Amiodarone or lidocaine for cardiac arrest: a systematic review and meta-analysis

Contents lists available at
Amiodarone or lidocaine for cardiac arrest: A systematic review and
F. Sanfilippo , C. Corredor , C. Santonocito , G. Panarello , A. Arcadipane ,
G. Ristagno , T. Pellis
a Department of Anesthesia and Intensive Care, IRCCS-ISMETT (Istituto Mediterraneo per i Trapianti e Terapie ad alta specializzazione), Via Tricomi 5,
90127 Palermo, Italy
b Cardiovascular Anaesthesiology and Critical Care, Toronto General Hospital, 200 Elizabeth Street, Toronto, ON M5G 2C4, Canada
c IRCCS-Istituto di Ricerche Farmacologiche "Mario Negri", Milan, Italy
d Italian Resuscitation Council—Scientific Committee, Bologna, Italy
e Anesthesia Institute, Cleveland Clinic Abu Dhabi, Abu Dhabi, UAE
Background: Guidelines for treatment of out-of-hospital cardiac arrest (OOH-CA) with shockable rhythm
Received 25 May 2016
recommend amiodarone, while lidocaine may be used if amiodarone is not available. Recent underpow-
Received in revised form 14 July 2016
ered evidence suggests that amiodarone, lidocaine or placebo are equivalent with respect to survival at
Accepted 18 July 2016
hospital discharge, but amiodarone and lidocaine showed higher hospital admission rates. We undertook
a systematic review and meta-analysis to assess efficacy of amiodarone vs lidocaine vs placebo.
Methods: We included studies published in PubMed and EMBASE databases from inception until May
Out-of-hospital cardiac arrest
15th, 2016. The primary outcomes were survival at hospital admission and discharge in OOH-CA patients
enrolled in randomized clinical trials (RCT) according to resuscitation with amiodarone vs lidocaine
Hospital admission
Hospital discharge
vs placebo. If feasible, secondary analysis was performed including in the analysis also patients with
Return of spontaneous circulation
in-hospital CA and data from non-RCT.
Results: A total of seven findings were included in the metanalysis (three RCTs, 4 non-RCTs). Amio-
darone was as beneficial as lidocaine for survival at hospital admission (primary analysis odds ratio—OR
0.86–1.23, p = 0.40) and discharge (primary analysis OR 0.87–1.30, p = 0.56; secondary analysis OR
0.86–1.27, p = 0.67). As compared with placebo, survival at hospital admission was higher both for
amiodarone (primary analysis OR 1.12–1.54, p < 0.0001; secondary analysis OR 1.07–1.45, p < 0.005)
and lidocaine (secondary analysis only OR 1.14–1.58, p = 0.0005). With regards to hospital discharge
there were no differences between placebo and amiodarone (primary outcome OR 0.98–1.44, p = 0.08;
secondary outcome OR 0.92–1.33, p = 0.28) or lidocaine (secondary outcome only OR 0.97–1.45, p = 0.10).
Conclusions: Amiodarone and lidocaine equally improve survival at hospital admission as compared with
placebo. However, neither amiodarone nor lidocaine improve long-term outcome.
2016 Elsevier Ireland Ltd. All rights reserved.
at hospital admission is approximately at hos-
pital discharge is much lower (8–24%).favorable
Sudden cardiac arrest (CA) is an emergency with high incidence
neurological outcome is reported only in less than half of patients
ranging between 320,000 and 700,000 events per year in the United
admitted to ICU after return of spontaneous circulation
States and out-of-hospital (OOH) CA, survival
The recent guidelines for the treatment of OOH-CA with a shock-
able rhythm (ventricular fibrillation – VF – or pulseless ventricular
tachycardia – VT –) suggest only amiodarone as antiarrhythmic
drug after three defibrillation attempts, while lidocaine may be
A Spanish translated version of the abstract of this article appears as Appendix
used as alternative, if amiodarone is not available.
in the final online version at .
∗ Corresponding author.
in a recent randomized controlled trial (RCT) amiodarone, lido-
E-mail addresses: (F. Sanfilippo),
caine or placebo had similar results, although the RCT was possibly
underpowered. Interestingly, amiodarone and lidocaine showed a
(C. Santonocito), (G. Panarello),
significantly higher number of patients admitted alive to the hos-
(A. Arcadipane), (G. Ristagno),
pital, and a higher survival at hospital discharge in the subgroup of
(T. Pellis).
0300-9572/ 2016 Elsevier Ireland Ltd. All rights reserved.
F. Sanfilippo et al. / Resuscitation 107 (2016) 31–37
"PICOS" approach for selecting clinical studies in the systematic search and meta-analysis. CA: cardiac arrest; VF: ventricular fibrillation; VT: ventricular tachycardia (pulseless).
Patients in CA with a shockable rhythm (VF/VT), including both in- and out-of-hospital setting
Administration of amiodarone
Placebo, lidocaine (primary analysis); no drug administered (secondary analysis)
Survival at hospital admission; survival at hospital discharge; favorable neurological outcome (modified Rankin scale score ≤3 or
return to independent living activities)
RCT (primary analysis); prospective and retrospective studies (secondary analysis)
patients with bystander-witnessed CA. Before this RCT, a recent
a modified Rankin scale score ≤3 or return to independent liv-
meta-analysis analyzed the efficacy of anti-arrhythmic drugs in
ing activities) was assessed. A secondary analysis was performed
the treatment of CA,it included drugs not currently recom-
including also results from non-RCTs and studies including patients
mended and suffered from large biases in the studies included. For
suffering from in-hospital CA.
instance, many of these studies were retrospective chart reviews,
with unbalanced baseline characteristics,different timing of
Quality assessment
drug administration and severely under-dosed treatments.
To overcome such limitations and in view of the recently pub-
Methodological quality of included RCTs was performed using
lished large RCT, we conducted a meta-analysis aiming at assessing
the Cochrane Collaboration tool which incorporated the following
the efficacy of amiodarone as compared with lidocaine or placebo.
domains: selection, performance, detection, attrition, performance
and other potential sources of of bias assessment for
observational studies was performed using the Newcastle–Ottawa
scale (NOS) which gives up to nine points if all criteria of qual-
Search strategy and criteria
ity assessment are fulfilled. The scale has three main domains and
according to their score studies are classified at high risk (1–3
We undertook a systematic web-based advanced literature
points), intermediate risk (4–5 points) and low risk of bias (6–9
search through the NHS Library Evidence tool on the effects of
amiodarone in patients with CA. We followed the approach sug-
gested by the PRISMA statement for reporting systematic reviews
Statistical analysis
and a PRISMA checklist is provided separately
(Supplemental digital content 1).
