Sleep_dr gold
The "old school" definition of
fibromyalgia (FM) used to be a sleep
disorder that produced muscle pain. It
was a textbook phenomenon identified
by Harvey Moldofsky, M.D., of
the nose, travels down the wind-pipe
the size of the airway opening (includ-
Toronto, Canada, of awake-like brain
(trachea) and into the lungs where
ing swelling from infections or
waves (alpha) interspersed throughout
oxygen is exchanged for carbon
allergens), could potentially lead to
sleep and could be documented by a
dioxide (the by-product of respira-
sleep study using an electroencephalo-
tion), which is then exhaled. The
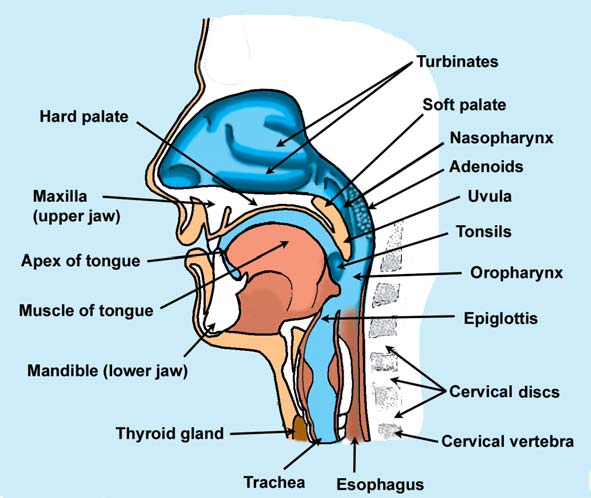
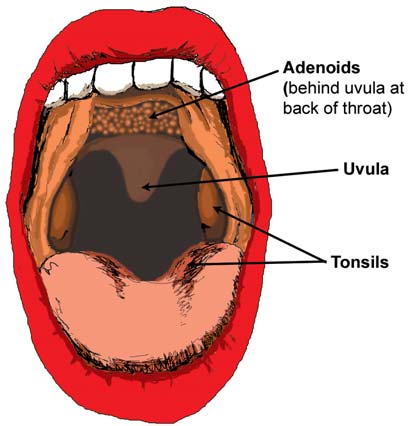
As you examine Diagrams A and
gram (EEG). This alpha-EEG was
process is simple: the lungs expand to
B, keep in mind the list below of
noticed in other medical conditions,
draw in air and they contract to expel
structural defects that may interfere
so it carried little weight as a diagnos-
it. Along the way, however, a number
with breathing, especially during sleep
tic tool. In fact, for the past ten years
of structural and physiological defects
when the head is in the reclined
the sleep disorder concept of FM, as
may place a damper on this simple,
position (see Diagram C).
well as chronic fatigue syndrome
rhythmic process. Also, some people
9 Small nostrils and/or wide (devi-
(CFS), has been shelved. Today, the
are less fortunate than others, possess-
focus is primarily on the symptom of
ing several of these glitches and
9 Excessive cartilage in the nose
causing a greater resistance to airflow.
9 Large, swollen turbinates (often
Sophisticated tools are being used
As a result, the breathing "system" for
due to allergens or infections)
to study FM pain and its many symp-
each person is uniquely shaped by
9 Upward arched hard palate
toms that are somehow linked to the
genetics (e.g., structure) and the
9 Long, dangling soft palate (uvula)
plethora of scientific findings associ-
environment (e.g., allergens).
9 Small nasopharnyx or oropharnyx
ated with the syndrome. Research is
The best way to point out the
9 Large tongue in comparison to
further complicated by the fact that
common problems that may interfere
chin size (e.g., recessed chin)
individuals with FM/CFS are a
with breathing is through the use of
9 Narrow upper maxillary bone
diverse group of patients.
illustrations. In Diagram A, a cross-
(smaller than normal distance
But, what if FM/CFS was not so
sectional drawing of the nose, mouth
between back molars)
complicated? What if the unifying
and throat highlights the path that air
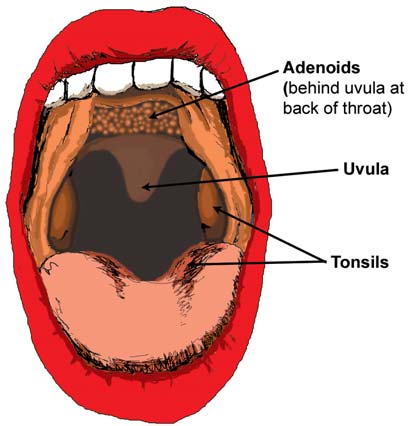
9 Tonsils and/or adenoids present
element among patients relates to
must follow from the nose to the
(especially if swollen due to
structural abnormalities in the air-
ways—from the tip of the nose to the
bronchial tubes entering the lungs?
Diagram A
Sounds too good to be true, doesn't it?
More studies are needed, but in the
meantime, Fibromyalgia Network will
let you decide whether researchers
have stumbled upon the solution to the
FM equation as we bring you back to
the classroom to learn the basics of
sleep, and the most crucial element of
life itself: the ability to breathe.
‘Refresher Course' in
structuresmay impede
air flow.
Obviously,
Breathing occurs so automatically,
it's easy to overlook. Air from the
Fibromyalgia Network • (800) 853-2929 • www.fmnetnews.com
significant portion of the night with
years have documented that snoring is
9 Protruding discs; soft tissue injury
their blood oxygen concentration well
not a prerequisite for Upper Airway
below optimal levels. Lario suggested
Resistance Syndrome (UARS).
9 Enlarged thyroid gland (e.g.,
that alterations in breathing during
Graves' disease withgoiters and
sleep reduced muscle tissue oxygen-
UARS School of
Hashimoto's may increase scar
ation. This in turn produced morning
pain and other FM/CFS symptoms.
