Operative risks of digestive surgery in cirrhotic patients
ARTICLE IN PRESS
Gastroentérologie Clinique et Biologique (2009) xxx, xxx—xxx
Vous êtes
autorisé à consulter ce document mais vous ne devez en aucun cas le télécharger ou l'imprimer.
Operative risks of digestive surgery in
cirrhotic patients
Risque opératoire du patient cirrhotique en chirurgie digestive
R. Douard , C. Lentschener , Y. Ozier , B. Dousset
a Service de chirurgie digestive et endocrinienne, hôpital Cochin, Assistance publique—Hôpitaux de Paris,faculté de médecine Paris Descartes, 27, rue du Faubourg Saint-Jacques, 75014 Paris, Franceb Service d'anesthésie—réanimation, hôpital Cochin, Assistance publique—Hôpitaux de Paris,faculté de médecine Paris-Descartes, 27, rue du Faubourg Saint-Jacques, 75014 Paris, France
Digestive surgery in cirrhotic patients has long been limited to the treatment of dis-
orders related to the liver disease (portal hypertension, hepatocellular carcinoma and umbilicalhernia). The improvement in cirrhotic patient management has allowed an increase in surgicalprocedures for extrahepatic indications. The aim of this study was to evaluate the operativerisks of such surgical procedures. Extrahepatic surgery in cirrhotic patients is associated withhigh mortality and morbidity. Emergency surgery, gastrointestinal tract opening (esophagus,stomach and colon), < 30 g/L serum albumin, transaminase levels more than three times theupper limit of normal, ascites, and intraoperative transfusions are the main risk factors forpostoperative death. In Child A patients, the operative risk of elective surgery is moderate andsurgical indications are not altered by the presence of cirrhosis. The laparoscopic approachshould be recommended because of the potentially lower morbidity. In Child C patients, oper-ative mortality is often higher than 40%; surgical indications must remain exceptional and nonoperative management has to be preferred. In Child B patients, preoperative improvement ofliver function is mandatory for lower risk surgery.
2009 Elsevier Masson SAS. All rights reserved.
La chirurgie digestive chez le cirrhotique a longtemps été limitée au traitement
des conséquences de la maladie hépatique (hypertension portale, carcinome hépatocellulaire,hernie ombilicale). L'amélioration de la prise en charge des cirrhotiques a permis une aug-mentation du nombre d'interventions réalisées pour des indications extrahépatiques. Le butde ce travail a été de faire le point sur le risque opératoire du cirrhotique dans ces indica-tions chirurgicales. La chirurgie extrahépatique chez le patient cirrhotique est associée à destaux élevés de mortalité et de morbidité élevés. Une intervention en urgence, une interven-tion portant sur le tube digestif (œsophage, estomac, côlon), une hypoalbuminémie inférieure à30 g/L, des transaminases supérieures à trois fois la limite supérieure de la normale, la présence
∗ Corresponding author.
E-mail address: (B. Dousset).
0399-8320/$ – see front matter 2009 Elsevier Masson SAS. All rights reserved.
Please cite this article in press as: Douard R, et al. Operative risks of digestive surgery in cirrhotic patients. GastroenterolClin Biol (2009), doi:
ARTICLE IN PRESS
R. Douard et al.
d'une ascite et l'existence de transfusions peropératoires sont les principaux facteurs de risquede mortalité postopératoire. Chez les malades Child A, le risque opératoire en chirurgie élec-tive est modéré et les indications chirurgicales ne sont pas modifiées par la cirrhose. La voied'abord laparoscopique doit être privilégiée car elle pourrait diminuer la morbidité. Chez lesmalades Child C, la mortalité opératoire dépasse souvent 40 % ; les indications chirurgicalesdoivent rester exceptionnelles et il faut privilégier les traitements non opératoires. Pour lesmalades Child B, il faut différer l'intervention et améliorer la fonction hépatique pour diminuerle risque opératoire.
2009 Elsevier Masson SAS. Tous droits réservés.
Digestive surgery in cirrhotic patients has long been limitedto the treatment of disorders related to the liver disease;portal hypertension, hepatocellular carcinoma and umbili-cal hernia. Improvement in cirrhotic patient managementhas improved patient survival and so more and more cir-rhotic patients are proposed for surgery. In this population,the number of surgical procedures for extrahepatic diseasehas consequently increased in a similar proportion. Althoughpostoperative morbidity and mortality are higher than gen-erally observed, few studies have examined the specific risksof digestive surgery in the cirrhotic patient. The purposeof this study was to review our knowledge of the opera-tive risk of digestive surgery in the cirrhotic patient. Theoperative risk related to hepatic surgery and portal hyper-tension will not be discussed in this review because they aredirectly related to the liver disease and its consequences.
We will first discuss the overall operative risk in the cir-rhotic patient and then examine the specific consequencesof surgery in this population before analyzing the different
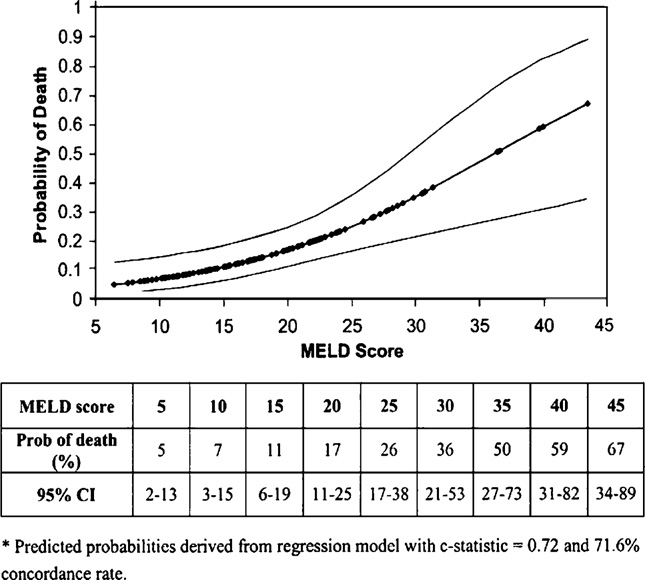
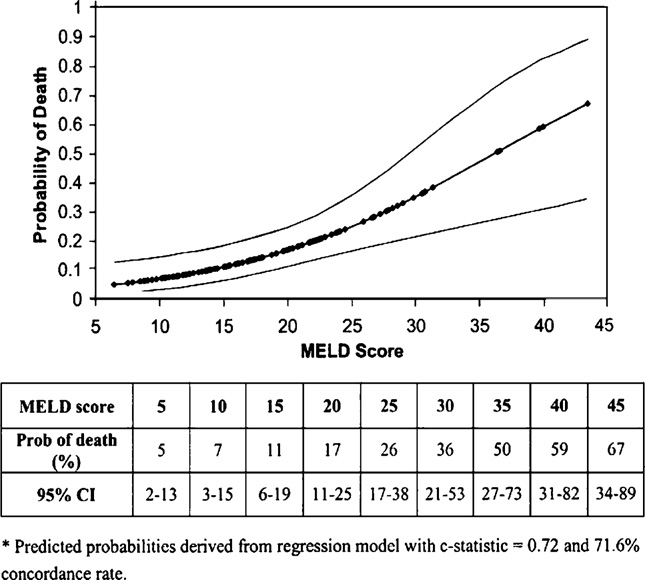
From Northup et al. mortality rate in the
types of surgery individually.
140 study cirrhotic patients at 30-day follow-up after generalsurgery according to the model for end-stage liver disease(MELD) score. The MELD score takes into account the inter-
Surgical risk in the cirrhotic patient
national normalized ratio, total bilirubin and serum creatininelevel.