The Mantel–Haenszel method was used to analyze dichotomous
An initial computerized search of MEDLINE (PubMed) was con-
outcomes of survival at hospital admission and at hospital dis-
ducted from inception until April 10th, 2016 to identify the relevant
charge and survival with good neurological outcome. Results are
articles. With these findings, we wrote a draft of the prospec-
reported as odd ratios (OR) with 95% confidence intervals (CI) and
tive study protocol. A final search was re-performed at the end
two tailed p values. p values were considered significant if <0.05.
of the analysis (May 15th, 2016) to identify further findings. Our
The presence of statistical heterogeneity was assessed using the
core search was structured by combining a group of findings
X2 (Cochran Q) test. Heterogeneity was likely if Q > df (degrees
containing the term "cardiac arrest" or "hear arrest" with a sec-
of freedom) suggested and confirmed if p ≤ 0.10. Quantification of
ond group including the word "amiodarone" and/or "lidocaine".
heterogeneity was performed and values of I2 ranging 0–24.9%,
Two further searches were performed manually combining the
25–49.9%, 50–74.9% and >75% were considered as none, low, mod-
words "amiodarone" and "cardiac arrest" or "lidocaine" and "car-
erate and high heterogeneity, respectively. If heterogeneity was
diac arrest". Inclusion criteria were pre-specified according to the
quantified as low or above, a random-model was also used for
We a priori decided to consider a secondary analysis includ-
ing non-randomized prospective and retrospective clinical studies.
We excluded experimental animal studies, book chapters, reviews,
editorials and letters to editor. Case series were not included in
the secondary analysis unless reporting at least 10 patients per
Our systematic search identified 528 findings via NHS Library
group. Study selection for determining the eligibility for inclusion
Evidence search. No other findings were retrieved manually. As
in the systematic review and data extraction were performed inde-
shown in the PRISMA flow diagram (Supplemental digital content
pendently by four reviewers (FS, CC, CS, AA). Discordances were
2), after the evaluation of all findings, only seven studies were
resolved by involving the other three authors and/or by consensus.
judged of interest for our analyses: three RCTs, one prospective
Language restrictions were applied: we read the full manuscript
observational study and three retrospective chart review studies.
only for articles published in English, French, Spanish, German or