Three years later, Margherita
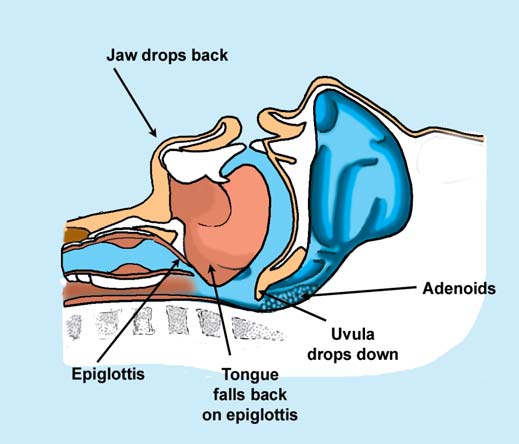
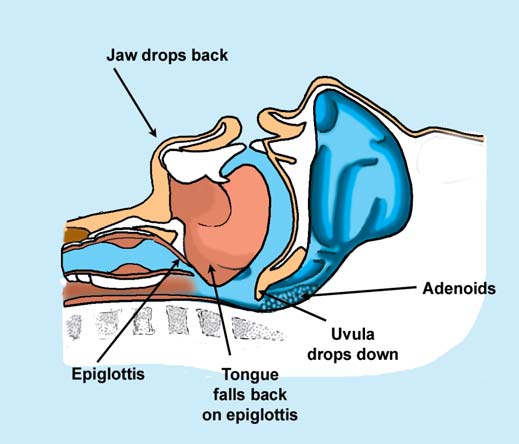
If you take the structures in the
In addition to the above, the
Sergi, M.D., of Italy published a
nose and throat (Diagrams A and B),
masseter muscle that stretches from
report on a possible link between
and place them in a supine sleeping
the upper check bone to the lower jaw
nighttime breathing and FM.2 An
position (Diagram C), it is clear to see
bone is often tight or knotted in
erratic breathing pattern was found in
how the airways can become ob-
people with FM. Taut masseter
15 out of 17 female FM patients,
structed—partially (UARS) or fully
muscles will draw the jaw up and
compared to 2 of the 17 controls.
(OSAS). The size of the airway is one
back towards the throat, especially
Again, the interrupted sleep pattern
major factor, but the characteristics of
when laying down. This may reduce
did not meet the criteria for OSAS,
the surrounding tissue (such as the
the size of the oropharnyx, and the
but it did produce twice as many
strength of the muscles and the
same is true of other tight muscles
arousals per hour in the patient group
amount of fat deposits in the area)
around the face or neck.
compared to the controls. The amount
also plays a role. For many people
of disturbed breathing during the night
with airway restrictions, difficulty
in FM patients correlated with symp-
sleeping and a variety of symptoms
toms of daytime fatigue and pain.
reminiscent of FM/CFS will develop.
FM patients often say they wake
Pulmonary volumes were the same in
As the lungs expand to suck in air,
up stiff and achy. This would make
the two groups, reducing the likeli-
there is so much resistance in the
sense if the oxygen supply to the
hood that the findings were caused by
airway that it takes much more effort
muscles was impaired during the
tight chest wall muscles.
to draw in each breath. This is hard on
night. Yet, people with Obstructive
The investigators suspected that
the heart, which is why physicians
Sleep Apnea Syndrome (OSAS), who
the breathing pattern could be caused
check for OSAS. Unfortunately,
have airflow blockages occurring at
by upper airway resistance (or flow
methods for testing UARS have only
least 5-10 times per hour, usually
restrictions) in the nose and throat
recently been developed, so this
don't have widespread pain. Their
regions, but discounted this possibility
disorder is often overlooked.
primary symptoms are morning
because many of the patients did not
Over ten years ago, scientists
headaches and daytime fatigue. FM/
snore. Although snoring is always
began studying people with UARS.3
CFS patients have these symptoms,
present OSAS (the loud vibrating
Researchers placed a small sensor
and many more. Could another sleep
noise produced when the airway
device in the nasal passage to measure
disorder explain this?
tissues collapse), researchers in recent
the amount of resistance in the airway
Alvarez Lario,
M.D., of Spain
Diagram C
addressed this
question and pub-
lished a follow-up
report in 1996.1 He
found that the level
of blood oxygenation
dropped significantly
during the night in 28
FM patients (all
female), compared to
15 healthy controls.
Patients did not meet
the criteria for OSAS,
but they did spend a
Diagram B
Fibromyalgia Network • (800) 853-2929 • www.fmnetnews.com
during sleep, so that people with
Half of the patients were recruited
because the effort required to exhale
UARS could be identified. As with
from their sleep center in Stony
kept them awake. Fortunately, CPAP
any "new" entity in medicine, UARS
Brook, NY, and the other half were
is not the only way to treat UARS.
is the subject of "put-downs" because
enrolled from a previous "survey
many doctors believe that OSAS is the
type" FM study that had nothing to do
OSAS or UARS?
only sleep-disordered breathing
with sleep. The investigators of the
. depends on how you grade them
condition that exists.4 UARS chal-
study wanted to include FM patients
lenges this traditional way of thinking,
who had not sought help for their
The foregoing study described the
just as fibromyalgia challenges the
sleep difficulties.
high prevalence of UARS in women
concept of real pain without obvious
Evaluation of the airflow dynam-
with FM. What about the overlap
tissue disease! UARS and FM/CFS
ics in all FM patients was compared to
between OSAS and FM? In 1993,
have more in common than just
that of 11 female UARS patients who
Kimberly May, M.D., looked for
had been identified by previous
sleep apnea in patients with FM (92
If the sleep disorder of FM/CFS
research projects. Between the over-
females and 25 males). The incidence
might really be that of UARS, why
night sleep lab data and the physical
of OSAS was low in the women (2%),
haven't you been tested for it? In
findings about the airflow openings,
but it turned out to be exceptionally
today's world, apnea remains King .
the study revealed that 27 of the 28
high (44%) in the group of men with
and there appears to be little room for
FM patients met the criteria for
FM.7 She concluded that sleep apnea
a Queen. Most physicians have been
UARS. The FM group averaged 30
may be a marker for undiagnosed FM
taught (and still may believe) that
arousals per hour, which was similar
in men. In addition, when the apnea
apnea is the only sleep-related breath-
to that found in the UARS group. In
was identified and treated, half of the
ing disorder that warrants further
addition, application of nasally
patients showed significant improve-
testing. The health insurance industry
administered continuous positive air-
ment in their sleep and FM symptoms.
further promotes this mindset by not
way pressure (CPAP) to overcome the
Therapies targeting OSAS and
covering sleep studies for the sole
resistance to air flow provided proof
UARS can produce a dramatic reduc-
purpose of diagnosing UARS, al-
that the frequent arousals were due to
tion in symptoms, so they are impor-
though many labs are capable of
the airway resistance. After three
tant to identify. The distinguishing
performing the necessary measure-
weeks on nasal CPAP, a substantial
features of OSAS and UARS are
ments. However, symptoms of chronic
reduction in FM symptoms (ranging
indicated in Diagram D. UARS
insomnia and suspicion of OSAS are
from 23-47%) was achieved.
involves a restriction in airflow during
usually sufficient grounds for ordering
Despite dramatic symptom
sleep, produces an alpha-EEG sleep
a sleep evaluation.