Operative mortality in the cirrhotic patient is correlatedwith the severity of liver failure, irrespective of the scoreused to assess surgical risk The Child-Pugh (
cirrhotic patient undergoing general surgery procedures
and model for end-stage liver disease (MELD) scores
Operative risk is higher in patients with sev-
initially correlated with operative mortality for portal caval
eral factors The risk of postoperative death, even for a
anastomosis, can be transposed to general operative risk
major operation, in cirrhotic patients free of ascites, liver
for cirrhotic patients. More recently, Ziser et al. confirmed
failure and acute alcoholic hepatitis, and who have a normal
these data and identified eight factors significantly corre-
prothrombin level, is the same as observed in noncirrhotic
lated with postoperative morbidity and mortality in the
patients with the same pathological condition
Organ failure in the operated cirrhotic patient
Child-Pugh classification
Hemodynamics
Irrespective of the etiology, cirrhotic patients present a
hyperkinetic hemodynamic situation associating elevated
heart flow rate, low systemic blood pressure and low left
Serum bilirubin (mol/L)
ventricle afterload associated with splanchnic vasodilata-
Serum albumin (g/L)
tion This splanchnic vasodilation ‘‘steals'' vascular flow
from other vital territories such as the renal circulation
The Child-Pugh score is the sum of points (5—15). The Child-Pugh
Perioperative infusion of vasopressive amines may be
stage is established from the Child-Pugh score: A: 5 or 6 points;
necessary to counterbalance the loss of volumetric con-
B: 7—9 points; C: 10—15 points. For primary biliary cirrhosis, the
trol triggered by the surgery. Perioperative hemodynamic
points for serum bilirubin are as follows: 1 point for <70 mol/L,
variations may disclose an alcohol-related dilated cardiomy-
2 points for 70 to 170 mol/L and 3 points for >170 mol/L.
opathy (low cardiac output and/or rythm disorders) or
Please cite this article in press as: Douard R, et al. Operative risks of digestive surgery in cirrhotic patients. GastroenterolClin Biol (2009),
ARTICLE IN PRESS
Digestive surgery and cirrhosis
Factors associated with postoperative complication in cirrhotic patients
Mortality at 30 days (%)
Mortality at 6 months (%)
Child-Pugh score: 7—10
Elevated serum creatinine
Chronic respiratory disease
Preoperative infection
Upper digestive bleeding
Low interoperative blood pressure
Cryptogenetic cirrhosis
cirrhotic cardiomyopathy (left ventricular dysfunction)
effective A deficit in factors I, II, V, VII, IX, X due to
Pulmonary artery hypertension, defined as a mean pul-
defective hepatic synthesis is correlated with the severity
monary arterial pressure ≥ 25 mmHg, associated with a
of liver failure. Apparently primary fibrinolysis is usually
normal wedge pressure can coexist with cirrhosis. The risk
a complication, especially of infection. Hypercoagulation
is severe intra- and postoperative heart failure due to right
markers are common in patients with cirrhosis, who are
ventricle failure. The prevalence of coronary artery disease
susceptible to thromboembolic complications
is high in the cirrhotic population, where diabetes, alcoholabuse and smoking are common
Malnutrition
Malnutrition is a common finding in cirrhotic patients
and is correlated with the severity of liver failure. Dex-
Hypoxemia has been noted in 15 to 45% of cirrhotic patients
trose infusions may reveal deficiency in trace elements and
generally related to pleural effusion associated with
vitamins Today, clinicians consider that cirrhosis does
ascites The hepatopulmonary syndrome is defined by
not preclude renutrition but have been unable to formally
hypoxemia associated with an oxygen alveolar-arterial gra-
demonstrate an advantage in terms of postoperative mor-
dient without cardiac anomalies. The causal mechanism is
the shunt provoked by the dilation of the pulmonary precap-illary arterioles. A spontaneous ventilation hyperoxemia test
Infections in the operated cirrhotic patient
can be used to assess the correction of the hypoxemia and
Preexisting infection is an independent variable associated
quantify the shunt, predictive of postventilatory weaning
with postoperative morbidity (74%) and mortality at 30 days
and postoperative respiratory tolerance
(49%) and 6 months (60%) in the operated cirrhotic patientSystematic search for infection and preoperative treat-
Renal function and ascites
ment are thus mandatory in the cirrhotic patient. Cirrhosis is
Renal blood flow declines proportionally with the sever-
not an independent factor for operative site infection, irre-
ity of the cirrhosis-related hyperkinetic syndrome In
spective of the type of surgery (contaminated or not)
patients with liver failure, lean body mass is often dimin-
It is, however, a risk factor for infections distant from the
ished and glomerular filtation can be greatly reduced despite
operative site Consequently, the same antibiotic pro-
a normal serum creatinine level Serum levels must be
phylaxis must be scheduled for the cirrhotic patient as for
assayed repeatedly in cirrhotic patients receiving nephro-
the noncirrhotic patient with the same surgical risk
toxic drugs In a surgery context, blood or digestive
steady rise in medicalization of cirrhotic patients has led
fluid losses, constitution of a third sector, evacuation of
to a high prevalence of multiresistant germs, irrespective
abundant ascites, aggressive diuretic treatment and inap-
of the site of infection Nasal and rectal swabs might
propriate fluid and electrolyte restriction may aggravate the
be helpful in detecting carriers of multiresistant bacteria
impact of the hyperkinetic syndrome on the kidneys inducing
among previously medicalized cirrhotic patients In the
functional renal failure Ascites is a frequent compli-
cirrhotic patient, the frequency of postoperative infections
cation of abdominal surgery in the cirrhotic patient
is associated with translocation of gastrointestinal tract
The ascitic fluid arises via a diminution of the circulating
bacteria into the general blood stream, blood transfusion,
volume There is no evidence supporting the hypothesis
duration of surgery, severity of liver failure and insufficient
that postoperative restriction of fluid intake prevents post-
antibiotic therapy Preoperative decontamination
operative ascites There is no evidence that exsudative
of the digestive tract has not been found to decrease the
effusion associated with digestive resection and postopera-
rate of postoperative infections
tive chylous ascites are specific for this population
Quantitative changes in the synthesis of binding proteins cir-
Splenic sequestration of platelets leads to various degrees
culating in the blood stream leads to an increase in the
of thrombopenia. Circulating platelets are functionally
concentration of pharmacologically active free fraction of
Please cite this article in press as: Douard R, et al. Operative risks of digestive surgery in cirrhotic patients. GastroenterolClin Biol (2009), doi:
ARTICLE IN PRESS
R. Douard et al.
certain drugs, including antibiotics The distribution vol-
fat-free diet supplemented with medium chain triglycerides
ume of certain drugs can be increased as a result of fluid
may be insufficient. Drainage (or iterative puncture) may
and electrolyte retention Drug administration must be
be needed, combined with exclusive parenteral nutrition to
halt the production of this chylous ascites in 4 to 6 weeks.