Of the RCTs, the most recent was a "three-arm" trial enrolling
Italian. For prospective and retrospective studies published in other
3026 patients (per-protocol population) divided in amiodarone
languages, we read the abstract and, if necessary, contacted the
(n = 974), lidocaine (n = 993) or placebo (n = trial was
authors for further information. A manual search was conducted
by far the largest trial since the other two comparing amiodarone
independently by three authors (FS, CS, AA), exploring also the list
with with only a total of 347 and
of references of the findings of the systematic search.
304 patients, respectively.
The only prospective observational study that compared lido-
Groups and endpoints
caine vs no lidocaine in OOH-CA patients and included 116 patients
and was over 25 years oldthe three retrospective studies
We primarily compared the efficacy of amiodarone vs lidocaine
included 290 (lidocaine vs no lidocaine),(amiodarone vs
vs placebo with regards of survival at hospital admission and hospi-
no 118 patients (amiodarone vs lidocaine).
tal discharge in patients with OOH-CA enrolled in RCTs. If available,
Only the latter study was performed in patients suffering from
the incidence of favorable neurological outcome (as defined by
in-hospital CA.
F. Sanfilippo et al. / Resuscitation 107 (2016) 31–37
Summary of the results of meta-analyses comparing amiodarone vs lidocaine vs placebo. The outcome analysed, the number of studies included in the analysis, the odds
ratio (OR), the p value, the heterogeneity (I2) and the figure of the forest plot are reported in separate columns. In bold are highlighted the p values reaching a statistically
Amiodarone vs placebo
Survival at hospital discharge
1.19 [0.98–1.44]
Survival at hospital admission
1.32 [1.12–1.54]
Survival & good neurological outcome
1.16 [0.93–1.44]
Survival at hospital
1.11 [0.92–1.33]
Survival at hospital admission
1.25 [1.07–1.45]
Lidocaine vs placebo
Survival at hospital
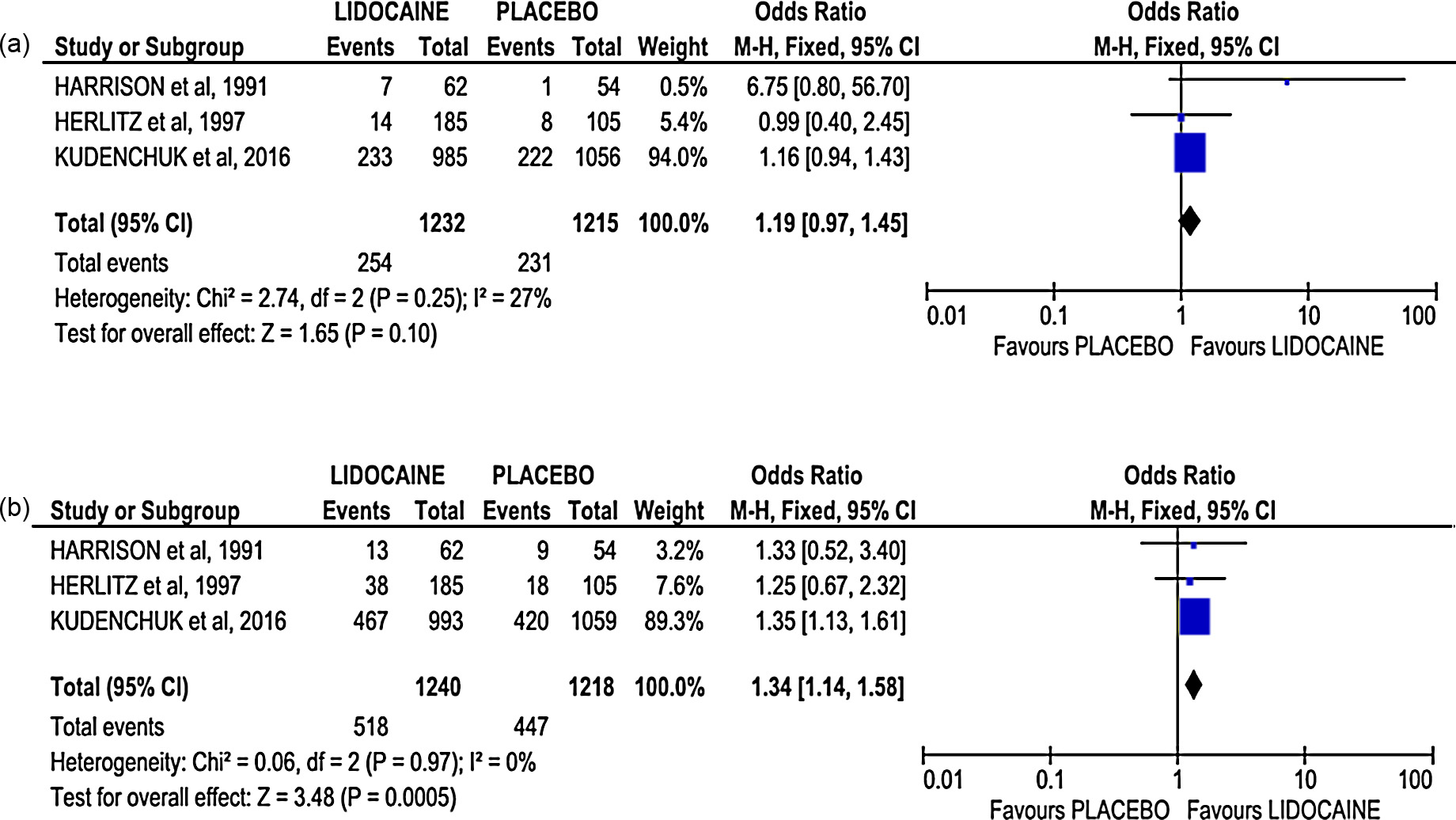
1.19 [0.97–1.45]
Survival at hospital admission
1.34 [1.14–1.58]
Amiodarone vs lidocaine
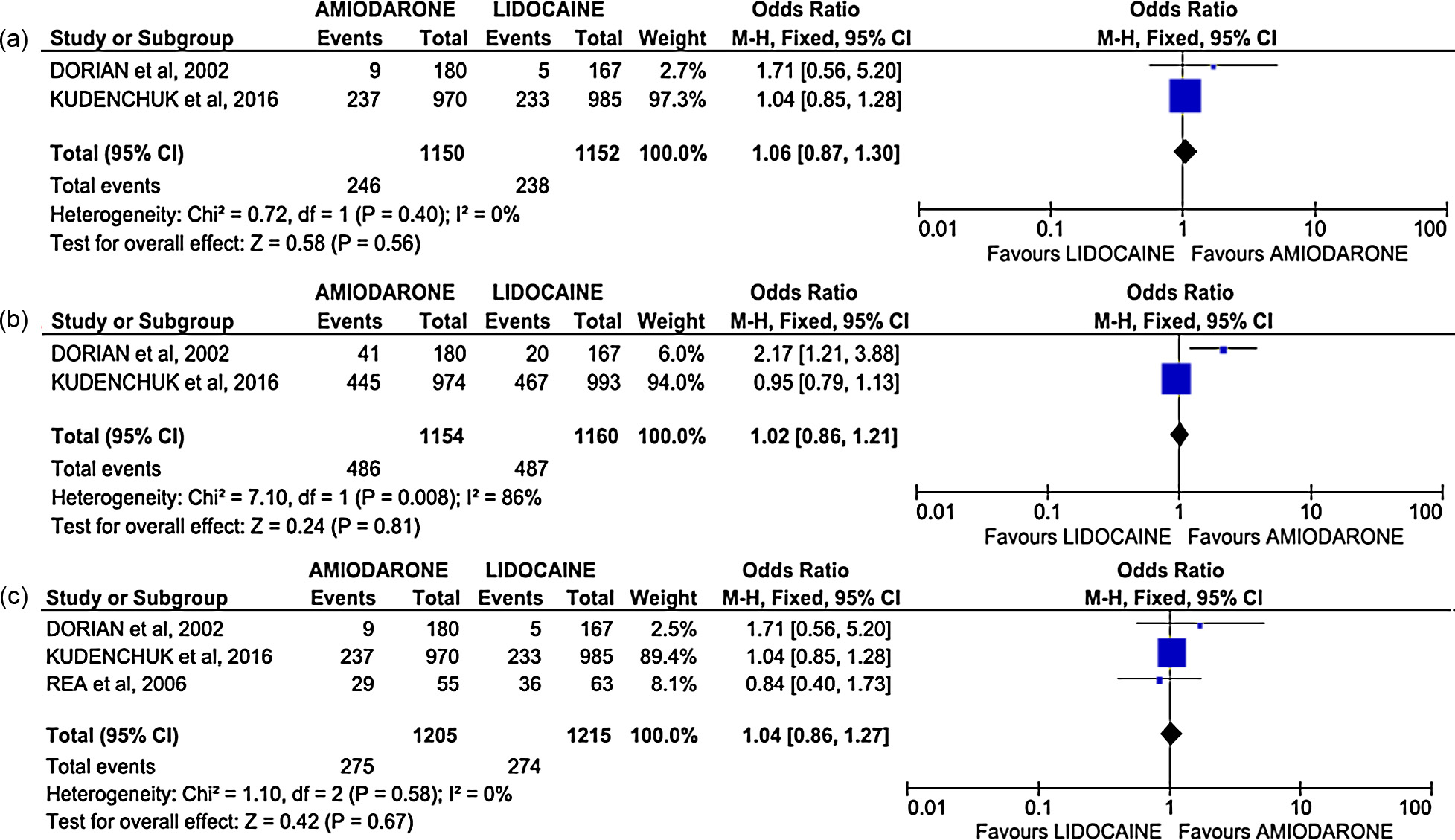
Survival at hospital discharge
1.06 [0.87–1.30]
Survival at hospital admission
1.02 [0.86–1.21]
Survival at hospital
1.04 [0.86–1.27]
a Analysis conducted including also non-randomized studies.
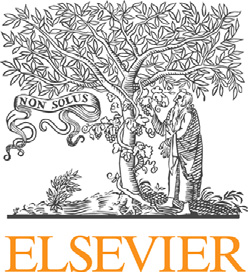
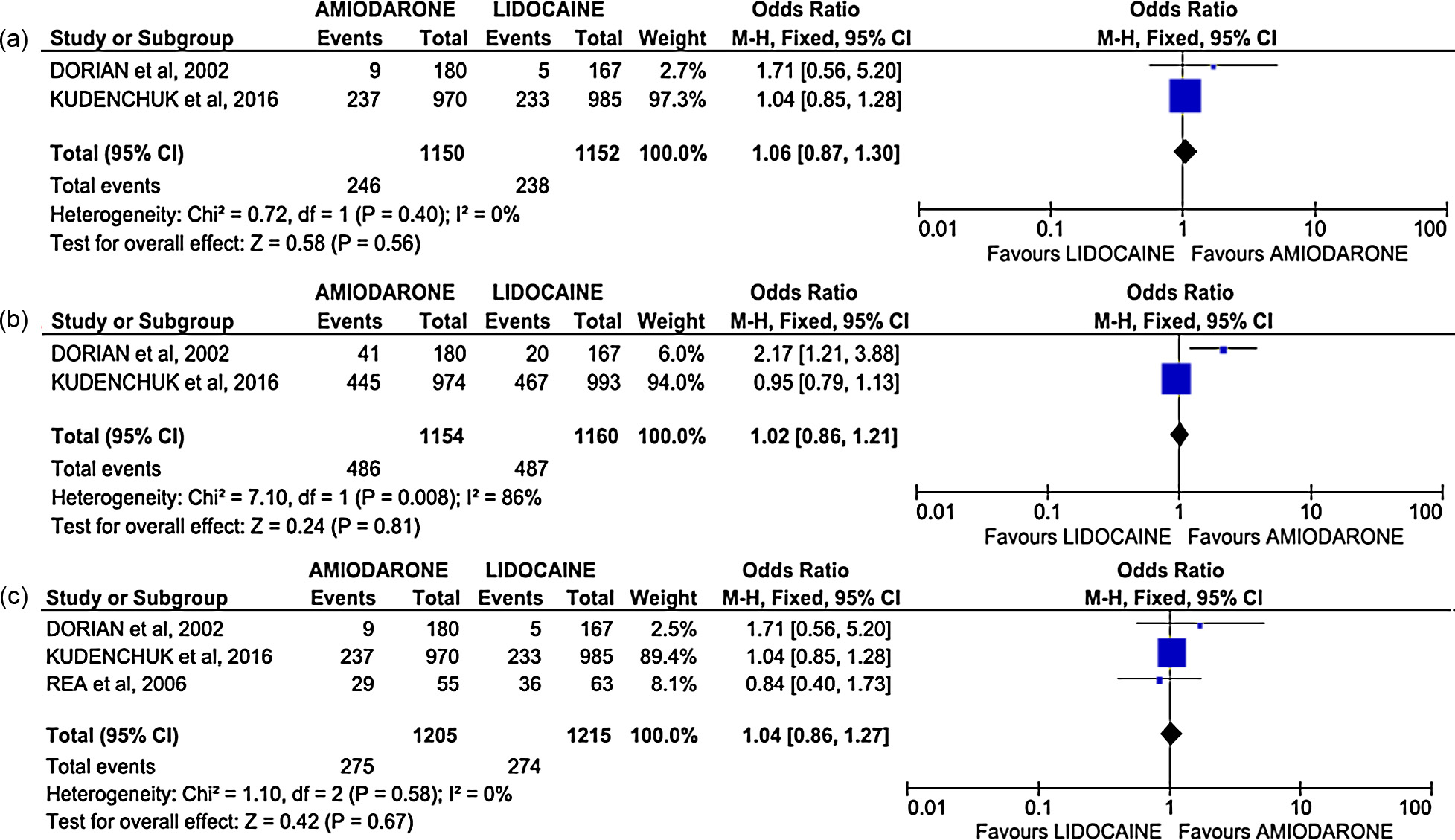
Fig. 1. Forest plots comparing amiodarone vs placebo. (1a) Survival at hospital discharge; (1b) survival at hospital admission; (1c) survival at with good neurological outcome.