improvements, only 36% of the
pattern similar to that found in FM,
Christian Guilleminault, M.D.,
patients placed on CPAP were still
and causes more frequent arousals
at the Stanford Sleep Center in
using it nine months later. Although it
than OSAS. In fact, studies in recent
California, has directed a large
may seem odd that patients would
years have documented that individu-
number of the studies on UARS. He
discontinue a therapy that helped
als with UARS exhibit many symp-
discovered that UARS patients have a
them, there are many valid reasons
toms in common with FM, such as
higher frequency of structural abnor-
why FM patients halted CPAP.
daytime fatigue, difficulty falling
malities in their upper airway than
Two-thirds of the patients in the
asleep (insomnia), headaches, irritable
those without UARS, and has looked
study had rhinitis (at least two of the
bowel syndrome, and bruxism (teeth
at blood pressure, age, gender, and
following symptoms: chronic nasal
grinding caused by unconscious jaw
menopause as predisposing risk
stuffiness, post-nasal drip or nasal
movements during sleep).8 Even low
factors for the condition.5
allergies). When chronic sinus prob-
blood pressure, which is a frequent
lems exist, it increases nasal resis-
sign of orthostatic intolerance, and
FM Study Scores A+
tance and impairs one's ability to
cold extremities, are significantly
breathe nasally. Other situations that
more common in people with UARS.5
Due to the similarities between
prevented the CPAP usage included
OSAS and UARS are at two ends
UARS and FM, sleep researcher
skin rashes caused by the device's
of the spectrum of sleep-disordered
Avram R. Gold, M.D., at SUNY-
mask, inability to vary sleep position,
breathing, but OSAS occurs more
Stony Brook in New York, collabo-
and difficulty breathing against a
often in men while the prevalence of
rated with Joan Broderick, Ph.D., to
positive pressure. Many could not fall
UARS is greater in women.9 The
determine how often UARS occurred
asleep while breathing against a
blood oxygen levels typically dip
in 28 women diagnosed with FM.6
steady stream of pressurized air,
below 88% several times an hour in
Fibromyalgia Network • (800) 853-2929 • www.fmnetnews.com
Symptoms begin in early
(Approximately 40% men with FM)
childhood; prevalence
(Potentially most women with FM)
increases with age
Higher incidence in men
Higher incidence in women, with
(3:1 ratio of men to women)
significant rises at puberty & menopause
Blood oxygenation often dips below 90%,
Blood oxygenation hovers between 88-94%,
but number of arousals caused by breathing
but number of arousals caused by breathing
difficulties less than UARS.
difficulties greater than OSAS.
Patient always snores.
Snoring not always present.
Alpha-EEG anomaly rarely present.
Alpha-EEG anomaly usually present.
Unrefreshing sleep
Difficulty sleeping (insomnia)
Irritable bowel (abdominal pain/diarrhea)
Muscle pain and tenderness
Attention deficits
Tendency towards high blood pressure
Bruxism (teeth grinding)
Tendency towards low blood pressure
Common FM/CFS symptoms
(except high blood pressure)
Diagram D
OSAS patients, but there is no evi-
an ear, nose and throat (ENT) special-
dence of alpha-EEGs or awake-like
ist for treatment. Many of them had
brain waves intruding upon deep
their tonsils and/or adenoids removed,
sleep—a finding in patients with
but the choice of therapy was left up
UARS. This alpha-EEG in UARS
How can researchers be certain
to the ENT. Three months after
suggests that the brain is in a constant
that sleep-disordered breathing is
therapy, 55 children still had symp-
state of arousal, even during sleep,
caused by airway restrictions and not
toms of sleep-disordered breathing,
and this could be why the two syn-
by aging, hormones, or other factors?
but none met the adult criteria for
dromes exhibit different symptoms.10
The answer to this comes from sleep
OSAS. Guilleminault re-graded their
Conversely, the blood oxygen levels
studies performed on children ages 2
sleep study charts according to less
in UARS patients hover between 88-
to 12. Guilleminault analyzed the
strict criteria for OSAS (e.g., pediatric
92% throughout the entire night (a
medical records of 400 youngsters
guidelines) and 31 patients received
phenomenon observed in the FM
who had undergone overnight sleep
the OSAS score. The other 24 patients
studies by both Lario and Sergi).
tests because their parents noticed
were scored as UARS.
OSAS and UARS are bad for one's
irregular breathing patterns during
The OSAS group was slightly
health, but UARS tends to be more
sleep. He compared them to 60 age-
older than the UARS children and
destructive to the sleep process.11 This
matched healthy kids who did not
consisted of more boys than girls. Of
may also explain why UARS patients
have any signs of sleep-disordered
interest, close to 50% of the UARS
have more symptoms, which happen
breathing.12 This latter group served as
group had already been diagnosed
to overlap with those found in FM/
controls and were subsequently
with attention deficit hyperactivity
CFS patients. It is quite possible that
evaluated by an overnight sleep test
disorder. All 55 children were treated
many diagnosed with FM or CFS also
for comparison purposes.
more aggressively (adenoids and
have UARS, but they are not being
All 400 of the children with
tonsils removed; turbinates cut back),
treated for the latter.
breathing problems were referred to
and almost all symptoms went away.
Fibromyalgia Network • (800) 853-2929 • www.fmnetnews.com
In a separate study, Guilleminault
Lario BA, et al. Am J Med 101:54-60,1996.
the fact that OSAS and UARS begin
Sergi M, et al. Eur Respir J 14:203-8,1999.
evaluated children in this same age
very early in life.
Guilleminault C, et al. Chest 104:781-7, 1993.
group to determine why OSAS
Gutierrez AL, Rodenstein DO. Eur Respir J
develops in a child as opposed to
17:835-37, 2001.
Guilleminault C, et al. Am J Respir Care Med
UARS.13 Children with the structural
164:1242-7, 2001.
features outlined on page 12 were
Gold AR, et al. SLEEP 27(3):459-66, 2004.
more likely to have sleep-disordered
May KP, et al. Am J Med 94:505-8, 1993.
Treatments for UARS vary from
Gold AR, et al. Chest 123(1):87-95, 2003.
breathing. Those who had high blood
invasive surgeries to simple, self-
Collop NA. Chest 120(5):1432-33, 2001.
pressure tended to meet the pediatric
Guilleminault C. Chest 123(1):12-14, 2003.
administered remedies. Typically,
Guilleminault C, et al. Eur Respir J 17:838-47,
guidelines for OSAS, while those with
multiple approaches are needed and
low blood pressure (less than 80/60)
Guilleminault C, et al. Arch Pediatr Adolesc
sometimes the best place to start is
tended to have UARS. This difference
Med 158:153-61, 2004.
with a sleep study to determine if
Guilleminault C, et al. Pediatric Res 55:76-84,
implies that the autonomic nervous
you have UARS, and if so, its
system is dysfunctional in both
severity. Even if you don't have
conditions. However, the nervous
UARS, learn the best methods for
system is responding to the airway
keeping your airways clear so that
resistance by two different mecha-
breathing difficulties don't compound
nisms, generating two separate
your sleep disorder, pain, and other
conditions. Both studies underscore
Reprinted with permission from:
Fibromyalgia Network Journal
October 2004 (Issue #67)
Tucson, AZ 85751-1750
To join, call toll-free (800) 853-2929
or visit www.fmnetnews.com
$28 a year / $30 USD in Canada
Articles are for informational purposes only.
