregnancy, or a history ofimmunosuppressant administration.
Before enrollment, patients' guardians provided written in-
formed consent, and informed assent was obtained from older
children. This study was approved by the institutional review boards
Figure 4 Initial treatment regimens. Upper doses are in mg/m2
of participating hospitals, complied with the Declaration of Helsinki
per day. Maximum doses are in mg/day. D, daily; AD, alternate days.
Kidney International
N Yoshikawa et al.: RCT for initial prednisolone in childhood NS
Basic regimen for relapse in
secondary end points were time to first relapse, the number of
2-month group and relapse at no
relapses per person-year, total prednisolone dose, and adverse events.
prednisolone in 6-month group
Statistical analysesThe primary objective of this trial was to confirm noninferiority ofinitial therapy with 2-month treatment compared with 6-monthtreatment, with respect to time to FRNS. The noninferiority marginof HR for the 2-month to 6-month group was predefined to 1.3, and
the significance level was set to 5% (one-sided). The former
was determined based on surveys conducted among practicing
pediatric nephrologists and other specialists before the protocol was
Figure 5 Treatment regimens for relapse. aUntil urinary protein is
negative on 3 consecutive days using a urine dipstick test. Upper
On the basis of results from a previous study,we assumed an
doses are in mg/m2/day. A maximum dose of each is the same as
event rate of 15 and 19% at 1 year in the 2- and 6-month groups,
initial treatments in AD, alternate days; D, daily.
respectively. With a sample size of 125 patients in each treatmentgroup, an HR test with a one-sided 5% significance level would have70% power to confirm noninferiority. Accrual and follow-up times
who relapsed during the 24-month trial medication period received
were specified to be 3 and 2 years, respectively.
relapse treatment regimens Relapse treatment was the
As the previous studywas conducted more than 10 years
same in both groups. However, relapse treatment given during the
earlier, it is possible that the current event rate of our study is lower
6-month initial treatment was adjusted according to the initial
than the previous study. We scheduled an interim analysis to take
treatment regimen in the 6-month group.
place just before the accrual completion date, which was performed
Participant characteristics (age, sex, physical characteristics,
in October 2010. A statistical test regarding the primary end point
blood, and urine test results) were recorded at baseline. Clinical
was not performed. The number of events observed matched that of
assessment and urine tests (urinalysis, qualitative and quantitative
the assumption, and the study plan was not changed.
proteinuria, quantitative creatinine) were performed at 1, 2, 4, and 6
Statistical analyses followed the protocol and the intention-
months after enrollment and every 3 months thereafter, and also on
to-treat principle. The Cox proportional hazard model was used
diagnosis of relapse. Blood analysis (complete blood cell count,
to test noninferiority and estimate the HR with a 90% CI of the
blood chemistry) was performed at 1, 2, 6, and 12 months after
primary end point. The Kaplan–Meier method was used to
enrollment, at the end of treatment, and at diagnosis of relapse only.
summarize time to FRNS. These methods and the log-rank test
Adverse events were recorded throughout the trial period and
were used to analyze time to first relapse. The number of relapses
assessed using Common Terminology Criteria for Adverse Events
per person-year was calculated as the total number of relapses
v3.0. Within 4 weeks of starting initial treatment, participants were
divided by the total observed person-years in each treatment group
screened for glaucoma by an ophthalmologist. Details about
A permutation test was used to compare the number of
monitoring adverse events are described in the Supplementary
relapses per person-year between groups. We compared the
Information online. Briefly, name of diagnosis, severity, seriousness,
prednisolone total dose using the Wilcoxon test. The number of
date of onset and disappearance, outcome, and assessment of causal
adverse events was compared using Poisson regression. For baseline
relationship to the study drug were investigated at the start of study
characteristics, we compared distributions of continuous variables
treatment and at 1, 2, 4, 6, 9, 12, 15, 18, 21, and 24 months after the
between groups using the t-test or Wilcoxon test, depending on the
start of study treatment (each within ±2 weeks).