The results of the three comparison between amiodarone, lido-
difference between amiodarone and placebo also with respect to
caine and placebo are reported separately as subparagraphs and
survival at hospital admission (OR 1.13 [0.77–166], p = 0.53).
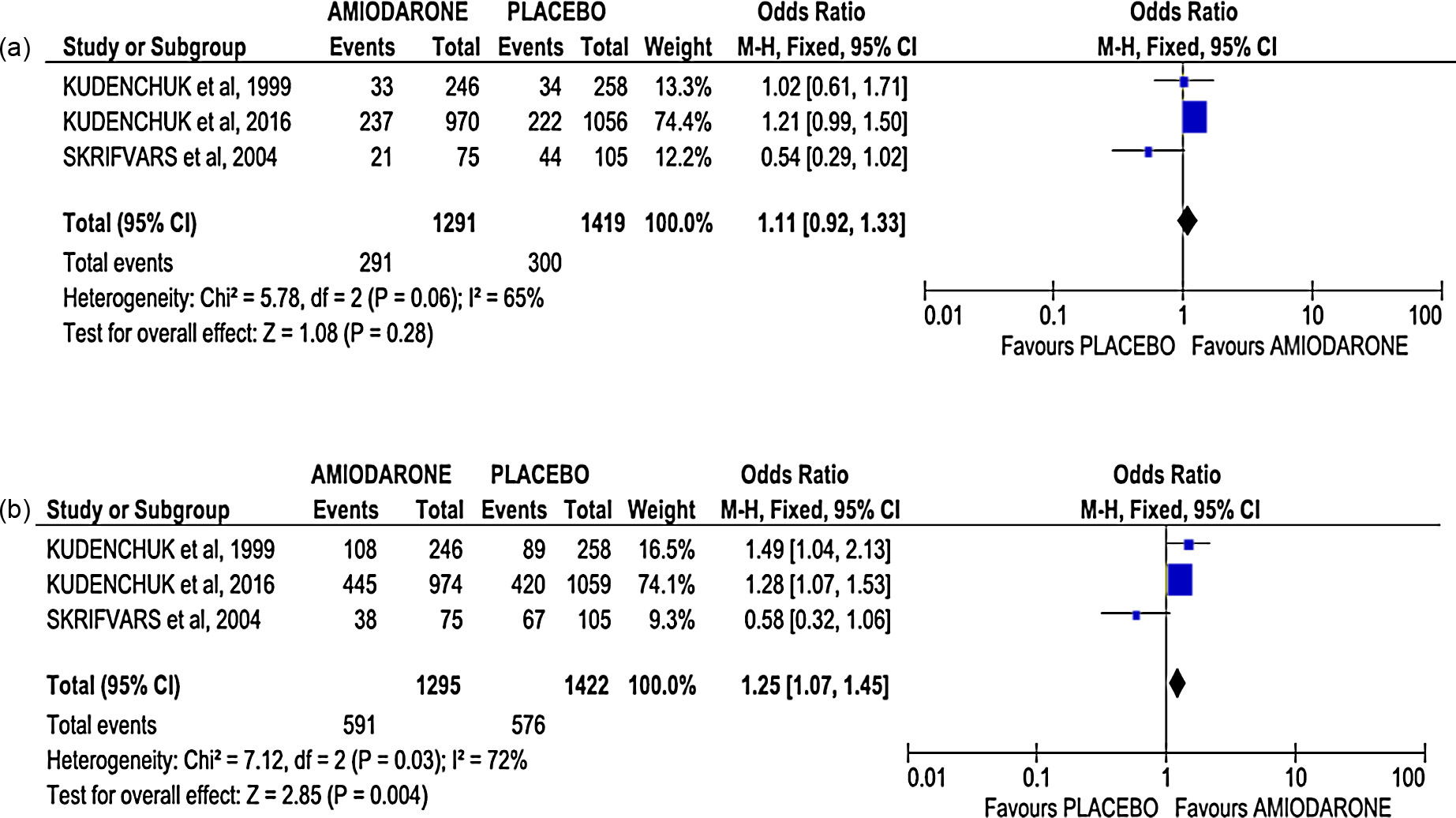
Lidocaine vs placebo
Amiodarone vs placebo
Only one RCT compared lidocaine vs placebo in the treatment
Two RCTs compared amiodarone vs placebo in the treatment of
of CA one retrospective
CA victimsup to 2537 patients. Amiodarone showed a
evaluated the administration of lidocaine vs none in patients with
trend toward higher survival at hospital discharge (p = 0.08,
OOH-CA. In the analyses of these three studies with data up to
and a significantly higher survival at hospital admission (p = 0.0006,
2458 patients, lidocaine showed a trend toward higher survival
There was no difference in discharge with favorable neuro-
at hospital discharge (p = 0.10, This result showed mild
logical outcome between amiodarone and placebo (p = 0.18,
heterogeneity (I2 = 27%) and the analysis with the random effect
There was no heterogeneity in these three results.