Anesthesia and postoperative analgesia
No anesthesia protocol has been proven superior in the
Renal failure is observed in nearly 10% of operated cir-
operated cirrhotic patient Locoregional and peridural
rhotic patients may present functional renal failure
anesthesia and analgesia should be discussed for patients
a hepatorenal syndrome associated with severe liver
with normal coagulation factors and a platelet count above
failure renal failure subsequent to acute tubular
100,000/mm3 who would not be expected to develop
necrosis related to severe infection or multiorgan failure. It
major fibrinolysis postoperatively. Acetaminophen should be
is associated with ascites in 60% of patients and an infectious
used prudently Nefopam is not submitted to hepatic
syndrome in 50%. These associations show that the renal
metabolism; its efficacy in relieving postoperative pain has
failure is generally the consequence of other complications
been demonstrated for major digestive surgery Care-
(dehydration, infection, multiorgan failure).
ful titration of analgesic and secondary effects is requiredfor morphine prescription Inhibition of prostaglandin
synthesis in the kidneys by administration of nonsteroidal
Postoperative infection affects 13 to 40% of operated
anti-inflammatory drugs (NSAID) is a cause of renal ischemia
cirrhotic patients The rate is higher if the gas-
by reduced blood flow NSAID should be proscribed for
trointestinal tract has been opened In the cirrhotic
cirrhotic patients with ascites
patient, infections occur more readily late after surgery andgenerally do not involve the operative site. The most com-
Chronic viral hepatitis B and C
mon localizations include the lung (8%) and the urinary tract
Viral disease can be associated with renal failure,
or infected ascites, sometimes associated with septicemia
systemic hypertension, pulmonary vasculitis, cryoglobu-
The risk of spontaneous bacteriemia is higher
linemia, peripheral neuropathy, thyroid dysfunction and
in cirrhotic patients and increases further in the event of
thrombopenic purpura. The secondary effects of certain
postoperative liver failure
antiviral agents should be taken into account, e.g. epilep-sia, depression, leukothrombopenia with infection and risk
Complications involving the abdominal wall
of hemolysis with ribavirin
Ascites leakage through the abdominal wall is observedin 2% of operated patients, even if abdominal drainage is
Specific postoperative complications
installed. This leakage favors infections and evisceration.
Abdominal drainage may be insufficient to avoid this leakage
but significantly increases the risk of ascites infection
Postoperative ascites is one of the main complications
Abdominal drainage can, however, avoid excessive accu-
observed in cirrhotic patients undergoing abdominal surgery.
mulation of ascites which would exaggerate the leakage
The prevalence is greater than 20% The risk of post-
favoring the constitution of pseudocellulitis due to infiltra-
operative ascites is significantly increased by the presence
tion of the subcutaneous tissues and evisceration.
of intraoperative ascites and installation of drainage. The
An expert consensus recommends a solid suture of the
risk differs depending on the type of abdominal surgery;
abdominal wall using a slow resorbing thread and tight clo-
it is lower after parietal and biliary surgery. Postoperative
sure of the teguments using a cutaneous overcast stitch.
ascites in a cirrhotic patient can be divided into three cat-
Depending on the procedure performed and the anticipated
egories. Type I is correlated with liver failure. It is favored
risk of postoperative ascites, it is recommended either to
by postoperative fluid and electrolyte retention and readily
avoid drainage or to drain with a sterile aspiration system.
responds to treatment. Type II ascites is defined as unremit-ting and difficult to treat. More commonly observed after
supramesocolonic surgery (gastrectomy), this type of ascites
This complication is observed in 10% of operated cirrhotic
would be related to section of the lymphatic vessels drain-
patients but in only 5% of those undergoing abdominal
ing the liver and overloaded with interstitial fluid because of
surgery Because of this high rate special pre- and
the portal hypertension This is a lymphatic ascites of
postoperative measures are warranted to prevent digestive
hepatic origin producing a clear effusion with high protein
bleeding related to portal hypertension, i.e. betablockers
content, high lymphocyte count and a normal triglyceride
and/or endoscopic treatment, depending on the size of
level, similar to the ascites observed after liver transplanta-
the varices and the past history of rupture of esophageal
tion Type III postoperative ascites is a chylous effusion
varices In the cirrhotic patient, there is a higher risk of
related to the extravasation of lymphatic fluid rich in
bleeding from gastroduodenal stress ulcers; favoring factors
triglycerides arising from the interruption of the mesenteric
are severe sepsis, prolonged mechanical ventilation, liver
lymphatic flow because of the surgical section of the mesen-
failure and abdominal surgery Several studies have
teric or periaortic lymphatic vessels It can be observed
demonstrated an increased risk of nosocomial pneumopathy
after pancreatic, colonic or small bowel surgery. There is no
related to the use of antisecretory agents (compared with
relationship between the severity of the liver failure and
sucralfate) by alkalinization and colonization of the gastric
the development of chylous ascites. Treatment is difficult;
Please cite this article in press as: Douard R, et al. Operative risks of digestive surgery in cirrhotic patients. GastroenterolClin Biol (2009),
ARTICLE IN PRESS
Digestive surgery and cirrhosis
Severe liver failure
umbilical hernia and 2% after elective surgery Mortality
Severe liver failure is the most common complication, the
was zero in the two most recent studies reported by expert
cause of nearly 50% of postoperative deaths
centers and including 39 and 40 patients undergoing surgery
For the majority of patients, severe liver failure develops in
for umbilical hernia
a context of preoperative liver failure after an emergencyintervention opening the gastrointestinal tract. Prothrombin
below 50% and total serum bilirubin > 50 mol/L on the 5th
Surgery should be proposed solely for
postoperative day would be the best sign of postoperative
inguinal hernias and incisional hernia which become symp-
liver failure This 50-50 rule was defined for patients
tomatic or complicated. For patients with a moderately
undergoing liver resection of healthy or pathological liv-
altered liver function (Child A or B), cure for inguinal her-
ers but not for patients undergoing extrahepatic surgery.
nia can be achieved with acceptable morbidity In
It is difficult to differentiate liver failure from multiorgan
the presence of ascites, the same precautions must be taken
failure, common in this context.
as for umbilical hernias. The French Association of Surgeryreported a series of 38 inguinal hernias (one case of prosthe-
Surgery of the abdominal wall
sis interposition) and 23 incisional hernias (nine prosthesisinterpositions and two peritoneojugular shunts) Mor-
Hernias and incisional hernias are more common in the cir-
tality was 5.7% (91% elective surgery). The recurrence rate
rhotic patient than in the general population. Abdominal
was 8 to 10% recurrence being favored by weak wall
distention caused by the ascites and the loss of muscle mass
structure and ascites.
secondary to the poor nutritional status are the main risk
Irrespective of the type of parietal hernia or evisceration,
factors In the cirrhotic patient, the rate of abdominal
an extraperitoneal interposition prosthesis should be used in
wall hernia is 16% and reaches 24% in the presence of ascites
cirrhotic patients because of the higher risk of recurrence.
More than half of all hernias are umbilical; the
Furthermore, prostheses with a very low infectious risk are
rate is 4-fold higher in patients with ascites. Umbilical her-
available. This approach is however debatable if the patient
nias are also favored by Cruveilhier-Baumgarten syndrome
presents a complication (strangulation, rupture), cutaneous
(renewed patency of the umbilical vein). Treatments for
lesions or an infected ascites. If the ascites proves to be
inguinal hernia and incisional hernia must be distinguished
unresponsive to treatment, a TIPS would probably be the
from the treatment of umbilical hernia more specific to the
best solution since indications for peritoneojugular shunt
cirrhotic patient.
have disappeared. Should a cirrhotic patient on the livertransplantation list present a hernia or incisional hernia freeof complications, treatment may be delayed until the trans-
plantation procedure, although a TIPS while on the waiting
Indications retained for treating an umbilical hernia are
list might be useful to prevent the development of parietal
functional impairment and presence of a complication:
voluminous herniation, strangulation, rupture, cutaneous
The operative technique should prefer oblique or
lesions. Strangulation, rare in patients with ascites, is
transversal approaches, using a multilayer wall closure with
favored by a sudden drop in the volume of the effusion due to
slow resorption thread and overcast stitches to limit the risk
an umbilical rupture, evacuating puncture, vigorous medical
of ascites leakage and evisceration. If possible, drainage
treatment or installation of a peritoneojugular shunt
should be avoided, but when necessary, using a minimally
The goal is to treat the ascites before undertaking surgery.