shape of the distribution. We analyzed categorical variables using thechi-squared test or Fisher's exact test. Posterior probability wascalculated with the improper flat prior and the normal distribution
to which log-HR was approximated. Except for noninferiority
The primary end point was defined as the duration from start of
testing of the primary end point, we regarded a two-sided P-value
initial treatment to diagnosis of FRNS, or ‘time to FRNS'. Diagnosis
o0.05 to indicate statistical significance. We analyzed data using
of FRNS was based on the relapse dates according to the ISKDC.
SAS software (version 9.3) and calculated the sample size using the
In our study, FRNS was defined as two relapses within 6 months
SAS POWER procedure.
of initial remission (definition 1), or four relapses within any12-month period (definition 2), which included relapses during
initial tapering treatment but excluded relapses with spontaneous
This study was supported by a grant from the Ministry of Health,
remissions. Patients were observed for at least 2 years, on the basis of
Labour and Welfare, Japan. All expenses were covered by the grant.
the Cochrane review, which states that the risk of relapse after 1–2
NY has received grants from Novartis Pharma K.K. and Asahi Kasei
years was lower after long-term prednisolone treatment relative to
Pharma Corporation and has also received lecture fees from Novartis
the ISKDC Relapse was defined as proteinuria 2 þ or
Pharma K.K. and Asahi Kasei Pharma Corporation. KN has receivedlecture fees from Novartis Pharma K.K. and Asahi Kasei Pharma
higher on dipstick analysis for 3 or more consecutive days or
Corporation. KIs has received lecture fees from Novartis Pharma K.K.
proteinuria 2 þ or higher on dipstick analysis and serum albumin
HH has received lecture fees from Asahi Kasei Pharma Corporation.
p25 g/l. Immunosuppressant administration was prohibited in the
MH has received lecture fees from Novartis Pharma K.K. and Asahi
protocol. However, if administration was undertaken for clinical
Kasei Pharma Corporation. SI has received lecture fees from Novartis
necessity, e.g., steroid dependency, it was treated as an event in the
Pharma and Asahi Kasei Pharma Corporation. YS has received lecture
primary analysis. Data for patients who did not experience these
fees from Novartis Pharma K.K. HN owns stocks in Asahi Kasei Pharma
events were considered censored at the last examination. Important
Corporation. TI has received lecture fees from Takeda Pharmaceutical,
Kidney International
N Yoshikawa et al.: RCT for initial prednisolone in childhood NS
K.K. KIi has received grants from Takeda Pharmaceutical Co., Ltd.,
relapsing nephrotic syndrome in children: a multicenter randomized
Asahi Kasei Pharma Corporation, and Novartis Pharma K.K., and
phase II trial. Clin J Am Soc Nephrol 2014; 9: 271–278.
lecture fees from Novartis Pharma K.K. and Asahi Kasei Pharma
Kobayashi T, Saji T, Otani T et al. RAISE study group investigators. Efficacyof immunoglobulin plus prednisolone for prevention of coronary artery
Corporation. No other disclosures were reported.
abnormalities in severe Kawasaki disease (RAISE study): a randomised,open-label, blinded-endpoints trial. Lancet 2012; 379: 1613–1620.
Nakanishi K, Iijima K, Ishikura K et al. Two-year outcome of the ISKDC
We thank all our patients, their families, and the site investigators. We
regimen and frequent-relapsing risk in children with idiopathic nephrotic
thank Emma Barber for editing the article. We thank Drs Jonathan
syndrome. Clin J Am Soc Nephrol 2013; 8: 756–762.
Craig, Patrick Niaudet, and Tohru Kobayashi for their helpful advice.
Mishra OP, Thakur N, Mishra RN et al. Prolonged versus standardprednisolone therapy for initial episode of idiopathic nephrotic
The trial was supported by a grant from the Ministry of Health,
syndrome. J Nephrol 2012; 25: 394–400.