made the trend non-significant (p = 0.41, result not shown). Lido-
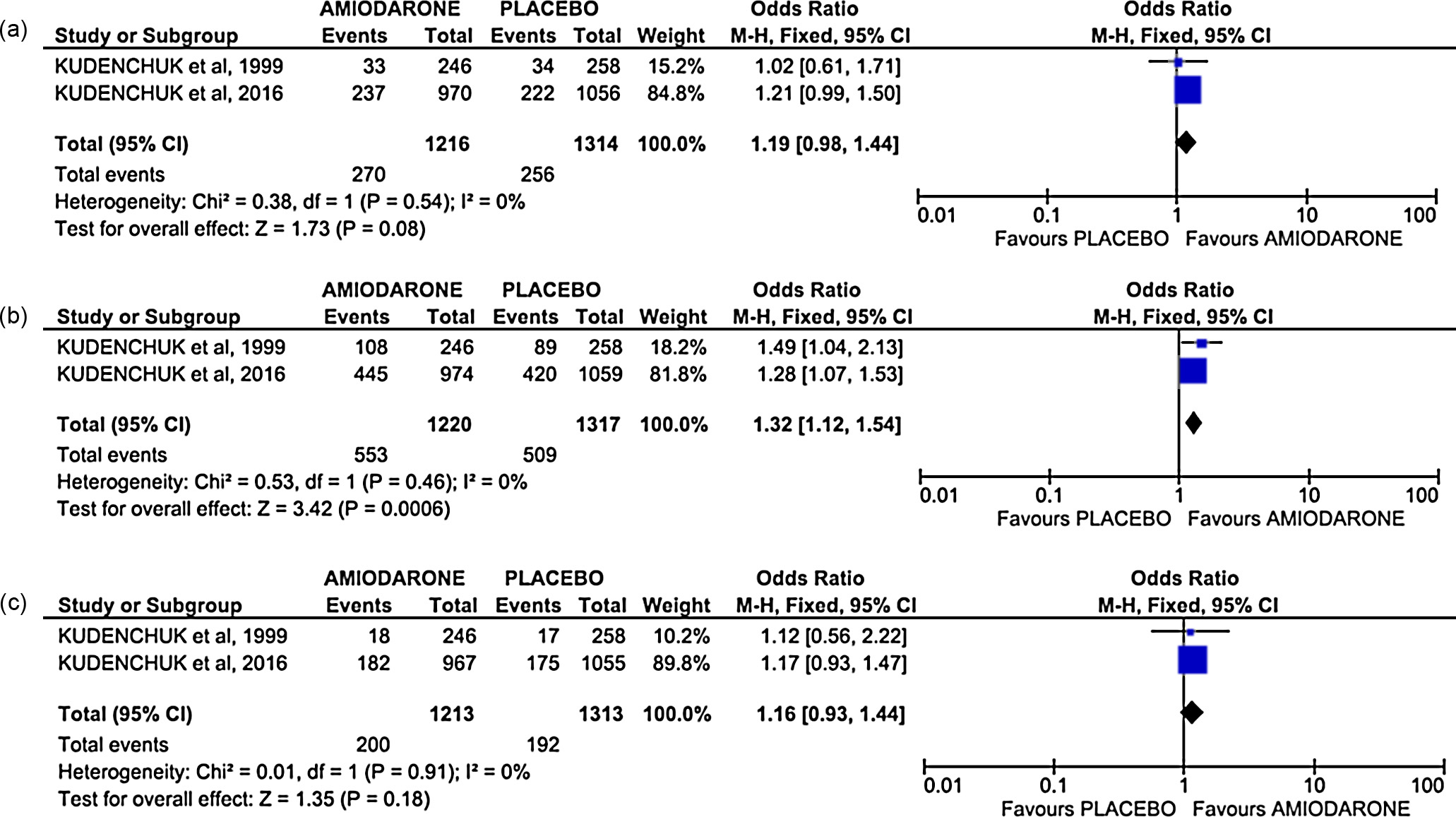
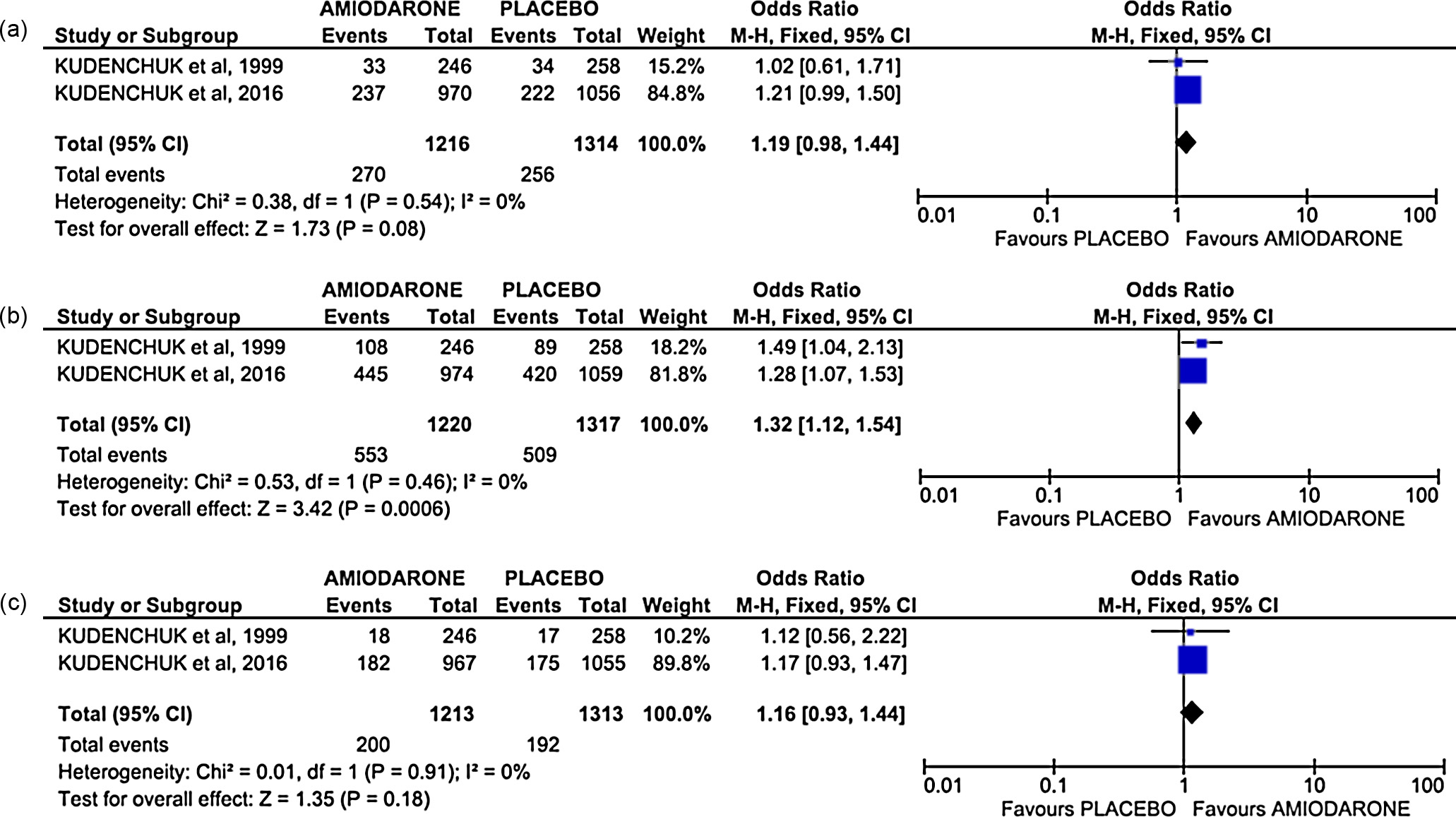
In the secondary analysis conducted adding one retrospective
caine showed a significantly higher survival at hospital admission
studyfurther 180 patients, amiodarone was not associ-
(p = 0.0005, There was no heterogeneity in this result.