You must consult your physician for treatment.
Fibromyalgia Network • (800) 853-2929 • www.fmnetnews.com
Insomnia and Obstructive Sleep
cannot be applied
Apnea Syndrome (OSAS) are the two
most common sleep disorders. The
typical person with
overlap between the two is substantial
(40% of people with OSAS battle
insomnia).1 The reverse is also true:
many people with insomnia also
what about those who are younger,
Guilleminault writes, " . nonrecogni-
exhibit some form of sleep-disordered
female, and not overweight? These
tion of the syndrome (UARS) and the
breathing (apnea and the newly
people are rarely referred to sleep
anatomic abnormalities surrounding
identified Upper Airway Resistance
centers for overnight studies. If they
the upper airway responsible for its
Syndrome or UARS). Despite the
have UARS, it will go undetected and
symptoms will lead to complications
apparent link between the two condi-
untreated. In fact, these people will
and perhaps even development of
tions, they have remained on two
likely be given sleeping pills or sent to
sides of a rift, with insomnia on one
psychotherapy (a common approach to
According to Guilleminault, "A
side, and sleep-disordered breathing
treating chronic insomnia), but neither
study looking at the long term evolu-
on the other.
will correct a person's airflow limita-
tion of UARS has been done." The
Barry Krakow, M.D., director of
tions during sleep.
evolution from UARS to OSAS was
a sleep center in Albuquerque, NM,
So, what are the implications for
slow, but 6-7% of patients in the five-
explained in his 2004 editorial how
fibromyalgia (FM) patients? UARS
year study developed OSAS. This
insomnia is usually pushed aside to be
has been documented in a diverse
soon-to-be published study could be
viewed from a purely psychological
group of people with a variety of
highly significant, given that OSAS
perspective (i.e., a defect that should
primary symptom complaints, such as
develops over many decades.
be treated by mental health profes-
young children and teenagers with
The expansion of FM sleep
sionals).2 Conversely, OSAS is judged
attention deficits, as well as adults
research to include UARS is good
as a "real" disease that is rigorously
with fatigue, irritable bowel, trouble
news. However, one of the major
investigated and treated by pulmonary
sleeping, headaches, and the wide-
obstacles for detecting UARS with a
specialists. Referring to this division,
spread pain of FM.3 Since not all FM
high degree of accuracy is that pa-
Krakow says, "It's as though the right
patients fit the "OSAS profile," it is
tients must swallow a small transmit-
hand doesn't know what the left hand
important for treating physicians to
ter to measure the pressure in the
recognize that airflow can be re-
esophagus during sleep. The device is
Now that the tracks have been laid
stricted by a number of mechanisms,
tiny and inexpensive, but is seldom
to make a connection between insom-
and not simply the one that produces
used outside the realm of UARS
nia and sleep-disordered breathing,
research (i.e., it is not used to evaluate
sleep medicine is at a crossroads.
If UARS is a likely cause of
apnea . not even for research).
Which direction should sleep experts
insomnia, and OSAS is on the flip
Fortunately, a less expensive (but less
go? Krakow recommends that sleep
side of the "insomnia coin," does this
accurate) tool for detecting UARS
doctors consider sleep-disordered
mean that there may also be a connec-
was developed. In the meantime, sleep
breathing and insomnia as two sides
tion between UARS and OSAS?
studies that evaluate people with
of the same coin.
Recently, Guilleminault published an
insomnia, UARS, and mild OSAS
Breathing difficulties during
article reflecting the progress made in
may all lead to a better understand-
sleep, particularly UARS, may be the
the field of UARS over the past ten
ing of the nighttime frustrations
cause of most cases of insomnia.
years.4 He indicates that people with
faced by millions of patients with
Unfortunately, most doctors are only
UARS usually have structural abnor-
on the lookout for OSAS, and are
malities that restrict airflow, while
Smith S, et al. Sleep Med 5:449-456, 2004.
unaware of UARS. Christian
OSAS is neurological in nature. They
Krakow B. Sleep Med 5:431-433, 2004.
Guilleminault, M.D., of Stanford
appear to be two distinct syndromes,
Gold AR, et al. CHEST 123:87-95, 2003.
University, has shown that the com-
but research shows that, over time,
Bao G, Guilleminault CG. Curr Opin PulmMed 10:461-467, 2004.
mon profile for people with OSAS
UARS may actually become OSAS.
Fibromyalgia Network • (800) 853-2929 • www.fmnetnews.com

If you manage to sleep an extra
endings—were both increased during
major drawback of both of these
hour or two, is it a waste of valuable
the day. Cytokines are markers of
studies: Upper Airway Resistance
time? What if you are overwhelmed
systemic inflammation and are known
Syndrome (UARS) during sleep was
with work and decide to cut your
to cause symptoms of pain and
not evaluated in the patients with
sleep time short in order to get things
fatigue. Not surprisingly, they have
done? Given that FM/CFS patients are
been found to be elevated in patients
often exhausted and feeling short-
with FM.2,3 Cortisol, an alerting
changed on time, these are important
hormone, was also impacted by the
questions. Certainly, you want to do
sleep restriction. While the total
what is best for your health. Recogniz-
amount of cortisol produced was
There is evidence that insomnia
ing the connection between sleep and
unaffected, it peaked two hours earlier
may be caused by airway resistance
health, patients who responded to a
in the morning following the pattern
(e.g., UARS). If this is the case, and if
nondrug Fibromyalgia Network
of a two-hour decrease in sleep.