Labour and Welfare, Japan (H19-shouni-002). The results of this trial
Hiraoka M, Tsukahara H, Matsubara K et al. A randomized study of two
were presented in abstract form at the annual meeting of the
long-course prednisolone regimens for nephrotic syndrome in children.
American Society of Nephrology, November 7–10, 2013, Atlanta, USA.
Am J Kidney Dis 2003; 4: 1155–1162.
This trial is registered at the University Hospital Medical Information
Yoshikawa N, Ito H, Takehoshi Y et al. Standard versus long-term
Network clinical trial registry (UMIN-CTR) (
prednisolone with Sairei-to in childhood steroid-responsive nephrotic
registration number UMIN000000747. See the Supplementary
syndrome: a prospective controlled study. Jpn J Nephrol 1998; 40:587–590.
Information online for complete Methods (Clinical Study Protocol).
SUPPLEMENTARY MATERIAL
Figure S2. (A) Meta-analysis of studies comparing 2–3 months
Japanese Study Group of Kidney Disease in Children (JSKDC).
of prednisolone to 5–6 months of prednisolone for children with
JSKDC has been supported by grants from the Ministry of
their first episode of nephrotic syndrome, with an outcome showing
Health, Labour and Welfare, Japan. Members of the JSKDC
the number of children with frequent relapses after 1–2 years.
(B) Sensitivity analysis excluding Sharma 2002 (unpublished
are as follows.
conference proceeding) from Fig. A.
Steering Committee: Norishige Yoshikawa (chair), Kazumoto
Supplementary material is linked to the online version of the paper at
Iijima, Hidefumi Nakamura, Masataka Honda, and Mayumi
JSKDC study office: Koichi Nakanishi (chair) and Yuko
Schlesinger ER, Sultz HA, Mosher WE et al. The nephrotic syndrome: itsincidence and implications for the community. Am J Dis Child 1968; 116:
Data Coordinating Center: Yasuo Ohashi (chair).
Statistical Center: Mari S Oba (chair).
van Husen M, Kemper MJ. New therapies in steroid-sensitive and steroid-
Data and Safety Monitoring Board: Takashi Igarashi, Yasuo
resistant idiopathic nephrotic syndrome. Pediatr Nephrol 2011; 26:881–892.
Ohashi, Tetsuya Kawamura, and Michio Nagata.
Tarshish P, Tobin JN, Bernstein J et al. Prognostic significance of the early
Clinical Investigators (Institution): Satoshi Sasaki (Hokkai-
course of minimal change nephrotic syndrome: report of theInternational Study of Kidney Disease in Children. J Am Soc Nephrol 1997;
do University Hospital), Yutaka Yamada (Hakodate Central
8: 769–776.
General Hospital), Tetsuro Nagashima (Kushiro Red Cross
Ueda N, Chihara M, Kawaguchi S et al. Intermittent versus long-term
Hospital), Yoshinori Saita (Japanese Red Cross Kitami
tapering prednisolone for initial therapy in children with idiopathicnephrotic syndrome. J Pediatr 1988; 112: 122–126.
Hospital), Tetsuji Morimoto (Tohoku University Hospital),
Ehrich JH, Brodehl J. Long versus standard prednisone therapy for initial
Yohei Ikezumi (Niigata University Medical & Dental
treatment of idiopathic nephrotic syndrome in children.
Hospital), Toshio Yanagihara (Niigata Prefecture Yoshida
Arbeitsgemeinschaft fu¨r Pa¨diatrische Nephrologie. Eur J Pediatr 1993;152: 357–361.
Hospital), Noriko Oonishi (Fujita General Hospital), Tomoko
Ksiazek J, Wyszyn´ska T. Short versus long initial prednisone treatment in
Sato (Jusendo General Hospital), Kenji Nemoto (Shirakawa
steroid-sensitive nephrotic syndrome in children. Acta Paediatr 1995; 84:889–893.