ated with survival at hospital discharge (p = 0.28; but
remained significantly associated with survival at hospital admis-
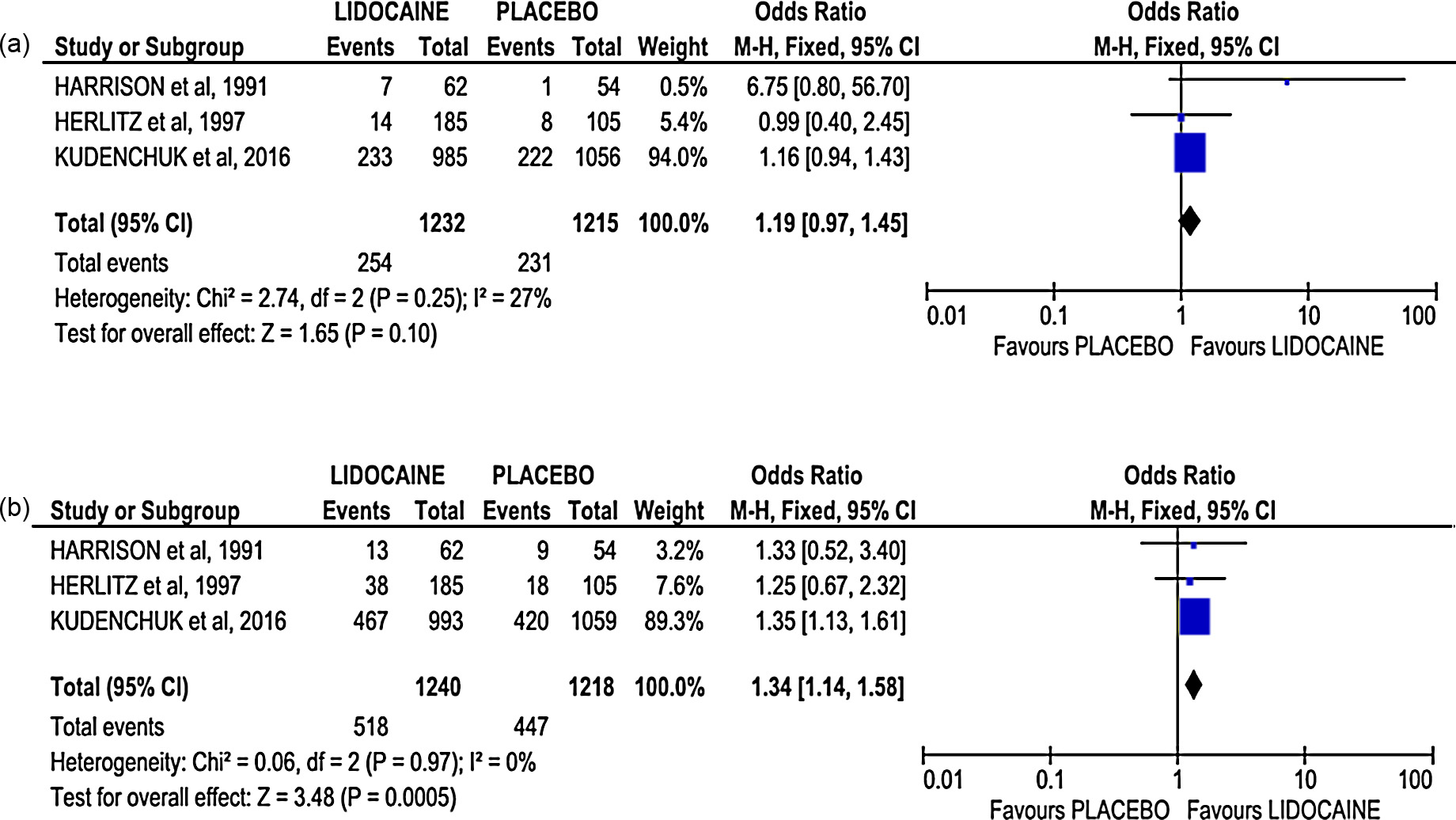
Amiodarone vs lidocaine
sion (p = 0.004; In both analyses, there was a moderate
degree of heterogeneity (I2 = 65% and 72% respectively). However,
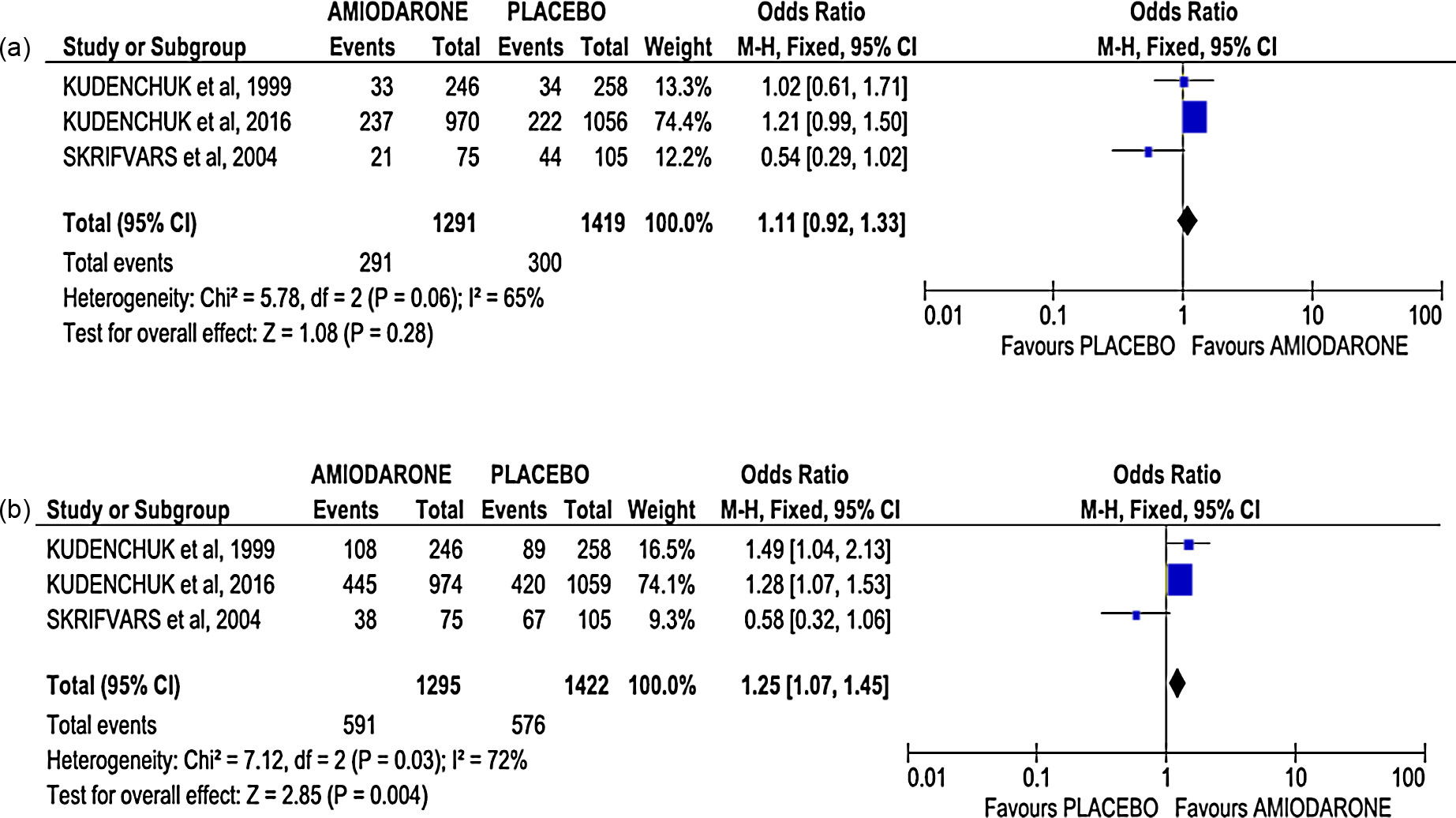
Two RCT compared amiodarone vs placebo in the treatment of
using a random-effect model, the secondary analysis showed no
CA up to 2302 patients. There were no dif-
F. Sanfilippo et al. / Resuscitation 107 (2016) 31–37
Fig. 2. Forest plots comparing amiodarone vs placebo including in the analysis also one non-randomized controlled study. (2a) Survival at hospital discharge; (2b) survival
at hospital admission.