traumatic technique with sterile aspiration. There is no con-
Specific complications after surgical treatment of an umbil-
traindication for laparoscopy in a cirrhotic patient
ical hernia are ascites, renal failure, wall infection, liverfailure and recurrent hernia. Ascitis is the main cause ofrecurrent parietal deficiency; 71% versus 4% without ascites
The predominant role of ascites in the developmentof postoperative complications explains why a simultane-
ous peritoneojugular shunt has been proposed in the event
Biliary surgery in cirrhotic patients is mainly represented
of refractory ascites or when an emergency treatment is
by gallstone. Incidence is increased because of the hyper-
required, despite the estimated 14% risk of infection
splenism and the subsequent hemolysis. Prevalence of
More recently, a small series of three cirrhotic patients who
gallstones in the cirrhotic patient is higher than in the gen-
underwent emergency surgery for a ruptured or strangu-
eral population, reaching 17 to 28% Cirrhosis, with
lated umbilical hernia reported treatment by parietal repair
cardiovascular disease, is the main risk factor for postchole-
and installation of a transjugular intrahepatic portosystemic
cystectomy mortality. A recent meta-analysis demonstrated
shunt (TIPS) on days 2, 0 and 2 of the herniorrhaphy
that, on average, cholecystectomy is performed in cirrhotic
These data, based on the efficacy of TIPS for the treat-
patients in more urgent situations and with higher morbidity
ment of refractory ascites suggest that TIPS should be
Laparoscopic cholecystectomy is currently the pre-
preferred over peritoneojugular shunt for the treatment of
ferred technique for cirrhotic patients Complications
umbilical hernia in patients with refractory ascites.
include ascites, liver failure, infection, kidney failure, diges-
In the series reported by the French Association of
tive bleeding and operative site bleeding. Morbidity is
Surgery, which included 81 patients who underwent surgical
related to the indication, the severity of the liver fail-
treatment of an umbilical hernia, overall mortality was 5%:
ure, blood transfusion and surgical approach. There were
11% after emergency surgery for ruptured or strangulated
no deaths in a study comparing the results of laparoscopic
Please cite this article in press as: Douard R, et al. Operative risks of digestive surgery in cirrhotic patients. GastroenterolClin Biol (2009), doi:
ARTICLE IN PRESS
R. Douard et al.
cholecystectomy (n = 26) with open cholecystectomy (n = 24)
of 52 cirrhotic patients who underwent endoscopic sphinc-
in Child A or B patients The conversion rate for
terotomy for common bile duct stones Considering this
the laparoscopic procedures was 12%, with significantly
evidence, several teams have proposed balloon endoscopic
decreased morbidity (19% versus 67%, p = 0.001) and lower
sphincteroclasia to avoid the risk of bleeding in cirrhotic
risk of transfusion (0% versus 33%, p = 0.008) Laparo-
patients, particularly Child C patients
scopic cholecystectomy in Child A or B patients is feasible
For the Child A or B patient, stones in the common
with a conversion rate of 5 to 9%, 5 to 10% morbidity
bile duct should be treated by endoscopic sphinctero-
and 0 to 1% mortality In the cirrhotic patient,
tomy followed by laparoscopic cholecystectomy. Endoscopic
laparoscopy is associated, as in the noncirrhotic patient,
sphincteroclasia would appear to be the best alternative for
with less blood loss, shorter operative time and shorter hos-
Child C patients, without secondary cholecystectomy.
pital stay Some authors suggested that in thecirrhotic patient preoperative coagulation disorders would
be more predictive of difficult operation and complicationsfor laparoscopic cholecystectomy than the Child score. Oth-
Excepting the survey published by the French Association of
ers have proposed subtotal cholecystectomy in this
Surgery data are lacking on the specificity of pancre-
context of increased risk of hemorrhage, especially for acute
atic surgery in the cirrhotic patient. In the published series,
or chronic cholecystitis. On the contrary, for the Child C
35 patients underwent surgery for chronic (n = 17) or acute
patient, cholecystectomy is associated with a prohibitive
(n = 3) pancreatitis, a malignant tumor (n = 14) or a benign
death rate of 23 to 50% severe liver failure, acute
tumor (n = 1). The procedures were resection (n = 9; left
cholecystitis and emergency surgery are common in this
pancreatectomy: 3, pancreaticoduodenectomy: 2, ampul-
type of patient. Most authors agree that medical treat-
lectomy: 2, atypical resection for acute pancreatitis: 2) and
ment should be proposed in this type of situation. If the
derivations (n = 26; digestive = 7, biliodigestive: 13, pancre-
medical approach is unsuccessful, or should pyocholecystitis
aticodigestive: 10). The transfusion rate was 44%, morbidity
develop, percutaneous cholecystostomy could be a solution
51% and mortality 20%. All three patients who had an emer-
The cholecystotomy should ideally be performed via
gency procedure died. All deaths occurred in patients whose
a transhepatic approach after transfusion of platelets and
gastrointestinal tract was opened. The univariate analysis
coagulation factors; percutaneous drainage of the ascites
identified emergency procedure and elevated transaminase
may be associated or precede the operation.
level as independently predictive of death.
Laparoscopic cholecystectomy is the procedure of choice
The findings suggest endoscopic (stent, endoscopic cys-
for the Child A or B patient with symptomatic gallstones or
togastrostomy, ampullectomy) and radiologic (percutaneous
acute cholecystitis morbidity is 10 to 15%, mortality 0
drainage of pancreatic abscesses) treatments should be pre-
to 1% and conversion rate 5 to 9%. For the Child C patient,
ferred in cirrhotic patients with an inflammatory disease or
medical treatment should be proposed and, if necessary,
tumor of the pancreas. The rare indications for resection
combined with percutaneous cholecystostomy.
should be reserved for elective procedures in Child-Pugh Apatients without elevated transaminases.
Common bile duct stones
Treatment of stones in the common bile duct is more diffi-
cult in the cirrhotic patient because the procedure involves
cholecystectomy and extraction of the stone from the bileduct. Stone extraction is difficult because of the portal
Studies on gastric surgery in the cirrhotic patient have
hypertension and the risk of injuring neighboring varices or
focused on the treatment of complications of peptic ulcers
triggering hemobilia with the extraction instruments. In the
and gastric cancers.
series reported by the French Association of Surgery, morbid-
Peptic ulcers appear to be more common in cirrhotic
ity in 31 patients undergoing surgery for a common bile duct
patients, affecting 8 to 20% of patients The propor-
stone was 29%, with 9.6% mortality. In a series of 87 cirrhotic
tion of cirrhotic patients among patients with peptic ulcer
patients who underwent surgery for gallstones (n = 53) or
appears to be higher than the equivalent proportion in the
common bile duct stones (n = 34), morbidity was 15% and
general population: 9% among patients with hemorrhagic
mortality 4.5%. Two factors had a significant impact on mor-
ulcer, 6% among patients with a perforated ulcer and 8%
bidity and mortality: Child-Pugh stage C (morbidity 32%,
among patients aged 65 years-old and over with a symp-
mortality 12%) and presence of a stone in the common duct
tomatic ulcer The mortality of emergency surgery for
(morbidity 24%, mortality 9%) Another team compared
complicated peptic ulcer in the cirrhotic patient is very
surgery (n = 9) versus endoscopic sphincterotomy (n = 7) for
high, ranging from 23 to 64% Prognostic fac-
this indication. Mortality was 44% versus 14.3% (p < 0.01) and
tors impacting mortality are severity of the liver failure and
morbidity 66% versus 14% (p < 0.01) with a mean blood loss
presence of ascitis With the advent of proton
of 1576 mL after surgery highlighting the benefits for endo-
pump inhibitors, eradication of Helicobacter pylori and the
scopic sphincterotomy Another study confirmed these
development of endoscopic hemostasis techniques, the effi-
findings and reported 67% morbidity after surgery versus 22%
cacy of simple suture of the perforation in a patient with
after endoscopic sphincterotomy with no significant differ-
peritonitis due to the perforated ulcer has been demon-
ence for mortality Endoscopic sphincterotomy has thus
strated, dramatically reducing the indications for surgery
become the gold standard for common bile duct stones, fol-
and gastric resections for hemorrhagic ulcers. Excepting rare
lowed by elective laparoscopic cholecystectomy. The risks
cases, emergency surgery for complicated ulcers does not
must not however be overlooked; mortality was 7% in a series
require resection, although the gastrointestinal tract must
Please cite this article in press as: Douard R, et al. Operative risks of digestive surgery in cirrhotic patients. GastroenterolClin Biol (2009),
ARTICLE IN PRESS
Digestive surgery and cirrhosis
be opened. Two controlled studies have demonstrated the
• pleural effusion (26%);
efficacy of laparoscopic suture of perforated ulcers
• anastomotic fistula (24%);
by extrapolation, laparoscopic suture of perforated ulcers
• infection (22%);
can be proposed for cirrhotic patients.