Kosei General Hospital), Katsutoshi Nagasawa (Takeda
Bagga A, Hari P, Srivastava RN. Prolonged versus standard prednisolone
General Hospital), Masahiko Katayose (Public Soma General
therapy for initial episode of nephrotic syndrome. Pediatr Nephrol 1999;
Hospital), Yoshiyuki Namai (Ohta General Nishinouchi
13: 824–827.
Hodson EM, Willis NS, Craig JC. Corticosteroid therapy for nephrotic
Hospital), Shigeo Suzuki (Ohara General Hospital), Yasuaki
syndrome in children. Cochrane Database Syst Rev 2010; 4: CD001533.
Kobayashi (Japanese Red Cross Ashikaga Hospital), Yoko
Hodson EM, Alexander SI. Evaluation and management of steroid-
Owada (Dokkyo Medical University Hospital), Hideaki
sensitive nephrotic syndrome. Curr Opin Pediatr 2008; 20: 145–150.
Hodson EM, Craig JC, Willis NS. Evidence-based management of steroid-
Kurayama (National Hospital Organization Chiba-East-Hos-
sensitive nephrotic syndrome. Pediatr Nephrol 2005; 20: 1523–1530.
pital), Shuichiro Fujinaga (Saitama Children's Medical
Hodson EM, Willis NS, Craig JC. Non-corticosteroid treatment fornephrotic syndrome in children. Cochrane Database Syst Rev 2008; 23:
Center), Midori Awazu (Keio University Hospital), Hirotaka
Takahashi (Tokyo Metropolitan Ohtsuka Hospital), Shori
MacHardy N, Miles PV, Massengill SF et al. Management patterns of
Takahashi (Surugadai Nihon University Hospital), Motoshi
childhood-onset nephrotic syndrome. Pediatr Nephrol 2009; 24:2193–2201.
Hattutori (Tokyo Women's Medical University Hospital),
Teeninga N, Kist-van Holthe J, van Rijskwijk N et al. Extending
Shuichi Ito and Koichi Kamei (National Center for Child
prednisolone therapy does not reduce relapse in childhood nephrotic
Health and Development), Masayasu Ohta (Toride Kyodo
syndrome. J Am Soc Nephrol 2013; 24: 149–159.
Hodson EM, Craig JC. Corticosteroid therapy for steroid-sensitive
General Hospital), Tae Omori (Tokyo Metropolitan Bokutoh
nephrotic syndrome in children: dose or duration? J Am Soc Nephrol 2013;
Hospital), Nobuyuki Kurosawa (Tsuchiura Kyodo General
Hospital), Masuhiro Shimoda (Japanese Red Cross Musashino
Iijima K, Sako M, Oba MS et al. Japanese Study Group of Kidney Disease inChildren. Cyclosporine C2 monitoring for the treatment of frequently
Kidney International
N Yoshikawa et al.: RCT for initial prednisolone in childhood NS
Kenichiro Miura (The University of Tokyo Hospital), Atsushi
Shimizu (Sakai City Hospital), Katsuhisa Yamamoto (Minoh
Inatomi (Yaizu City Hospital), Yoshiyuki Otomo (Juntendo
City Hospital), Shinichi Sumimoto (Osaka Red Cross
University Nerima Hospital), Tomonosuke Someya (Juntendo
Hospital), Koichi Nakanishi (Wakayama Medical University
University Hospital), Shoichi Oyama (Saiseikai Kawaguchi
Hospital), Noriyuki Aoyagi (Wakayama Rosai Hospital), Seiji
General Hospital), Hiroshi Hataya and Kenji Ishikura (Tokyo
Iwahashi (Hidaka General Hospital), Masakazu Miyawaki
Metropolitan Children's Medical Center), Takeshi Matsuyama
(Fussa Hospital), Masahiro Banba (Yokosuka Kyosai Hospi-
(Izumiotsu Municipal Hospital), Masamitsu Nishino (Takat-