Fig. 3. Forest plots comparing lidocaine vs placebo including in the analysis also two non-randomized controlled studies. (3a) Survival at hospital discharge; (3b) survival at
hospital admission.
ferences in survival at hospital discharge (p = 0.56, and at
Risk of bias assessment
hospital admission (p = 0.81, Only one study reported neu-
rological therefore such analysis was not feasible.
The assessment of risk of bias for RCTs, showed that only the
There was no heterogeneity in the first result, while a high hetero-
recent RCT was at low risk of bias,the other studies
geneity was seen in the survival at hospital admission (I2 = 86%)
one or more domain with unclear or high risk of bias (Supplemental
but the analysis with random-effect did not change the results
digital content 3).
(p = 0.45). Survival at hospital discharge was also evaluated by one
The assessment of risk of bias for non-RCTs performed with
retrospective study in 118 patients with in-hospital inclu-
the NOS method showed that all the studies had low-risk, scor-
sion of this study in the secondary analysis did not change the result
ing 6/9 or above. In particular, scores were higher in the two most
recent ones slightly lower for Herlitz et al.
F. Sanfilippo et al. / Resuscitation 107 (2016) 31–37
Fig. 4. Forest plots comparing amiodarone vs lidocaine. (4a) Survival at hospital discharge; (4b) survival at hospital admission; (4c) survival at hospital discharge including
in the analysis also one non-randomized controlled study.
the lowest score was found for the prospective study (6/9).
data (180 patients) for the secondary analysis were obtained from
these studies had no independent blind assessment/record linkage
(Supplemental digital content 4).
With only one high-quality RCT comparing the effects of lido-
caine vs placebo (2041 could not undertake a
metanalysis for the primary outcomes; however two further stud-
ies (one one enrolling a total of
406 patients allowed a secondary analysis. Similarly to amiodarone,
The primary endpoint of our meta-analysis was to evaluate
but with lower degree of evidence, administration of lidocaine
the effectiveness of antiarrhythmics when administered to adult
compared to no administration significantly improved survival to
non-traumatic CA patients with persistent or recurrent shock-
hospital admission, but there were no differences at hospital dis-
able rhythms. We found three RCTs comprising 3877 patients,
almost 1400 patients receiving amiodarone, over 1150 in the lido-
Finally, when amiodarone was compared to lidocaine, high-
caine group and more than 1300 randomized to
quality evidence from 1995 enrolled in a recent RCT
One prospective observational studythree retrospective
with low-quality evidence from 347 patients included in an ear-
studiesincluded in the secondary analysis providing
lier RCTno difference in survival to hospital admission
data on approximately 700 patients.
and discharge between the two drugs. The addition of data retro-
All but one conducted in the pre-hospital set-
spectively acquired from 118 patients who suffered an in-hospital
ting in the US and in Europe. The CPR treatments during ALS were
CAnot modify the results.
according to current AHA or ERC guidelines at the time of the enroll-
Although amiodarone and lidocaine are considered the standard
ment, ranging over a period greater than 20 years (1989–2016).
of care and are included in current guidelines to promote successful
The low number of published RCTs and the fact that all of them
defibrillation of shock-refractory VF or pulseless VT, and to prevent
are underpowered for the critical outcome of survival to hospi-
anti-arrhythmic drug given during CA has been
tal discharge prompted this meta-analysis. Indeed, even the most
shown to increase survival to hospital discharge. Until the publi-
recent RCT had a smaller-than-predicted treatment effect, since
cation of the recent was limited evidence in favor of
sample size was calculated on a predicted 6.3% absolute difference
the use anti-arrhythmic drugs for the management of arrhythmias
between amiodarone and placebo, which was almost twice than
in CA and, more specifically, it was limited to survival to hospital
the observed one.
admission.response to such need for sufficiently powered
One of the main finding of this meta-analysis is that administra-
RCTs, a large RCT, in which patients have been randomized to
tion of amiodarone during ALS as compared with placebo did not
amiodarone, lidocaine or saline placebo, was conducted. This study
improve survival at discharge nor survival with favorable neurolog-
confirmed in over 3000 patients significant benefits from the use of
ical outcome. However, administration of amiodarone compared
amiodarone or lidocaine with respect to short-term outcome but
to placebo showed significantly higher survival at hospital admis-
not on long-term survival or neurological recovery.
sion in both the RCTs. This finding stems from pooling data from
According to current AHA end ERC guidelines amiodarone or
one high-quality evidence recent RCT (over 2400 a
lidocaine may be considered (class IIb recommendation): in par-
smaller low-quality evidence RCT (just over 500 patients) from the
ticular, a bolus of 300 mg of amiodarone may be given after three
same research group conducted over 15 years additional
defibrillation attempts, while a bolus of 1–1.5 mg/kg of lidocaine
F. Sanfilippo et al. / Resuscitation 107 (2016) 31–37
may be used as alternative, if amiodarone is not
population. Importantly, post-ROSC treatment of patients was not
Amiodarone is a membrane-stabilizing anti-arrhythmic drug and
standardized, nor the quality was evaluated by the studies included
improves the response to defibrillation in VF or hemodynamically
in this metanalysis, and this may have played a role on survival.