• renal failure (17%).
Two series from Japan have reported results of surgi-
cal treatment of gastric cancer in cirrhotic patients. The
Twelve patients (26%) died. Factors predictive of fatal
first was a series of 37 operated patients (24 superficial can-
outcome included liver failure (prothombin < 60%, serum
cers); morbidity was 20%, mortality 0%, and 5-year actuarial
albumin < 30 g/L, serum bilirubin > 35 mol/L), transfusion
survival 51% The second study included 39 operated
of more than three packed cell units and anastomotic fis-
patients (28 superficial cancers); morbidity was 26%, mortal-
tula. These findings illustrate the risks of esophagectomy in
ity 10.3% and 5-year acturarial survival 64% for superficial
the cirrhotic patient; mortality is greater than 20% and the
cancers and 14% for invasive cancers Causes of late
rate of anastomotic leakage greater than 20%. This surgery
death were mainly related to the liver disease.
should be reserved for Child-Pugh A5 patients with T1-T3 N0
The series of 66 operated cirrhotic patients with gas-
tumors who are free of ascites and transaminase elevation.
tric disease reported by the French Association of Surgery
For all other patients, non-surgical treatment with exclusive
included patients with a noncomplicated benign disease
chemoradiotherapy should be proposed
(n = 12), hemorrhagic or perforated ulcer (n = 35), malignanttumor (n = 17) or another disease (n = 2). Mortality was 23%,
significantly higher in patients with ascites and low serumalbumin; mortality was not affected by gastric disease orby type of surgery (simple suture, vagotomy, gastrectomy).
Particularities of colorectal cancer in the cirrhotic
Overall morbidity was 56%, most deaths related to ascites,
infection, and renal failure
Hepatic metastasis is less frequent in cirrhotic patients than
For perforated ulcers in the cirrhotic patient, laparo-
non-cirrhotic patients For patients with chronic
scopic suture is the treatment of choice. In the event of
viral hepatitis B, colorectal cancer-related survival is longer
a hemorrhagic ulcer, endoscopic hemostasis should be fol-
than in noncirrhotic patients due to the lower rate of liver
lowed, if necessary, by surgery in order to maximize elective
involvement Reporting experience of the Mayo clinic,
procedures. Direct hemostasis with arterial ligature and
Gervaz et al. observed a lower rate of hepatic
vagotomy should be preferred over vagotomy-antrectomy.
metastasis in cirrhotic patients (10%) and noted that survival
In cirrhotic patients, who have a gastric cancer, surgery is a
in these patients was long enough for hepatic metastases to
very high risk option in the presence of ascites, hypoalbu-
develop. An alteration of the extracellular matrix stim-
minemia, and Child-Pugh stage C. For stage A and B patients,
ulation of the Kupffer cells defective angiogenesis
it would be preferable to propose type D1 dissection and to
and presence of spontaneous portalcaval shunts
avoid dissection of the hepatic pedicle because of the risk
been proposed to explain this lower risk of hepatic metasta-
of type II lymphatic ascites.
sis. Because of the different prognostic course of colorectalcancer, Child-Pugh stage remains the main prognostic factorfor long-term survival of these patients.
Indications for surgery in the cirrhotic patient
Seven percent of patients with cancer of the esophagus
Two main series have reported results of colorectal cancer
also have cirrhosis Overall morbidity after esophageal
in cirrhotic patients: the Mayo clinic series the
surgery in the operated cirrhotic patient is twice that
French Association of Surgery series The Mayo clinic
observed in the noncirrhotic patient: 17 to 21% versus 3
reported 72 operated cirrhotic patients with colorectal can-
to 8% Mortality does not appear to be affected
cer: Child A (43%), Child B (42%), Child C (15%). Mortality was
by the type of operation; the rate of esophagogastric fis-
13% and morbidity 46%. Fistulae developed in 3%. Cirrhosis-
tulization ranges from 9 to 11% Morbidity, especially
related complications were mainly secondary to liver failure
lung disease, is significantly increased by cirrhosis
and included infection and digestive bleeding. Factors pre-
Mortality is correlated with preoperative liver failure, pro-
dictive of postoperative death were elevated serum bilirubin
thrombin < 60%, presence of ascites and hypoalbuminemia
and low prothrombin level. Ten percent of the patients
The risk of postoperative liver failure is higher in
developed liver metastases. Overall 1, 2 and 3-year survivals
the event of acute alcoholic hepatitis; it is recommended
were 69, 49 and 35%. Survival was better in Child A patients
to wait until transaminase levels return to normal before
than Child B or C patients. Multivariate analysis identified
attempting surgery. For most teams, the presence of Child B
serum albumin and prothormbin level as affecting survival.
or C cirrhosis proscribes surgery The series of 53 patients
Conversely, Tumor Node Metastasis (TNM) staging had no
undergoing esophageal surgery reported by the French Asso-
impact on survival, suggesting that the prognosis in these
ciation of Surgery included 46 patients who had elective
patients depends mainly on liver function.
resections followed by esophagogastric anastomosis; 26% of
In the French Association of Surgery series, 54 cirrhotic
the patients had ascites and 81% received a blood transfu-
patients underwent colorectal surgery: 11 for divertic-
sion. Complications developed in 72% of patients:
ular disease and 19 for other diseases. An emergencyprocedure was necessary for 17 patients for peritonitis
• ascites (39%);
(n = 10), obstruction (n = 5), hemorrhage (n = 2). Among the
• pneumopathy (30%);
56 patients who had a resection-anastomosis, 7% developed
Please cite this article in press as: Douard R, et al. Operative risks of digestive surgery in cirrhotic patients. GastroenterolClin Biol (2009), doi:
ARTICLE IN PRESS
R. Douard et al.
a fistula. Overall morbidity was 51%, mainly ascites and
exceptional. Nonoperative endoscopic or percutaneous radi-
infection. Overall mortality was 23%. Emergency surgery
ological treatments should be preferred.
and presence of intraoperative ascites were predictive of
For Child B patients, a precise assessment of the liver fail-
operative death. It should be remembered, however, that
ure and the operative risks as a function of the projected
in the cirrhotic patient a protective stomy has specific
operation is required to adapt management practices. The
complications including ascites leakage, ascites infection,
operative risk may be reduced by improving liver function,
stomial disinsertion, peristomial hernia, peristomial eviscer-
reducing the ascites, improving the nutritional status and
ation and peristomial varices
normalizing elevated transaminase levels; surgery may have
Colorectal surgery in the cirrhotic patient is associated
to be delayed but not proscribed. The presence of por-
with higher morbidity and mortality than in the noncirrhotic
tal hypertension with esophageal varices ≥ grade 2 warrants
patient. Factors predictive of operative mortality are those
primary prophylaxis with betablockers. If the postopera-
of surgery in the cirrhotic patient: emergency procedure,
tive risk of hemorrhage is considered high, or if there
serum albumin < 30 g/L, presence of ascites, low prothrom-
is a contraindication for betablockers, prophylactic elas-
bin These factors are included in Child-Pugh staging
tic ligation of the esophageal varices may be proposed.
allowing the distinction of two categories of patients: Child A
Persistence of refractory ascites or severe portal hyperten-
patients who can undergo elective surgery with an expected
sion (history of digestive bleeding by rupture of esophageal
postoperative period comparable to noncirrhotic patients
varices and ≥ grade 2 varices) despite well-conducted medi-
and Child C patients with a high operative mortality (40—50
cal treatment may require preoperative TIPS, which, in this
%) for which surgery should be undertaken only exception-
indication, should replace the peritoneojugular shunt
ally. For Child B patients, the degree of liver failure must
In emergency situations, it is best, whenever possi-
be assessed carefully; correction of an ascites, with TIPS if
ble, to defer surgery of the cirrhotic patient, preferring
necessary, may delay surgery.
a semi-elective intervention. Intensive care and nonoper-ative treatments would be more advisable in these high-riskpatients.