tal), Kiyoshi Araki (Saitama Social Insurance Hospital),
suki General Hospital), Daisuke Hata (Kitano Hospital),
Hitoshi Wakaki (Yokohama City Hospital), Cho Hideo
Mikio Goto (Kishiwada City Hospital), Ryojiro Tanaka
(Kawasaki Municipal Hospital), Tomonori Harada (Yokohama
(Hyogo Children's Hospital), Kandai Nozu and Hiroshi Kaito
City University Medical Center), Tomoko Nakamura (Oda-
(Kobe University Hospital), Sakiko Konohana (Ono Munici-
wara Municipal Hospital), Shoko Goto (Saiseikai Yokohama
pal Hospital), Ichiro Kamioka (Kakogawa City Hospital),
City Nanbu Hospital), Fumio Niimura (Tokai University
Masayuki Yamane (Saiseikai Hyogoken Hospital), Katsuji
Hospital), Naohiro Wada (Shizuoka Children's Hospital),
Kuwakado (Kurashiki Central Hospital), Shoji Kagami
Masami Shirai (Iwata City Hospital), Kozo Muto (Shimada
Municipal Hospital), Osamu Uemura (Aichi Children's Health
University Medical Center), Yoshihiko Murakami (Omuta
and Medical Center), Yoshimitsu Goto (Japanese Red Cross
City Hospital), Jiro Iwamoto (Iizuka Hospital), Yoshitsugu
Nagoya Daini Hospital), Naoya Fujita (Seirei Hamamatsu
Kaku (Fukuoka Children's Hospital & Medical Center for
General Hospital), Kazuhide Ohta (National Hospital Orga-
Infectious Diseases), Kentaro Kamesaki (Kokuritsukokura
nization Kanazawa Medical Center), Masaki Shimizu (Kana-
Hospital), Ken Hatae (Japanese Red Cross Fukuoka Hospital),
zawa University Hospital), Koichi Tsukahara (Fukui University
Hitoshi Nakazato (Kumamoto University Hospital), Yasushi
Hospital), Yukiko Mori (Fukui Red Cross Hospital), Hiroshi
Otsuka (Saga University Hospital), Tomohiro Ichimaru
Akutagawa (Hyogo Prefectural Tsukaguchi Hospital), Toshi-
(Saga-ken Medical Centre Koseikan), and Tadashi Sato
hiro Sawai (Shiga University of Medical Science Hospital),
(National Hospital Organization Ureshino Medical Center).
Kashiro Nishizawa (Omihachiman City Hospital), AkiraAshida (Osaka Medical College Hospital), Naohisa Kawamura(Osaka Rosai Hospital), Takuya Tanabe (Hirakata City
This work is licensed under a Creative Commons
Hospital), Koji Taira (Nara Prefectural Nara Hospital), Seiji
Attribution-NonCommercial-NoDerivs 3.0 Un-
Kinoshita (Higashi-Osaka City General Hospital), Shinya
ported License. To view a copy of this license, visit
Tanaka (Hyogo Prefectural Nishinomiya Hospital), Nobuhiko
Kidney International
Source: https://www.wakayama-med.ac.jp/intro/press/201407/h26-0729ns2.pdf
REVERSE PAYMENT PATENT SETTLEMENTS IN THE EUROPEAN UNION AND THE UNITED STATES Damien Geradin George Mason University School of Law Douglas Ginsburg George Mason University School of Law Graham Safty University of Chicago Law School George Mason University
Security Guards A guide for newcomers to British Columbia Security Guards A guide for newcomers to British Columbia Contents 1. Working as a Security Guard [NOC 6541] . 2 2. Skills, Education and Experience . 7 3. Finding Jobs . 9 4. Applying for a Job . 11 5. Getting Help from Industry Sources . 12 1. Working as a Security Guard [NOC 6541]