insomnia and apnea are on different
survey rated maintaining a consistent
Since reducing sleep time has
sides of the same coin (see previous
sleep routine as the third most effec-
serious consequences, does sleeping
article), then logically, there must be
tive self-help measure for controlling
more have a positive impact? A recent
some connection with cytokines and
study examined the benefits of
apnea. As it turns out, there is! Day-
increased sleep time.4 College stu-
time levels of IL-6 are elevated in
Toying with Sleep
dents (ages 18 to 23) were allowed to
people with apnea, which could
ignore their alarm clocks and sleep in
explain their daytime fatigue (IL-6
(on average an extra hour). After eight
causes fatigue in insomnia patients
Two studies indicate that extra
days, researchers found that in com-
too).7 After a one-month treatment of
sleep should not be viewed as op-
parison to baseline values, the ex-
apnea patients with Continuous
tional, but rather, as a priority for
tended sleep led to substantial im-
Positive Airway Pressure (CPAP),
healthy living and maximizing day-
provements in daytime alertness,
which kept the airways open at night
time function. The first study looked
reaction time, vigor, fatigue, and
so that patients could obtain restful
at the effects of modestly restricting
sleep, the levels of IL-6 were signifi-
the sleep of 25 healthy subjects (who
cantly decreased. A recent study found
had no sleep complaints) for one
that administering CPAP to FM
week.1 For the purpose of comparison,
patients who also met the criteria for
the participants were first observed in
UARS substantially reduced their pain
an overnight sleep lab for four days,
Cytokines IL-6 and TNF are both
and fatigue. One can speculate that,
with no changes to their sleep sched-
fatigue-inducing substances, so their
like the apnea patients, symptom
ule. Then, every day for one week, the
production during the daytime can
improvements in UARS and FM
subjects (13 men and 12 women) were
greatly hinder a person's performance.
should coincide with a drop in
awakened after only six hours of
Ordinarily, their peak secretion is
sleep. The participants were not
around 9 p.m., which explains why
allowed to nap and were told to stick
people get sleepy at this time of
to their regular schedules.
night. A study looking at people with
Vgontzas AN et al. J Clin & Metab89(5):211902126, 2004.
After just one week of this
chronic insomnia found that IL-6
Wallace DJ, et al. Rheumatology 40:743-
relatively modest (25%) sleep restric-
production shifted to the middle of
tion, the subjects' performance on
the day (2 to 3 p.m.), while TNF
Salemi S, et al. J Rheumatol 30(1):146-50, 2003.
various tests measurably declined.
secretion was elevated throughout the
Kamdar BB et al. Sleep Medicine 5:441-448,
This corresponded with significant
daytime hours.5 In a separate report,
changes in the body's production of
the same research team also found
Vgontzas AN et al. Metabolism 51(7):887-892, 2002.
several important substances. Among
that cortisol was overproduced in
Vgontzas AN, et al. J Clin Endo Metab
these, cytokine chemicals IL-6 and
people with insomnia, so even if they
Yokoe T et al. Circulation 107:1129-1134,
TNF—produced by the immune
wanted to fall asleep, this arousing
system but secreted through nerve
hormone could keep them awake.6 A
Fibromyalgia Network • (800) 853-2929 • www.fmnetnews.com

In the previous Network newslet-
like," says Gold. Only during the
ter, we reported that Continuous
sleep study, when the pressure setting
Positive Airway Pressure (CPAP)
is determined, must patients sleep on
reduced the symptoms of FM pain,
their back. "The airway is most
fatigue, sleep disorder, and gas-
Aggressive treatment of nasal
collapsible in this position."
trointestinal disturbances by 40 to
congestion tops the list for benefitting
If you already have insomnia, you
50%—a success rate unmatched by
your breathing at night. Sleeping
may think the CPAP machine will
any other therapy. Avram Gold,
position is also important. Laying on
keep you awake. Gold says that
M.D., at Stony Brook University in
one's back will force the base of the
patients are often prescribed Ambien
New York was the lead author.1 When
tongue and other structures to fall
to help them adjust to sleeping with a
Fibromyalgia Network asked Dr. Gold
back and occlude the airway. Ideally, a
mask and that symptoms of insomnia
about his approach for reducing the
person should sleep on their side, with
actually improve over time .
symptoms of FM, he emphasized, "I
a cervical neck support to keep the
do not treat FM; I DO treat flow
trachea straight.2 A tennis ball or
limitation during sleep in FM pa-
something similar can be attached to
the back of a nightshirt to prevent
Patients who are unable to tolerate
Even after months of follow-up,
people from sleeping on their back.
CPAP due to difficulties with the
the success rate does not improve.
Weight loss has long been promoted
mask, such as skin rash or problems
Why might this be? Three-quarters of
for the treatment of sleep apnea, but
breathing through the nose, may have
the FM patients in Gold's study had
recent research shows that it is of little
greater success with oral appliances.
chronic allergic rhinitis (AR) and
These devices are designed to bring
Gold suspects that the "high rate of
the lower jaw forward during sleep
poor nasal breathing in FM" could be
and were developed as an alternative
partially responsible for limited
to CPAP for patients with apnea.
CPAP is considered the first-
treatment success. "I cannot rule out,
Impressions of your upper and lower
choice therapy for UARS because the
however, that some other mechanism
teeth are used to make appliances out
pressure setting can be individualized.
is also playing a role in causing the
of plastic. They are not as effective as
It consists of a snug-fitting nasal mask
CPAP at preventing the airways from
with tubes connecting it to a machine
"I am quite convinced that when
collapsing, but for people with mild
that pressurizes the air flowing into
the work is done, it will demonstrate
airflow limitations (UARS and mild
the nose for breathing. Two types of
that inspiratory flow limitations
apnea), these devices may work well.5
machines are available, one which
during sleep are the unrecognized
A study involving mild apnea patients
automatically adjusts the amount of
cause of much human suffering," says
indicates that they often prefer the
pressure according to need, and
Gold. "Six years of working with
appliance over the CPAP machine, so
another which produces a "fixed"
women with UARS (Upper Airway
they may represent your next-best
pressure throughout the night. The
Resistance Syndrome) has convinced
auto CPAP delivers a lower average
Four key points about oral devices
pressure and may be preferred by
What are the primary approaches
include: (1) dentists specializing in
some patients. However, sudden
used for treating UARS, which in turn
sleep medicine and temporomandibu-
changes in air pressure may cause
should improve FM/CFS? Therapies
lar disorders are most likely to cus-
frequent arousals, so if you find you
for UARS may be divided into four
tomize an appliance for you, (2) if
cannot acclimate to one type of
categories in order of increasing cost
your physician is not aware of a
machine, try the other one before
and invasiveness: (1) Inexpensive/
provider, The American Academy of
giving up.4
Self-Help Strategies, (2) CPAP, (3)
Dental and Sleep Medicine's Web site
"Patients can sleep with nasal
Oral Appliances, and (4) Nasal
at www.dentalsleepmed.org may be
CPAP at home in any position they
Fibromyalgia Network • (800) 853-2929 • www.fmnetnews.com
helpful, (3) sore teeth and jaw in the
with insomnia seldom undergo a sleep
therapy), less money will be spent on
morning are common side effects that
study. This is particularly true for non-
medications and doctor's visits. She
should wear off shortly after removing
obese women. Fortunately, UARS is
will also be more alert behind the
the device . contact your provider for
steering wheel and less likely to have
adjustments if your jaw pain or sleep
Criteria: Asking Gold if any persis-
an auto accident that could be a very
worsens, and (4) major medical
tent symptoms should prompt doctors
expensive affair. These letters are
insurance companies often pay for
to order a sleep study, he responded:
remarkably effective."