Regarding surgical technique for open procedures,
oblique or transversal approaches are preferable. A multiple
In the cirrhotic patient, extrahepatic surgery is associ-
plane closure of the abdominal wall using slow absorption
ated with higher morbidity and mortality. In the series
thread and overcast stitches is advisable to reduce the risk of
of the French Association of Surgery which collected data
ascites leakage, evisceration, incisional hernia and drainage
on 760 patients, including a very large majority of Child A
should, whenever possible, be avoided. If necessary, non-
patients, overall mortality was 14%. Factors predictive of
traumatic minimal aspiration drainage can be used. Despite
operative mortality were emergency procedure, operation
the lack of solid evidence, it is probably useful to pre-
involving the digestive tract (esophagus, stomach, colon),
pare the colon to reduce the risk of bacterial contamination
serum albumin < 30 g/L, transaminase level more than three
for esophageal, gastric or colorectal surgery. Rigorous sur-
times above the upper limit of normal, presence of ascites
gical technique with special attention to hemostasis and
and intraoperative blood transfusion
lymphostasis is necessary; for cancer surgery, where the
Can the operative risk be reduced for the cirrhotic
prognosis is probably more related to the cirrhosis than the
patient undergoing digestive surgery?
cancer, there is evidence in the literature arguing against
It is important to carefully search for cirrhosis before
extensive nodal dissection.
undertaking abdominal surgery. The problematic is sim-
Hepatotoxic and nephrotoxic agents should be avoided
ple when the cirrhosis is known, for carriers of hepatitis
for anesthesia and perioperative intensive care; it is
C virus, or when chronic alcohol abuse is obvious. For
approximately 20% of patients, however, cirrhosis may go
tors (prothrombin level < 50%, fibrinogen < 1 g/L), schedule
unrecognized and be discovered intraoperatively. Focus
platelet transfusion when the platelet count is less than
should be placed on asymptomatic patients whose imag-
50,000/mm3, and maintain intra- and postoperative sys-
ing work-up displays splenomegaly, hepatic dysmorphism or
temic, renal and hepatic hemodynamics, even at the cost
spontaneous portosystemic shunts as well as patients with
of aggravating postoperative ascites if necessary. Intensive
an isolated thrombopenia, sometimes the inaugural sign of
care must focus on nutritional status and identification and
well-compensated cirrhosis A FibroScan can be useful
rapid treatment of infections, crucial challenges for the
before surgery; its contribution should be assessed
postoperative outcome of the cirrhotic patient.
Three factors known to aggravate the operative risk
should be identified: ascites, serum albumin < 30 g/L,transaminase elevation. For Child A patients, the operative
Conflict of interests
risk of elective surgery is acceptable and surgical indicationsneed not be changed from those proposed for non-cirrhotic
patients, if management is carefully adapted. The laparo-scopic approach should be preferred because it reduces therisk of bleeding, respiratory disorders, infection and abdom-
inal wall defects as well as the prevalence of postoperativeascites.
[1] Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams
For Child C patients, however, operative mortality
R. Transection of the oesophagus for bleeding oesophageal
is often 40%; indications for surgery should remain
varices. Br J Surg 1973;60:646—9.
Please cite this article in press as: Douard R, et al. Operative risks of digestive surgery in cirrhotic patients. GastroenterolClin Biol (2009),
ARTICLE IN PRESS
Digestive surgery and cirrhosis
[2] Northup PG, Wanacker RC, Lee VD, Adams RB, Berg CL. Model
[21] Zwaveling JH, Maring JK, Klompmaker IJ, Haagsma EB, Bot-
for end-stage liver disease (MELD) predicts non-transplant sur-
tema JT, Laseur M, et al. Selective decontamination of the
gical mortality in patients with cirrhosis. Ann Surg 2005;242:
digestive tract to prevent postoperative infection: a random-
ized placebo-controlled trial in liver transplant patients. Crit
[3] Ziser A, Plevac DJ, Wiesner RH, Rakela J, Offord KP, Brown
Care Med 2002;30:1204—9.
DL. Morbidity and mortality in cirrhotic patients undergoing
[22] Mimoz O, Incagnoli P, Josse C, Gillon MC, Kuhlman L, Mirand A,
anesthesia and surgery. Anesthesiology 1999;90:42—53.
et al. Analgesic efficacy and safety of nefopam vs propacetamol
[4] Belghiti J. Chirurgie œsophagienne chez le cirrhotique. In:
following hepatic resection. Anaesthesia 2001;56:520—5.
Belghiti J, Gillet M, editors. La chirurgie digestive chez le cir-
[23] Williams RL. Drug administration in hepatic disease. N Engl J
rhotique. Paris: Monographies de l'AFC; 1993, p. 61—72.
[5] Blei AT, Mazhar S, Davidson CJ, Flamm SL, Abecassis M,
[24] Lentschener C, Ozier Y. What anaesthetists need to know
Gheorghiade M. Hemodynamic evaluation before liver trans-
about viral hepatitis. Acta Anaesthesiol Scand 2003;47:794—
plantation: insights into the portal hypertensive syndrome. J
Clin Gastroenterol 2007;41(Suppl. 3):S323—9.
[25] Valla DC. Complications postopératoires chez les malades
[6] Arroyo V, Jimenez W. Complications of cirrhosis. Renal and
atteints de cirrhose. In: Belghiti J, Gillet M, editors. La
circulatory dysfunction. Lights and shadows in an important
chirurgie digestive chez le cirrhotique. Paris: Monographies de
clinical problem. J Hepatol 2000;32:157—70.
l'AFC; 1993, p. 41—52.
[7] Myers RP, Cerini R, Sayegh R, Moreau R, Degott C, Lebrec D,
[26] Arroyo V, Bernardi M, Epstein M, Henriksen JH, Schrier RW,
et al. Cardiac hepatopathy: clinical, hemodynamic and his-
Rodes J. Pathophysiology of ascites and functional renal failure
tologic characteristics and correlations. Hepatology 2003;37:
in cirrhosis. J Hepatol 1988;6:239—57.
[27] Guidelines for the management of complications in patients
[8] Swanson KL, Wiesner RH, Krowka MJ. Natural history of
with cirrhosis. Gastroenterol Clin Biol 2008; 32:887—97.
hepatopulmonary syndrome: impact of liver transplantation.