unstable VT.onset of its antifibrillatory action is slower
Although the results of our metanalysis are similar to those of the
than lidocaine, but its effect is longer-lasting.of brady-
most recent meta-analysis has some advantages. One is
cardia and hypotension post-ROSC have been reported in patients
providing the reader with a systematic and up-to-date evidence
receiving amiodarone during resuscitation.has
on the effects of amiodarone and lidocaine on outcomes of CA
been one of the antiarrhythmic drugs for shock-resistant or recur-
patients. Another advantage is the reinforcement of Kudenchuck
rent VF in the lidocaine has detrimental
et al. not only by the similar results but also
effects on counter-shock efficacy due to an increase in lidocaine's
by the absence of heterogeneity in the primary analyses (I2 = 0%).
affinity for sodium-channel receptors in acidotic
Moreover, our results suggests a reconsideration of the role of lido-
and has been associated with an increased rate of post-shock
caine that still appears only as a substitute of amiodarone in case
asystole.evidence on the use of lidocaine vs amiodarone
was uncertain; while some authors showed higher rates of survival
We acknowledge several limitations in our meta-analysis. First
to hospital admission in patients with shock-resistant VF when
of all, the studies included are largely different in several aspects.
amiodarone was used as compared to reports
These studies, in fact, reported pooled data from patients who
were contradictory.recent RCT from Kudenchuck et al.
presented differences in the setting of collapse, rate of wit-
demonstrated substantial equivalence in short-term outcomes
nessed events and bystander-initiated CPR, resuscitative protocols
with either amiodarone or lidocaine, with a potential disadvantage
employed, that varied based on concurrent guidelines, with differ-
of more numerous episodes of hypotension and bradycardia in the
ent shock protocols and time to drug administration. In this regards,
amiodarone group. These adverse events were observed despite the
the time lag between the first and the last RCT is over 15 years, and
use of a new amiodarone aqueous formulation in which polysor-
between all the studies included is over 25 years. Finally, different
bate 80 has been replaced by captisol and therefore supposedly
amiodarone formulations (with polysorbate solvent – potentially
devoid of hypotensive effects. Thus, although current guidelines
accounting for or aqueous solution), and different
advocate amiodarone as the first choice drug in refractory and
dosages of amiodarone or lidocaine were employed.
recurrent VF/pulseless VT, recent evidence may lead to potential
In conclusion, the above limitation withstanding, both amio-
discussion and revision on the consensus on science.sim-
darone and lidocaine seem equally beneficial as compared with
ilarly to vasopressors during CPR, there is evidence of benefit only
placebo with respect to survival to hospital admission. However,
on short-term outcome but not in the long-term survival, mean-
neither amiodarone nor lidocaine improves long-term outcome, in
ing that a greater number of patients potentially resuscitated with
term of survival to hospital discharge or neurological recovery.
aid of an anti-arrhythmic drug, subsequently die during hospital
stay. Several reasons may provide potential explanation for this
Conflict of interest statement
Among these, the timing of administration of the drug may play
a pivotal role. The optimal time at which these drugs should be
given when using a single-shock strategy remains unknown but it
is likely that their efficacy is gradually lost with delayed adminis-
tration, in particular during the so-called "metabolic phase", when
the ischemic injury results in release of metabolic factors causing
additional beneficial effects from an early interven-
tion is well recognized in the instance of a defibrillation attempt,
Appendix A. Supplementary data
as well as vasopressors administration during cardiac
For instance, epinephrine has been shown effective in improving
Supplementary data associated with this article can be found,
survival to hospital discharge and survival with good neurological
in the online version, at
outcome when given within 10 min from collapse, while evidence
of possible harm has been reported when it was administered
later.the clinical studies, amiodarone or lidocaine were usually
given if VF/VT persisted after at least three shocks,
the exception of the most recent RCTwhich at least one shock
was delivered prior to drug injection. In the older studies, the time
from collapse to drug administration ranged from 15 to 24 min. It
is noteworthy that in the recent RCT the first administration of the
study drug was performed after a median of three shocks, resulting
in mean administration time of 19
Thus, the treatment was administered fairly late in all the
studies, when significant end-organ damage had probably already
resulted from prolonged hypoperfusion, especially in the cen-
tral nervous system. For these reasons, the potential benefit of
treatment could have been underestimated. This hypothesis is
strengthened by the observation in the recent RCTpatients
with witnessed CA receiving earlier initiation of resuscitation and
a shorter interval to antiarrhythmic drug administration (12 min)
had significantly higher survival at hospital discharge (by about
5%). However, only this recent RCT provided data on witnessed CA
and therefore we could not perform a sub-analysis of this patient's
F. Sanfilippo et al. / Resuscitation 107 (2016) 31–37
31. Guidelines for cardiopulmonary resuscitation and emergency cardiac care.
Emergency Cardiac Care Committee and Subcommittees, American Heart Asso-
ciation. Part I. Introduction. JAMA 1992;268:2171–83.
32. Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovas-
cular Care. Part 6: advanced cardiovascular life support: section 5: pharmacology
I: agents for arrhythmias. The American Heart Association in collabora-
tion with the International Liaison Committee on Resuscitation. Circulation
18. Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P. The
Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised
studies in meta-analyses
Source: http://www.cercp.org/images/stories/recursos/articulos_mes/octubre_2016_Articulo.pdf
Middle-East Journal of Scientific Research 20 (8): 893-899, 2014 © IDOSI Publications, 2014 Studying the Factors Affecting Osteoporosis in Women with the Logistic Regression Analysis 1Bülent K l ç, Y 2 avuz Ta k ran, 3A. Serdar Yücel and M urat Korkmaz 1Orthopedist, Tekirda , Turkey 2Kocaeli University School of Physical Education and Sports, Kocaeli, Turkey
3D Cell Culture: A Review of Current Techniques Brad Larson, Senior Applications Scientist, Applications Department, BioTek Instruments, Inc., Winooski, VT Over the last decade, a central focus of drug discovery efforts has been the incorporation of in vitro testing models that better mimic in vivo conditions found within the target patient. An initial step saw a move away from biochemical assays using purified drug target, in favor of a cell-based approach which utilized over-expression of drug target in common host cell lines, such as CHO and HEK-293. The quest for greater physiological relevance proceeded to the use of primary cells, preferably human if supply was adequate, and the reliance on endogenous expression of drug target should detection technology be sensitive enough. A large percentage of these cell types, being naturally adherent, allowed simple culturing workflows that seeded cells in a coated microplate well, incubating the microplate to encourage the cells to attach in a two dimensional (2D) monolayer before performing the prescribed assay. While providing initial improvements over biochemical and immortalized cell lines, an abundance of evidence now supports the reality that culturing cells in this 2D manner is often problematic and is a relatively poor model for in vivo conditions and behaviors. Using a 2D model, attrition rates of drug candidates for cancer were approximately 95%1, stemming from in vitro drug efficacy values that did not translate to the clinic, as well as unforeseen toxicity issues. In 2011 alone, out of approximately 900 anti-cancer therapies in clinical trials or under Federal Drug Administration review2, only twelve achieved approval3; resulting in the loss of hundreds of millions of dollars that were spent on pre-clinical and clinical trials. The reason for these shortfalls can be traced to using conventional 2D conditions, where extracellular matrix (ECM) components, cell-to-cell and cell-to-matrix interactions, important for differentiation, proliferation and cellular functions in vivo, are lost4.