oral appliances as "durable medical
"Fatigue/sleepiness . PERIOD. In my
Study Preparation: Many patients
experience (since 1999), it is rare to
fear that in order to undergo a sleep
find a patient with this symptom who
study, they must go off all of their
does not have inspiratory flow limita-
medications. Barry Krakow, M.D.,
tions (e.g., UARS) during sleep."
who routinely evaluates patients for
The fatigue of FM/CFS is usually
When asked if other tests could take
UARS, indicates that "people should
not viewed in relationship to chronic
the place of an overnight sleep study,
not change their sleep regimen for the
inflammation of the nasal or sinus
Gold's answer was "no." This is
study unless narcolepsy is suspected."
tissues (e.g., rhinosinusitis or AR). A
because large drops in blood oxygen
Otherwise, Krakow says that sleep
recent study by Alexander Chester,
levels (a detectable sign for most
doctors first want to evaluate patients
M.D., of Georgetown University, may
apnea patients using a portable
"as is." This includes bringing in all
help change this often overlooked
device) don't occur in UARS.
of your pillows and other comforts to
cause of fatigue! At the October 2004
Finding a Sleep Center: If your
best mimic your home environment.
meeting of the American Association
doctor prescribes a sleep study, you
After The Network published the
for CFS, Chester posed the question:
will need to locate a sleep center.
UARS article in the last issue, no
"Does functional endoscopic sinus
According to Gold, the best screening
physician or researcher in the FM
surgery reliably improve the fatigue
question is: "Do you make the diagno-
field has commented about it. Gold
associated with chronic
sis of UARS?" The most accurate
suspects that "the medical community
rhinosinusitis?" He presented a review
method of detecting UARS requires
is uncertain of what to make of this"
of the medical literature, showing that
patients to swallow a tiny pressure
(referring to UARS) because it
the fatigue levels greatly improve in
sensor, but this tool is used primarily
contradicts current opinions. He adds
patients after this form of surgery.7,8,9
in the research setting. Fortunately,
that more studies are needed to
What type of surgery is Chester
Gold points out a new alternative that
strengthen the concept that flow
referring to? It's an outpatient proce-
is capable of detecting most cases of
limitations during sleep could cause or
dure and the only form of surgery that
UARS. "Today, there is a new tool for
be partially responsible for FM/CFS.
Dr. Gold advocates for his patients. "It
measuring airflow during sleep that
Yet, Gold believes that with new
is surgery to improve nasal breathing
simplifies the detection of mild flow
medical ideas, "the tail can wag the
(trimming back the turbinates, correc-
limitation. It is a nasal/oral trans-
dog. Patients demanding answers will
tion of deviated nasal septum, removal
ducer." Only 25% of sleep centers
lead their physicians to learn new
of polyps)," says Gold. "These
have this device, so inquire about it
procedures reduce nasal resistance
before scheduling a study.
and at the very least, they can improve
Insurance Coverage: "All of our
a patient's compliance with nasal
patients have their studies covered by
Gold AR, et al. SLEEP 27(3):459-66, 2004.
CPAP." The procedure also improves
their insurers (as well as their treat-
Kushida CA, et al. Sleep Res Online 2(1):7-
sleep and reduces daytime fatigue due
ment) using the code 780.53 (sleep
Levy P, et al. SLEEP 19(9):S101-S110, 1996.
to enlargement of the airway. Aside
apnea with fatigue) and sometimes
Marrone O, et al. Sleep Medicine 5:247-51,
from this approach, other forms of
780.51 (sleep apnea with insomnia),"
surgery are generally considered a last
says Gold. "All of these patients have
Yoshida K. J Prosthetic Dentistry 87:427-30,2002.
fatigue/sleepiness and many have mild
Randerath W, et al. Chest 122(2):569-75,
snoring. In cases where the patient
Ragab SM, et al. Laryngoscope 114(5):923-
does not snore, the physician can
When & How they should be done
write a letter to the insurance com-
Chester AC. Arch Intern Med 163(15):1832-6,
pany citing my recent paper in SLEEP
Bhattacharyya N. Arch Otolaryngol H & N Surg
Typically, overnight sleep studies
and Dr. May's paper from 1993.1,10 I
are only ordered if a person is sus-
explain to the company that if we can
May K, et al. American J Med 94:505-8, 1993.
pected of having apnea, so people
get this woman on CPAP (or similar
Fibromyalgia Network • (800) 853-2929 • www.fmnetnews.com

It turns out that a stuffy nose can
AR symptoms peak between 5-6 a.m.,
So how does AR congestion
be detrimental to the quality of your
whereas they may be less bothersome
impact sleep? A study published over
sleep. Recent research reveals that
around 3 p.m. Morning stuffiness is
twenty years ago showed that
nasal congestion leads to daytime
usually about 20% worse than any of
microarousals (or disturbances) in
drowsiness.1 Allergic rhinitis (AR),
your daytime nasal symptoms.
sleep were ten times higher in patients
the medical term for sneezing and
Several factors may make your
with AR than in easy-breathing,
nasal congestion, is a risk factor for
stuffy nose worse in the early morning
healthy controls.5 In addition, these
developing sleep apnea, as well as its
hours.4 First, the nasal cavity swells
arousals were associated with abnor-
cousin, Upper Airway Resistance
up when you are laying down, causing
mal breathing patterns in the people
Syndrome (UARS).2 AR causes
nighttime secretions to accumulate.
with AR. Today, chronic nasal conges-
serious sleep disruption, which in turn
Second, your cortisol levels are the
tion is known to impede airflow and
leads to excessive sleepiness, de-
lowest at night. Cortisol is known for
increase the incidence of snoring—
creased alertness, concentration
its role in suppressing the immune
both of which may cause or worsen
deficits, irritability, and a diminished
system, so at low levels, immune
existing UARS and Obstructive Sleep
quality of life. Job performance and
substances are more likely to be
Apnea Syndrome (OSAS).
learning skills may also be impaired.
released, causing nasal inflammation
Clearly, nasal congestion can
The vast majority of patients with
and congestion. Third, the nervous
restrict breathing, which in turn
FM/CFS put up with the chronic
system promotes an expansion of the
impacts your sleep. So why doesn't
nuisance of AR. In fact, the symptom
blood vessels at night, which leads to
your doctor prescribe therapies that
cycles of FM and AR are strikingly
swelling of sinus tissues.
target AR when you complain of
similar. FM symptoms fluctuate over a
24-hour period in a cycle that was
documented by researcher Harvey
Daily 24-hour Cycles for FM Pain/Fatigue,
Moldofsky, M.D., of Toronto,
Canada. A graph of this cycle is
AR Symptoms and Cytokines IL-6/TNF
superimposed over the AR symptomcycle below. The pattern of thefatigue-enhancing cytokine shift (asdescribed on the previous page forinsomnia/apnea) is also shown forcomparison.