[28] Zarski JP, Bichard P, Bourbon P, Tournery A, Demongeot
J, Rachail M. La chirurgie digestive extrahépatique chez
[9] Mimoz O, Soreda S, Padoin C, Tod M, Petitjean O, Benhamou
le cirrhotique : mortalité, morbidité, facteurs pronostiques
D. Ceftriaxone pharmacokinetics during iatrogenic hydrox-
préopératoires. Gastroenterol Clin Biol 1988;12:43—7.
yethyl starch-induced hypoalbuminemia: a model to explore
[29] Belghiti J. La chirurgie digestive chez le cirrhotique : résultats
the effects of decreased protein binding capacity on highly
globaux. In: Belghiti J, Gillet M, editors. La chirurgie diges-
bound drugs. Anesthesiology 2000;93:735—43.
tive chez le cirrhotique. Paris: Monographies de l'AFC; 1993,
[10] Brown MW, Burk RF. Development of intractable ascites follow-
ing upper abdominal surgery in patients with cirrhosis. Am J
[30] Silvain C, Besson I, Ingrand P, Mannant PR, Fort E, Beauchant
M. Prognosis and long-term recurrence of spontaeous bacterial
[11] Sultan S, Pauwels A, Poupon R, Levy VG. Ascite chyleuse du
peritonitis in cirrhosis. J Hepatol 1993;19:188—9.
cirrhotique. Étude rétrospective de 20 cas. Gastroenterol Clin
[31] Jouët P, Grange JD. Flore bactérienne et cirrhose. Gastroen-
terol Clin Biol 2003;27:738—48.
[12] Northup PG, Sundaram V, Fallon MB, Reddy KR, Balogun RA,
[32] Martin LF, Booth FV, Reines HD, Deysach LG, Kochman RL,
Sanyal AJ, et al. Hypercoagulation and thrombophilia in liver
Erhardt LJ, et al. Stress ulcers and organ failure in intubated
disease. J Thromb Haemost 2008;6:2—9.
patients in surgical intensive care units. Ann Surg 1992;215:
[13] Buyse S, Durand F, Joly F. Évaluation de l'état nutrition-
nel au cours de la cirrhose. Gastroenterol Clin Biol 2008;32:
[33] Daley RJ, Rebuck JA, Welage LS, Rogers FB. Prevention of
stress ulceration: current trends in critical care. Crit Care Med
[14] Plank LD, McCall JL, Gane EJ, Rafique M, Gillanders LK, McIlroy
K, et al. Pre- and postoperative immunonutrition in patients
[34] Belghiti J, Cherqui D, Langonnet F, Fekete F. Esophagogastrec-
undergoing liver transplantation: a pilot study of safety and
tomy for carcinoma in cirrhotic patients. Hepatogastroenterol-
efficacy. Clin Nutr 2005;24:288—96.
[15] Selberg O, Bottcher J, Tusch G, Pichlmayr R, Henkel E, et
[35] Aranha GV, Greenlee HB. Intraabdominal surgery in patients
al. Identification of high- and low-risk patients before liver
with advanced cirrhosis. Arch Surg 1986;121:275—7.
transplantation: a prospective cohort study of nutritional and
[36] Balzan S, Belghiti J, Farges O, Ogata S, Sauvanet A, Delefosse D,
metabolic parameters in 150 patients. Hepatology 1997;25:
et al. The ‘‘50-50 criteria'' on postoperative day 5: an accurate
predictor of liver failure and death after hepatectomy. Ann
[16] Pessaux P, Msika S, Atalla D, Hay JM, Flamant Y, French Asso-
ciation for Surgical Research. Risk factors for postoperative
[37] Franco D, Charra M, Jeambrun P, Belghiti J, Cortesse A,
infectious complications in noncolorectal abdominal surgery: a
Sossler C, et al. Nutrition and immunity after peritoneovenous
multivariate analysis based on a prospective multicenter study
drainage of intractable ascites in cirrhotic patients. Am J Surg
of 4718 patients. Arch Surg 2003;138:314—24.
[17] Guidelines for the surveillance of patients with uncomplicated
[38] Henrikson EC. Cirrhosis of the liver, with special reference to
cirrhosis and for the primary prevention of complications. Gas-
surgical aspects. Arch Surg 1936;32:413—51.
troenterol Clin Biol 2008; 32:898—905.
[39] Chapman CB, Snell AM, Rowntree LG. Decompensated portal
[18] Fernandez J, Navasa M, Gomez J, Colmenero J, Vila J, Arroyo V,
cirrhosis. JAMA 1931;97:237—44.
et al. Bacterial infections in cirrhosis: epidemiological changes
[40] Lemmer JH, Strodel WE, Knol JA, Eckhauser FE. Management
with invasive procedures and norfloxacin prophylaxis. Hepatol-
of spontaneous umbilical hernia disruption in the cirrhotic
patient. Ann Surg 1983;198:30—4.
[19] Yeh DC, Wu CC, Ho WM, Cheng SB, Lu IY, Liu TJ, et al. Bac-
[41] Belghiti J, Desgrandchamps F, Farges O, Fékété F. Hernior-
terial translocation after cirrhotic liver resection: a clinical
rhaphy and concomitant peritoneovenous shunting in cirrhotic
investigation of 181 patients. J Surg Res 2003;111:209—14.
patients with umbilical hernia. World J Surg 1990;14:242—6.
[20] Walz JM, Paterson CA, Seligowski JM, Heard SO. Surgical site
[42] Fagan SP, Awad SS, Berger DH. Management of complicated
infection following bowel surgery: a retrospective analysis of
umbilical hernias in patients with end-stage liver disease and
1446 patients. Arch Surg 2006;141:1014—8.
refractory ascites. Surgery 2004;135:679—82.
Please cite this article in press as: Douard R, et al. Operative risks of digestive surgery in cirrhotic patients. GastroenterolClin Biol (2009), doi:
ARTICLE IN PRESS
R. Douard et al.
[43] Gillet M. Chirurgie de la paroi chez le cirrhotique. In: Belghiti
[64] Garrison RN, Cryer HM, Howard DA, Polk Jr HC. Clarification of
J, Gillet M, editors. La chirurgie digestive chez le cirrhotique.
risk factors for abdominal operations in patients with hepatic
Paris: Monographies de l'AFC; 1993, p. 53—60.
cirrhosis. Ann Surg 1984;199:648—55.
[44] Leonetti JP, Aranha GV, Wilkinson WA, Stanley M, Greenlee
[65] Lau WY, Leung KL, Kwong KH, Davey IC, Robertson C, Dawson
HB. Umbilical herniorrhaphy in cirrhotic patients. Arch Surg
JJ, et al. A randomized study comparing laparoscopic versus
open repair of perforated peptic ulcer using suture or suture-
[45] Hurst RD, Butler BN, Soybel DI, Wright HK. Management of groin
less technique. Ann Surg 1996;224:131—8.
hernias in patients with ascites. Ann Surg 1992;216:696—700.
[66] Siu WT, Leong HT, Law BKB, Chau CH, Li ACN, Fung KH, et al.
[46] Cobb WS, Heniford BT, Burns JM, Carbonell AM, Matthews BD,
Laparoscopic repair for perforated peptic ulcer: a randomised
Kercher KW. Cirrhosis is not a contraindication to laparoscopic
controlled trial. Ann Surg 2002;235:313—9.
surgery. Surg Endosc 2005;19:418—23.
[67] Takeda J, Hashimoto K, Tanaka T, Koufuji K, Kakegawa T.
[47] Castaing D, Houssin D, Lemoine J, Bismuth H. Surgical manage-
Review of operative indication and prognosis in gastric can-
ment of gallstones in cirrhotic patients. Am J Surg 1983;146:
cer with hepatic cirrhosis. Hepatogastroenterology 1992;39:
[48] Puggioni A, Wong LL. A metaanalysis of laparoscopic cholecys-
[68] Isozaki H, Okajima K, Ichinona T, Fujii K, Nomura E, Izumi N.
tectomy in patients with cirrhosis. J Am Coll Surg 2003;197:
Surgery for gastric cancer in patients with liver cirrhosis. Surg
[49] Gillet M. Chirurgie des voies biliaires chez le cirrhotique. In:
[69] Lazorthes f, Charlet JP, Buisson T, Ketata M. Chirurgie de
Belghiti J, Gillet M, editors. La chirurgie digestive chez le cir-
l'estomac chez le cirrhotique. In: Belghiti J, Gillet M, editors.
rhotique. Monographies de l'AFC; 1993, p. 91—100.