AR can exacerbate anyone's sleep
problems. For people with FM/CFSwho are already tired and struggling toget a good night's sleep, a betterunderstanding of what causes AR andhow to treat it is essential.
Stuffy Nose and Sleep
While it is possible that an
allergen in your bedroom is causing
you to wake up congested, there is a
more likely cause of this symptom.
Waking up each morning with a stuffy
nose is part of the AR symptom
cycle.3 Researchers have shown that
Fibromyalgia Network • (800) 853-2929 • www.fmnetnews.com
fatigue? A study indicates that people
piqued after working with I. Jon
rarely voice strong complaints about
Russell, M.D., Ph.D., at the Univer-
The possibility of a relationship
their stuffy nose, especially if it isn't
sity of Texas at San Antonio, to
between leukotrienes and FM has not
that bad in the doctor's office in the
document the three- and fourfold
been studied. Yet, out of all of the
middle of the day.6 If you have a
increases in substance P and nerve
nasal irritants produced by AR, these
chronic runny nose or wake up to
growth factor (respectively) in the
substances cause the most congestion.
nasal congestion in the morning, make
spinal fluid of patients with FM.
Two new drugs that block the action
a point of addressing this symptom at
Due to the lack of a blood-brain
of leukotrienes have been approved
your next doctor's visit.
barrier surrounding the sinuses,
for prescription sale in the United
substances released from the mast
States. As you will read in the section
cells into the nasal tissues have easy
below, they should benefit your sleep
. are also found in FM
access to the pain/fatigue regulating
to a greater extent than drugs that
centers in the brain, such as the
target histamine.
The many sinus irritants involved
thalamus. (The blood-brain barrier is
in AR are listed in the table below,
a boundary that prevents many
along with a brief description of their
substances from traveling from the
effects on sleep and nasal obstruction.
bloodstream into the brain tissues.) At
Cells within the nasal cavity, called
a scientific meeting on FM, sponsored
Now that the ties between AR and
mast cells, can cause congestion and
by the National Institutes of Health,
disturbed sleep have been explained,
induce sleep-disruption by releasing
Larson discussed her work that shows
it's time to make sure that your
their irritating contents into the nearby
cromolyn solution prevents mast cells
nighttime breathing is as effortless as
tissues. Examples include prostaglan-
from releasing their contents, even
possible! At first, decongestants might
dins, histamine, cytokines,
under conditions that would normally
seem like the ideal treatment. Nasal
leukotrienes, and neurotransmitters
trigger them into action. Therefore,
sprays in this category, such as Afrin,
involved in pain, such as substance P
cromolyn-based nasal sprays (such as
take only 10 minutes to clear the
and nerve growth factor. Although a
over-the-counter NasalCrom) may
upper airways. They work by shrink-
link between AR and FM is not
minimize the symptoms of AR. More
ing the blood vessels and drying up
established, University of Minnesota
details about Larson's mast cell
the tissue. The downside is that they
neuroscientist Alice Larson, Ph.D., is
research can be found on the Web site
make congestion worse if used for
investigating the role of mast cells in
for the American Fibromyalgia
more than four days (they are strictly
FM. Her interest in these cells was
Syndrome Association (AFSA) at
to be used for one or two nights, if atall). Oral decongestants, such as
pseudoephedrine (e.g., Sudafed), will
clear your passages in 30 minutes, butthey are stimulating agents that
Balances sleep/wake cycle
destroy sleep and cause drying of thenasal membranes, which aggravates
Increase deep level sleep
Inflammatory Cytokines * Associated with sleep
Usually, when people think of
(e.g., IL-1, TNF)
allergies, they think of antihistamines.
Unfortunately, histamine in the brain
plays a major role in maintaining
Substance P *
Interferes with sleep
wakefulness, so medications thatinterfere with its actions may cause
Nerve Growth Factor *
Interferes with sleep
sedation. The "first-generation"antihistamines, such as Benadryl, are
* Reported elevated in FM patients
able to cross the blood-brain barrier
All of the above are released from mast cells. For more information, visit the Ameri-
and induce sleepiness as well as
can Fibromyalgia Syndrome Association (AFSA) Web site at www.afsafund.org.
AFSA is an all-volunteer charity, whose overhead expenses are paid for by
cognitive dysfunction. Even if you
Fibromyalgia Network. This enables AFSA to spend over 90% of its contributions
choose to take these agents only at
directly on research. Contribute Online, or print out the order form to mail in your
bedtime, they won't curb nasal
contribution to AFSA today.
stuffiness in the morning because they
Fibromyalgia Network • (800) 853-2929 • www.fmnetnews.com
only work for 4-5 hours. Besides, they
usually administered
dry out the nasal passages and provide
twice daily. Due to the
minimal help with congestion (they
cyclic nature of AR
Decongestants (Oral and Nasal)
primarily relieve symptoms of sneez-
(worse in the morning
ing and itching). If you elect to use
and evening), it is
this category of meds, avoid the
optimal to use the
popular cold-season combinations that
spray immediately
Oxymetazoline (Afrin, Dristan)*
include decongestants that are detri-
upon waking and then
Phenylephrine (Alconefrin, Neo-Synephrine,
mental to sleep.
again before bedtime.
Vicks Sinex, etc.)*
mines have been purposefully de-
of AR medications
signed to work outside of the brain, so
work by blocking the
they don't cause as much sedation.
However, this side effect depends on
leukotrienes. Two such
the percentage of the drug that crosses
the blood-brain barrier. For example,
approved for prescrip-
Triprolidine (Actifed, Allephed)*
fexofenadine (Allegra) doesn't cross
tion sale in the United
Loratadine (Claritin, Alavert)*
the blood-brain barrier at all, while
States: Singulair
Certirizine (Zyrtec)
30% of Zyrtec passes through. For
(montelukast) and
Desloratadine (Clarinex)
this reason, Zyrtec is best taken at
Accolate (zafirlukast),
Fexofenadine (Allegra)
bedtime. This class of histamines can
but only Singulair has
provide 24-hour relief and does not
specific approval for
Leukotriene Blockers (Oral)
cause as much drying. Antihistamines
treating AR. Both have
Montelukast (Singulair)
in general do not effectively relieve
Zafirlukast (Accolate)
nasal congestion, but certain brands
superior to other AR
Nasal Sprays
may be better than others. Zyrtec and
meds available in pill
Clarinex (not the same as OTC
form, particularly for
Claritin) have been shown to be the
reducing nasal conges-
Azelastine (Astelin)
most effective drugs in this class for
tion and enhancing
Budesonide (Rhinocort)
sleep.3 Reduced nasal
Flunisolide (Nasalide, Nasarel)
Nasal sprays are another treat-
resistance and in-
Fluticasone (Flonase)
ment option, and are usually supple-
creased airflow rates
Mometasone (Nasonex)
mental in AR therapy. Four categories
found in patients
Triamcinolone (Nasacort)
of nasal sprays exist: antihistamines,
taking these medica-
Mast Cell Stabilizer:
steroids, cromolyn-based mast cell
tions may be respon-
Cromolyn Solution (NasalCrom)*
stabilizers, and saline solutions. The
sible for the improve-
latter two are available over-the-
ments in sleep, espe-
Saline Solution (Ocean, Ayr, etc.)*
counter. The role of cromolyn (e.g.,
cially since upper
* Available over-the-counter
NasalCrom) was discussed in the
airway resistance
previous section. Saline solutions,
appears to be the
such as Ocean Spray, simply keep the
primary cause of insomnia.
lead to better sleep. Using a nasal
sinus membranes moist and help flush
saline solution to flush and moisten
the irritants out of the nose. A study
The Ideal Therapy
the sinus membranes is useful no
comparing antihistamine and steroid
matter what pharmacological ap-
nasal sprays (azelastine versus
If money and insurance issues
proach is tried. Also, mast cell stabi-
flunisolide) demonstrated the superi-
weren't factors, what would be the
lizers, such as over-the-counter
ority of dilute steroid solutions for
ideal therapy for treating chronic nasal
NasalCrom spray, have a high safety
treating AR.8 In particular, the steroid
congestion and related AR symptoms?
record and are an alternative option
was shown to best reduce congestion
Singulair is the best orally acting
for people who cannot tolerate steroid
and improve sleep. One drawback of
medication. If side effects are not
sprays. A second-generation antihista-
steroid sprays, however, is that they
tolerable, the next best is Accolate. A
mine may help with itching, watery
take up to two weeks to reach their
steroid nasal spray can also be used to
eyes, or a runny nose. Zyrtec and
full effectiveness. These sprays are
enhance breathing, which ought to
Clarinex are the best two meds in this
Fibromyalgia Network • (800) 853-2929 • www.fmnetnews.com
category because they also treatnasal congestion. Take the time to
Q&A on UARS
find the AR treatment regimen thatworks for you. Your sleep is impor-
Most questions on Upper Airway Resistance Syndrome (UARS) have been
tant, and breathing easier at night is
answered on the pages that follow. Below are answers to the remaining
the key to functioning better during
Q How would Hyperbaric Oxygen Therapy affect UARS? What about
changes in barometric pressure?
END A HBOT was found effective for treating FM and likely does so by reducing
Craig TJ, et al. J Allergy Clin Immunol
UARS (it increases the inspiratory air pressure), but it is expensive. We
114:S139-45, 2004.
Young T, et al. J Allergy Clin Immunol
previously reported that FM symptoms flared when the barometric pressure
dropped. In light of UARS, this makes sense because lower atmospheric
Ferguson BJ. Otolaryngol Head Neck Surg
pressure also exacerbates airflow resistance.
Storms W W. J Allergy Clin Immunol
Q Are there any medicines to treat UARS?
Drugs that increase serotonin (e.g., many antidepressants commonly
Lavie, et al. Acta Otolaryngol 92(5-6):529-33,
prescribed for FM) may "slightly" aid UARS and mild apnea. Mirtazapine
Storms W, et al. J Allergy Clin Immunol 99(6
(Remeron), a sedating med that boosts serotonin may help as well, but
causes substantial weight gain.
Nayak AS, Schenkel E. Allergy 56(11):1077-80, 2001.
Q Do age or hormones influence UARS?
Berlin JM, et al. J Amer Orthopedic Assoc
Yes, during childhood and especially puberty, the tongue grows, thereby
reducing the airway size and precipitating UARS in predisposed individu-als. After menopause, the airway tissues may sag, increasing the incidenceof UARS and apnea. Estrogen replacement minimizes this latter phenom-enon.
Additional comments: (1) gasping for breath may be a sign of apnea or
UARS, (2) grinding teeth at night highly correlates with the presence of UARS,
(3) morning stiffness in FM and fluid retention in female apnea patients both
respond to treatment with CPAP, (4) if a previous sleep study has ruled out
apnea, this does not necessarily rule out UARS, and (5) Lin Chen, M.D., of
Philadelphia, PA, looked at the charts of 135 FM patients and found that apnea
was present in 20% of the women and 32% of the men. She suspects that the
remaining patients may have had UARS, and comments: "These data provide
additional reasons to consider sleep studies in fibromyalgia."
Reprinted with permission from:
Fibromyalgia Network Journal
January 2005 (Issue #68)
PO Box 31750, Tucson, AZ 85751-1750
To join, call toll-free (800) 853-2929
or visit www.fmnetnews.com
$28 a year / $30 USD in Canada
Articles are for informational purposes only.
You must consult your physician for treatment.
Fibromyalgia Network • (800) 853-2929 • www.fmnetnews.com
Source: http://doctorstevenpark.com/wp-content/uploads/2011/03/Sleep.Dr_.Gold_.pdf
REVUE PUBLIÉE TOUS LES TROIS MOIS PAR UN GROUPE DE PROFESSEURS DE L'INSTITUT D'ÉTUDES THÉOLOGIQUES FACULTÉ DE THÉOLOGIE DE LA COMPAGNIE DE JÉSUS – BRUXELLES OCTOBRE-DÉCEMBRE 2014 J.-M. CARRIÈRE S.J. Une loi qu'on ne peut saisir?Remarques sur la loi nouvelle dans l'Évangile de Jean . . . . . . . . . Le Synode extraordinaire des évêques sur la famille . . . . . . . . .
Informational Shocks, O�-Label Prescribing and the E�ects of Physician Detailing Bradley T. Shapiro∗ This Version September 1, 2015 (Preliminary Version. Comments Welcome.) Promotional strategies employed by pharmaceutical �rms to convince physicians to prescribe their products are the subject of considerable regulatory scrutiny. In partic- ular, regulators worry that �rms may use sales reps to try to convince physicians to