La chirurgie digestive chez le cirrhotique. Paris: Monographies
[50] Poggio JL, Rowland CM, Gores GJ, Nagorney DM, Donohue JH.
de l'AFC; 1993, p. 73—80.
A comparison of laparoscopic and open cholecystectomy in
[70] Tachibana M, Kotoh T, Kinugasa S, Dhar DK, Shibakita M, Ohno
patients with compensated cirrhosis and symptomatic gall-
S, et al. Esophageal cancer with cirrhosis of the liver: results
stone disease. Surgery 2000;127:405—11.
of esophagectomy in 18 consecutive patients. Ann Surg Oncol
[51] Yeh CN, Chen MF, Jan YY. Laparoscopic cholecystectomy in
226 cirrhotic patients: experience of a single center in Taiwan.
[71] Nagawa H, Kobori O, Muto T. Prediction of pulmonary
Surg Endosc 2002;16:1583—7.
complications after transthoracic oesophagectomy. Br J Surg
[52] Fernandes NF, Schwesinger WH, Hilsenbeck SG, Gross GWW, Bay
MK, Sirinek KR, et al. Laparoscopic cholecystectomy and cir-
[72] Stahl M, Stuschke M, Lehmann N, Meyer HJ, Waltz MK, Seeber S,
rhosis: a case-control study of outcomes. Liver Transpl 2000;6:
et al. Chemoradiation with and without surgery in patients with
locally advanced squamous cell carcinoma of the esophagus. J
[53] Schiff J, Misra M, Rendon G, Rothschild J, Schwaitzberg
Clin Oncol 2005;23:2310—7.
S. Laparoscopic cholecystectomy in cirrhotic patients. Surg
[73] Gervaz P, Pak-art R, Nivatvongs S, Wolff BG, Larson D, Ringel
S. Colorectal adenocarcinoma in cirrhotic patients. J Am coll
[54] Palanivelu C, Rajan PS, Jani K, Shetty AR, Sendhilkumar K,
Senthilnathan P, et al. Laparoscopic cholecystectomy in cir-
[74] Seymour K, Charnley RM. Evidence that metastasis is less com-
rhotic patients: the role of subtotal cholecystectomy and its
mon in cirrhotic than normal liver: a systematic review of
variants. J Am Coll Surg 2006;203:145—51.
post-mortem case-control studies. Br J Surg 1999;86:1237—43.
[55] Bloch RS, Allaben RD, Walt AJ. Cholecystectomy in patients
[75] Song E, Chen J, Ou Q, Su F. Rare occurrence of metastatic col-
with cirrhosis. A surgical challenge. Arch Surg 1985;120:
orectal cancers in livers with replicative hepatitis B infection.
Am J Surg 2001;181:529—33.
[56] Byrne MF, Suhocki P, Mitchell RM, Pappas TN, Stiffle HL, Jowell
[76] Barsky SH, Gopalakrishna R. High metalloproteinase inhibitor
PS, et al. Percutaneous cholecystostomy in patients with acute
content of human cirrhosis and its possible conference of
cholecystitis: experience of 45 patients at a US refrral center.
metastasis resistance. J Natl Cancer Inst 1988;80:102—8.
J Am Coll Surg 2003;197:206—11.
[77] Song E, Chen J, Ouyang N, Wang M, Exton MS, Heemann
[57] Sugiyama M, Atomi Y, Kuroda A, Muto T. Treatment of choledo-
U. Kupffer cells of cirrhotic rat livers sensitize colon can-
cholithiasis in patients with liver cirrhosis. Surgical treatment
cer cells to Fas-mediated apoptosis. Br J Cancer 2001;84:
or endoscopic sphincterotomy? Ann Surg 1993;218:68—73.
[58] Chijiiwa K, Kosaki N, Niato T, Kameoka N, Tanaka M. Treat-
[78] Gervaz P, Scholl B, Mainguene C, Poitry S, Gillet M, Wexner S.
ment of choice for choledocholithiasis in patients with acute
Angiogenesis of liver metastasis: role of sinusoidal endothelial
obstructive suppurative cholangitis and liver cirrhosis. Am J
cells. Dis Colon Rectum 2000;43:980—6.
[79] Utsunomiya T, Matsumata T. Metastatic carcinoma in the cir-
[59] Prat F, Tennebaum R, Pnsot P, Altman C, Pelletier G, Fritsch J,
rhotic liver. Am J Surg 1993;166:776.
et al. Endoscopic sphincterotomy in patients with liver cirrho-
[80] Wind P, Teixeira A, Parc R. Chirurgie colo-rectale chez le
sis. Gastrointest Endosc 1996;43:127—31.
cirrhotique. In: Belghiti J, Gillet M, editors. La chirurgie diges-
[60] Park Do H, Kim MH, Lee SK, Lee SS, Choi JS, Song MH, et
tive chez le cirrhotique. Paris: Monographies de l'AFC; 1993,
al. Endoscopic sphincterotomy vs endoscopic papillary balloon
diloation for cholodecholithiasis in patients with liver cirrhosis
[81] Conte JV, Arcomano TA, Naficy MA, Holt RW. Treatment of
and coagulopathy. Gastrointest Endosc 2004;60:180—5.
bleeding stomal varices. Report of a case and review of the
[61] Mariette D, Belghiti J. Chirurgie du pancréas et cirrhose. In:
literature. Dis Colon Rectum 1990;33:308—14.
Belghiti J, Gillet M, editors. La chirurgie digestive chez le cir-
[82] Conférence de consensus : complications de l'hypertension
rhotique. Monographies de l'AFC; 1993, p. 105—12.
portale chez l'adulte. Gastroenterol Clin Biol 2004;28:
[62] Rabinovitz M, Schade RR, Dindzans V, Van Thiel DH, Gavaler
JS. Prevalence of duodenal ulcer in cirrhotic males referred
[83] Azoulay D, Buabse F, Damiano I, Smail A, Ichai P, Dannaoui
for liver transplantation. Does the etiology of cirrhosis make a
M, et al. Neoadjuvant transjugular intrahepatic portosystemic
difference? Dig Dis Sci 1990;35:321—6.
shunt: a solution for extrahepatic abdominal operation in cir-
[63] Lehnert T, Herfarth C. Peptic ulcer surgery in patients with liver
rhotic patients with severe portal hypertension. J Am Coll Surg
cirrhosis. Ann Surg 1993;217:338—46.
Please cite this article in press as: Douard R, et al. Operative risks of digestive surgery in cirrhotic patients. GastroenterolClin Biol (2009),
Source: http://www.espoire.org/wp-content/uploads/2011/07/chirurgie-du-cirrhotique-GCB-2009.pdf
INTRODUZIONE (Mt. 13,1-3a) Le Parabole del Regno (Mt. 13) I 5 "discorsi" del vangelo di Matteo Le 7 Parabole del Regno Discorso della montagna (Mt. 5-7) Parabola del seminatore Discorso Missionario (Mt. 10) Parabola della zizzania Discorso delle parabole (Mt. 13) Parabola del chicco di senape
Top 10 Tips for Defending Mass Torts in New Jersey by James J. Ferrelli and Alyson B. Walker New Jersey is home to many mass torts—asbestos, hormone replacementtherapy (HRT), NuvaRing, Vioxx, Fosamax, Accutane, and Bextra/Celebrex—toname just a few. With plaintiffs filing numerous cases in the Garden State, it'seasy to fall into the mindset that New Jersey is for plaintiffs. But don't get caughtin that trap and become complacent, filing rote motions and litigating onautopilot. With the right strategy and tactics, New Jersey can be for defendantstoo. Here are our top 10 tips for defending mass torts in New Jersey: