Leading article
Professor C C de Silva Oration 2000 Multimodal treatment in the management of paediatric malignancies in Sri Lanka R S Jayatilake1 Sri Lanka Journal of Child Health, 2000; 29: 70-84 (Key words: paediatric malignancy, multimodal treatment, Sri Lanka) Introduction
The success brought about by the rational com-
Childhood cancers form a specific group of tumours
bination of the three important therapeutic mo-
which differ markedly in clinical behaviour, histology
dalities - surgery, radiotherapy and chemotherapy.
and sites of origin. In the last decade, childhood
mortality from infections and congenital diseases has
The dawn of multi-disciplinary team approach.
been so greatly reduced that cancers, albeit rare, are the
second principal cause of death. Only accidents cause
The growth of specialized centres of management
more deaths in children less than 12 years of age in Sri
for children with cancer i.e. Institutions expecting
Lanka. Childhood cancers make up 2% of all cancers in
to provide state of the art care for children with
Sri Lanka. 50% of them are haematological. The
cancer. They have teams consisting of experts as
epithelial tumours of adult life are rare in children and
well as coordinated programmes for total
the spectrum of malignancies in childhood is not varied
as seen in adult population. The common types of
tumours of childhood, number less than a dozen.
The use of rational study protocol.
History records some solid tumours undergoing
All of the above factors have become norms of
spontaneous remission. Neuroblastoma, hepatoblastoma,
management. The state of the art care is well seen in the
and sacrococcygeal tumours are some of them.
USA. 75% of children with cancer are treated according
Nasopharyngeal carcinoma, hepatocellular carcinoma,
to a national study protocol. Although cure is being
and Ewings Sarcoma are tumours children share with
achieved in an increasing number of children, the late
adults. Genetic factors account for several childhood
effects from these treatments have been identified in a
tumours. Few are associated with chromosomal
significant number of survivors. As this population of
abnormalities. Such modes of genetic oncogenesis
children and young adults continue to increase, the need
appear to occur in patients with retinoblastoma, Wilms
for health professionals, both specialist and primary care
tumour, osteogenic sarcoma, hepatoblastoma and
practitioners to monitor and treat long term survivors,
rhabdomyosarcoma.
has greatly increased.
Some genetic disorders are associated with increased
Aims of the study
incidence of cancer, e.g. Trisomy 21 has increased
incidence of acute lymphoblastic leukaemia. With the
This study spans from 1975 to 1999. From 1980 to 1995
use of combined modalities of treatment, such as
data of all patients visiting the Institute was correctly
recorded; this number included 1959 cases. The purpose
chemotherapy over 65% of children with cancer will be
of this study was to:
cured of their disease. This means that by the year 2000
an estimated one out of 900 young adults will be
Present the data available from the National Cancer
survivors of childhood cancer1. There has been
Institute, Maharagama, Paediatric Oncology Unit,
tremendous advances during the last two decades in the
in relation to types of malignancy, age at
management of paediatric cancers. This has resulted
presentation, the frequency and the ethnic dis-
Successive clinical trials of new treatment strate-
Study the results of treatment and cure and com-
gies, based upon the best treatment known at that
pare them with international results.
Record complications and late effects due to treat-
Consultant Oncologist
Material and methods
1959 cases have been entered into this study and all of
Paediatric malignancies in Sri Lanka:
them have undergone standard investigation and
Distribution of solid tumours (RSJ/1999)
treatment according to international protocols. Certain
special investigations such as CT scans MRI scans,
routine bone scans and tumour markers were not done
as these facilities were not available. Pathology reports
Soft tissue sarcoma
which were sent from district and provincial hospitals
were all reviewed by the Cancer Institute Pathologist for
examinations were repeated and verified. Acute
Lymphoblastic Leukaemia (ALL) was distinguished
from Non-Hodgkin's Lymphoma (NHL) on the
percentage of blasts at the time of diagnosis using
Murphy's classification2. More than or equal to 25%
blasts indicated ALL and less than 25% NHL. Main
disease groups were defined using an altered ICDO
French-American-British (FAB) classification was used
classification scheme as it is commonly used in pae-
to sub type the acute leukaemias. Table 4 shows the sub
diatric cancer3.
types in ALL. 304 (40.9%) were grouped as
Unclassified. L1 accounted for 39% and L2 18.2%.
In Sri Lanka the upper limit of the paediatric age is 12
87.9% of ALL were Sinhalese and Muslims showed a
years, Hence in this series the age group is classified as
higher incidence even though the Tamil population was
below 1 year, 1 to 4 years, 5 to 8 years and 9 to 12
higher. The war in the North may have contributed to
years. There were 1156 (59%) male and 803 (41%)
female children. 86.8% were Sinhalese, 6.6% Tamil and
6.7% Muslims. 34.4% and 33.6% of the cases were in
the 1 to 4 and 5 to 8 year age groups. Except for the
Sub types of acute lymphoblastic leukaemia
below 1 year group others had a male preponderance.
1075 cases (54.9%) were haematological malignancies
and 884 (44.1%) were solid tumours and accounted for 38%. NHL was second with 5.6% (Tables 1, 2 and 3).
Brain tumours and retinoblastomas accounted for 11.1%
and 6.7% respectively. 113 (5.7%) were classed as
'Others'. This group was separated into 'Frequent' and
'Infrequent' types. Ovarian cancers stood out at 2.3%.
Epithelial cancers were rare and less than 1%.
Table 5 shows the age distribution in ALL. 42.7% was
in the 1 to 4 age group with a median age of 4.9 years.
50% of acute myeloblastic leukaemias (AML) were
Paediatric malignancies in Sri Lanka:
unclassified and 30.1% were M4. 42.4% were in the 9 to
Distribution of malignancies (RSJ/1999)
12 age group, with a median age of 7.6 years. The
presenting age between ALL and AML showed a
distinct difference. Once again the Muslim community
had a higher representation - 11.3%.
Paediatric malignancies in Sri Lanka:
Age distribution in acute lymphoblastic leukaemia
Distribution of haematological malignancies
All the cases of Non-Hodgkin's Lymphomas (NHL)
were of the diffuse type with 95.5% having bone
marrow involvement (Table 6). Age distribution of
NHL is shown in Table 7. The median age was 7years.
83.4% of STS were distributed in the 1 to 8 age group.
Tamils showed a higher incidence than Muslims.
Neuroblastomas were unique in that 63.6% were in the
abdominal cavity and in 29.8% the site was unknown.
The age distribution was remarkable in that 54.5% were
Types of Non Hodgkins Lymphoma (NHL)
below the age of 4 years.
Except for a solitary case of chondrosarcoma, the rest of
the bone tumours were in two groups, Ewing sarcoma
56% and osteogenic sarcoma 43%. 60% of Ewing
sarcomas were in long bones, and affected the upper
third of the shaft of long bones and rarely showed the
Bone marrow infiltration
'onion peel' appearance radiologically. Flat bones were
affected in 30% and ileum was the common site. In
osteogenic sarcomas femur was the disease site in
NHL – Age distribution (RSJ/1995)
87.5%. Both Ewing and osteogenic sarcomas were seen
in the second half of childhood.
There were 40 cases Langerhan cell histiocytosis;
however the sub types affected different age groups
(Tables 8-11). Letterrer-Siwe disease was the least
common type, where 75% of them were seen in less
than one-year age group (Table 9). 90% of Hand-
Schuller-Christian Syndrome and 100% of eosinophilic
Classically Hodgkin's Lymphomas (HL) are grouped
granuloma were found in the second half of childhood
into four sub types. However, 25.9% were grouped as
(Tables 7 and 8). In the unclassified type 66.6% were in
unclassified due to the poor status of the slides on
the 5 to 8 year age group (Table 9).
reassessment. Mixed cellular sub type was the
commonest (25.9%). 91.3% of HL were in the latter
half of childhood. 16% of HL were Tamils with
Paediatric malignancies in Sri Lanka:
Muslims having 9%.
Langerhan-Cell-Histiocytosis (RSJ/1995)
On presentation, brain tumours were categorised into
Letterer-Siwe-Disease
subtentorial 72.5% (158) and supratentorial 27.5% (60)
Hand-Schuller-Christian
types. In the subtentorial group there were three main
types, medulloblastomas 22.5% (49), brain stem glioma
Eosinophilic granuloma
34.4% (75) and posterior fossa astrocytoma 15.6% (34).
Nearly 80% of the brain tumours were in the 5 to 12 year age group. Unique feature in the posterior fossa
tumours was that it spared the below one year age
childhood solid tumour, made up 6.7% and 80% were
Letterrer-Siwe-Disease - Age distribution
unilateral at the time of presentation. Both eyes were
equally affected. Unlike brain tumours 81% of
retinoblastomas were below 4 years of age. All bilateral
tumours were below 4 years of age, suggesting genetic
origin. Retinoblastomas occurring above 5 years were
unilateral and may have occurred due to spontaneous
mutations. All unilateral and some bilateral tumours had
enucleation done at the time of referral.
Hand-Schuller-Christian-Syndrome
98% of nephroblastomas (Wilms tumours) were
Age distribution
unilateral; equal representation was observed from both
sides. 80.5% were below the age of 4 years.
Histologically, Wilms tumours occurring after the age of
5 years had more of epithelial component. There were
two main types of soft tissue sarcomas (STS) - 44.5%
were rhabdomyosarcoms and 55.5% were other types.
38.7% of rhabdomyosarcomas originated in the head
and neck region, which was the highest individual site.
free survival. Cases lost for follow up has been indicated
Eosinophilic Granuloma - Age distribution
as 'lost'. 5 year disease free survival figures has not been
given for Period 3. Patients lost ranged from 8 to 23 %
in the haematological malignancies and less than 10%
for solid tumours.
Remission rates (CR) in haematological malignancies
CR rates for ALL during the three periods are shown in
Table 12. Even though the total number of patients
differed in the first period, CR rate was low (55.5%),
The results of paediatric malignancies have been
compared to 76% in the second period and 80% in the
categorized in to three periods ie.1980 to 1985 - Period
third period. The protocols adopted were different A
1; 1986 to 1990 - Period 2; 1991 to 1995 - Period 3.
similar trend was seen with AML, 37.5% in period 1
This has been done according to the facilities and man
and 57.1% and 60% in period 2 and period 3
power available. During Period 1 there was no
respectively (Table 13). The management protocols
Oncology training programme and facilities were mini-
were different. CR rate for NHL in period 1 was half
mal. Period 2 saw the dawn of Oncological training
that seen period 2 and period 3 (Table 12). CR rate was
programme. Period 3 was blessed with trained Oncolo-
40% vs 81.3% vs 79.2%. 'COP' schedule was used in
gist, Oncology nursing staff and the availability of first
period 1 and 'CHOP' schedule in the other two periods.
CT scanner in the private sector and at the National
The CR rates in Hodgkin's Disease were 42.8%, 69.4%
Hospital, Colombo. National Cancer Institute had the
and 78.8% in the three periods respectively. All the
establishment of the Blood Bank and facilities to obtain
cases had chemotherapy irrespective of the stage.
blood components. The protocols adopted for various
Customarily stage 1, Stage 11 A in adults had involved
conditions underwent change according to the
nodal irradiation. 'MOPP' schedule was the standard
availability of resources. Results have been compiled as
chemotherapy protocol used during period 1. However
Complete Remission (CR), 3 year and 5 year disease
this was changed to alternating 'MOPP' with 'ABVD'.
. Table 12 Remission rate and survival figures in ALL
Table 13 Remission rate and survival figures in AML
Three and five year survival figures
same CNS prophylaxis and maintenance schedule - 5. In
AML routine CNS prophylaxis was not given.
In ALL and NHL remission induction was followed by
Maintenance therapy was given for one year in period 1
consolidation, CNS prophylaxis and maintenance
and for two years in periods 2 and 3. Management of
therapy for three years. Hodgkin's Lymphoma had only
solid tumours involved utilization of all three modalities
remission induction therapy. ALL and NHL had the
of treatment. Except for brain tumours all others had
chemotherapy up-front. Chemotherapy was used for two
9.3% survived 5 years. In period 3 children lost for
years. Termination of chemotherapy was dependant on
follow up was the same for ALL and AML (Table 13).
the status of bone marrow.
NHL showed a definite difference in 3 year survival
from period 1 to period 3, with different induction
ALL, the commonest malignancy in children, had
schedules 33% to 79% with 22 to 23% lost for follow up
improvement of three-year survival from period 1 to 3,
(Table 14). In Hodgkin's Lymphoma the 3 year and 5
the recorded figures being 27.7% to 39.8% to 51.8%.
year survival was the same 28% and 55.5%. This is an
Once uncomplicated survival was completed by three
indication that if HL children survived 3 years disease
years, they had greater than 90% chance of surviving 5
free, then they had the same chance of surviving 5 years.
years. Lost for follow up during period 1 was up to 22%
On this assumption 73.6% successfully treated HL
(Table 12). There were no survivors in AML in period 1
children will survive 5 years irrespective of the stage
and no significant three-year survival difference
between the periods 2 and 3 (23.2% vs. 26.6%). Only Table 14 Remission rate and survival figures in NHL
Table 15 Remission rate and survival figures in HL
In brain tumours, chemotherapy schedules were
tumours. They had surgery followed by radiation
different in period 1 and period 2. Medulloblastoma
therapy and had an overall three year survival figure of
showed a significant difference in three year survival
rates in the three periods from 40% to 46.6% to 58.2%
(Table 16). Brain-Stem-Gliomas (BSG) during period 3
was diagnosed on CT scans and none had surgery; all
Survival figures in brain tumours –
had chemotherapy followed by radiation therapy. In
medulloblastomas
periods 1 and 2, diagnosis was made on radiology,
worsening clinical signs and on patients who did not
respond to anti TB drugs. They were unfit to have any
chemotherapy and only radiation therapy. None sur-
vived 3 years in period 1 and 10% (2/20) survived 3
years in period 2. There were no 5 year survivors. Period 3 had 26.6% (12/45) surviving 3 years which is
more than double that seen in period 2 (Table 17).
Posterior fossa astrocytoma had the best survival figures
for brain tumours. 60% three-year survival was seen in
periods 2 and 3 and 30% survived 5 years in period 2
(Table 18). Supra tentorial tumours ranged from
craniopharyngiomas to gliomas and choroid plexus
unilateral tumours had routine enucleation and bilateral
Survival figures in brain tumours – BSG
tumours had enucleation of the worst affected eye. In
period 1 all had oral cyclophosphamide with or without
radiation therapy. Due to the alarming survival figures
in period 1, treatment protocol was changed. With the
change of protocol 5 year survival rose from 17% in
period 1 to 54.9% in period 2. Three-year survival in
period 3 was 69.5% (Table 20). Survival figures in
Wilms tumours is shown in Table 21. Changes in
Survival figures in brain tumours –posterior fossa
survival rates are due to changed management protocol.
In period 1 patients had six weekly Actinomycin D for
one year postoperatively. In periods 2 and 3, children had Actinomycin D during surgery and postoperatively
in combination with doxorubicin for a year.
Radiotherapy was given in indicated cases only. Five-
year survival changed from 52.3% to 65.5% from period
1 to 2. Three-year survival rate of 78.5% was seen in
period 3. Cases lost for Wilms tumour was less than 4%.
In Wilms tumour there was one case with aniridia and
one with hemihypertrophy of the body; both cases died
Survival figures in supra tentorial brain
within one year. In soft tissue sarcoma, the 110 cases
recorded are confined to periods 2 and 3. Abdominal
rhabdomyosarcomas did poorly as all of them were
referred after inadequate surgery and most patients were
not fit to have chemotherapy. There were no 5 year
survivals and the three year survival was confined to
rhabdomyosarcomas did better with the combined
modality of treatment with three year and five year
survival figures of 39% and 26% respectively. Other
Treatment of retinoblastoma was a success story when
soft tissue sarcomas had survival figures of 36% and
figures are compared in the different periods. All
24.5% at three and five years respectively.
Table 20 Survival figures in retinoblastoma
Table 21 Survival figures in Wilms tumour
In Neuroblastoma, too, the management protocol
management's of bone tumours in period 1 was dismal,
differed in the three periods. In periods 1 and 2 the five
basically due to inability to give high dose methotrexate
year survival was almost half the figure seen in the three
with folinic acid rescue in osteogenic sarcoma. Schedule
year period, showing that almost 50% developed
variation was seen in periods 2 and 3 with change in
recurrent disease once being in remission and clinically
disease free at three years (Table 22). Results of
Table 22 Survival figures in neuroblastoma
Three-year survival of 44.4% and 43.3% was seen
100% survival (Table 23). In frequent paediatric
Ewing sarcoma and osteogenic sarcoma respectively. In
malignancies gonadal tumours had the best survival
Langerhan cell histiocytosis 72.9% overall three-year
figure, 62.5% three-year survival, nasopharyngeal carci-
survival was seen with eosinophilic granuloma having
noma having 54.5%.
Table 23 Survival figures in Langerhan-cell histiocytosis
Letterer-Siwe-Disease
Hand-Schuller-Christian Syndrome
Eosinophilic granuloma
same reason the aggressiveness of the induction
schedules used in the treatment. Hence our CR rate
Childhood cancers are rare, but with modern treatment a
being 80% and a cure of 37.5% in period 2 and three
high cure rate can be expected. The same cannot be said
year survival of 51.8% in period 3. Apart from bone
for adult cancers. This has been possible because a team
marrow relapse, recurrent CNS disease was the major
approach that incorporate the skills of the paediatrician,
complication that was encountered. In a follow up of
paediatric surgeon, radiation oncologist, paediatric
593 cases of ALL 40 (6.7%) had recurrent CNS disease.
Majority was in ALL (L3-25%). Table 24 shows the
specialist and social workers are imperative to ensure
different types of CNS disease. Meningeal leukaemia
that patients receive treatment, supportive care and
accounted for 80%. Tables 25 and 26 shows the survival
rehabilitation in order to ensure optimal survival and
after recurrent CNS disease and the survival of sub
quality of life. This type of 'state of the art' treatment
types. Only 25 % survived over one year. The survival
should be given at specialized centres, using protocols
figures for AML were dismal - 9.3% 5 year survival in
that have been tried out and proved effective.
period 2 and 26.6% three year survival in period 3.
United Kingdom national statistics show survival in
Approximately 70% of children with ALL are cured
AML has improved from 8% at 4 to 5 years during
with current protocol-based treatments, while 95% of
1974-1976 to 25% from 1983-19855. With more
the patients can be expected to attain complete re-
aggressive chemotherapy recent disease free survival
mission4. Cure is correlated to a number of prognostic
has risen to 30 to 40%6. Majority of them need bone
variables. These include clinical parameters and bio-
marrow transplants if we are to achieve a high cure rate.
logic variables. With the limited resources available we
Rate of cure after transplant is 60 to 70%7.
have been able outline the clinical variables. For the
Incidence of sub-types of recurrent CNS disease
Survival figures in recurrent CNS disease
Meningeal leukaemia
Hypothalamic syndrome
Localized CNS disease
Table 26 Survival of sub types of R-CNS disease after treatment
Meningeal leukaemia
Hypothalamic syndrome
Localized disease
We have had excellent survival figures for NHL i.e. a
fold; to cure the disease and to preserve as much vision
cure rate of 69%, with most studies reporting over 60%
as possible. In this series cases referred were after
cure rate8. A possible reason may be the use of 'CHOP'
enucleation and 3 year survival increased from 28.5% to
69.5% basically because all had intrathecal methotrexate
maintenance therapy for three years, as we now know
with combination chemotherapy. CNS seeding was the
that 'CHOP' is the best schedule for NHL. More than
primary site of disease recurrence and with the new
75% of newly diagnosed HL in children are cured with
approach of treatment CNS seeding was overcome.
modern radiation therapy and/or combination therapy9.
Patients with retinoblastoma, particularly the hereditary
Our results show 55.5% 5 year survival in period 2 and
type, have an increased frequency of second
73.6% three year survival in period 3, using
malignancies, most often bone tumours, occurring in up
combination chemotherapy alone. Use of combination
to 8% after 18 years of follow-up12. Wilms tumour is a
chemotherapy judiciously has spared muscle atrophy
curable condition in the majority of affected children.
that can occur with the use of radiation therapy.
Greater than 90% of patients survive 4 years after
diagnosis13. Our series recorded 78.5% three-year
Primary brain tumours are a widely varying group of
disease free survival in all cases pooled together. The
diseases and form the most common solid tumours in
major drawback in this series was the absence of data on
children. The clinical distribution of these tumours does
the subtypes and operative findings and inability to
not vary globally and more than 50% of children
recover the original slides of second opinion.
diagnosed with brain tumours will survive 5 years from
Pathologist's reluctance to release slides for second
diagnosis10. For a good many of childhood brain
opinion remained an obstacle in obtaining good
tumours, the optimal treatment regimen has not been
histological reports. This was true for all solid tumours.
determined. In this series for medulloblastomas and
Paediatric surgeons other than at Lady Ridgeway
BSG the chemotherapy schedule was changed from
Children's Hospital carried out surgery without
vincristine + procarbazine + methyl CCNU to 8-drugs-
consultation with the Oncologists and patients never had
in-one-day-regime ("8 in 1") and immediate survival
advantage was seen. In medulloblastoma from 40%
management was according to international protocol;
three year survival in period 1 to 58.2% in period 3. In
hence the lower survival figure is because of inadequate
BSG no survival in period 1 to 26.6% three year
staging and proper subtyping.
survival in period 3. BSG is classified according to
location, extent of spread and histology. BSG may occur
Nearly 70% of neuroblastoma patients have metastatic
in pons, mid brain, the tectum, the cervico-medullary
disease at diagnosis14 and it is of paramount importance
junction, or the dorsum as exophytic growths. However,
to identify them and to see the extent of disease prior to
majority are in the pons and are diffuse and intrinsic.
treatment. It is also necessary to perform catecholamine
One third spread by the CSF channel. The less common
assays in urine prior to and during management. MIBG
tumours of mid brain, especially in the tectal plates,
scan facilities were not available in Sri Lanka and
have slow growth and long term survival. There is
catecholamine assays took nearly a month, which would
approximately 80% five year progression free survival
mean that the disease will become far too advanced if
vs. 20% for tumours in pons and medulla11. All the BSG
this test was done on a routine basis. In spite of this, by
were treated without a biopsy; however biopsy may be
adopting a established protocol it was possible to cure
indicated for BSG that are not diffuse and intrinsic,
one third of the patients during period 2 and to a 68.7%
when the tumour is progressive or when surgical
three year survival in period 3. According to children
debulking is possible. New approaches with stereotactic
cancer group (CCG) staging system, stages I, II, III,
needle biopsy may make biopsy safer. These facilities
(unresected negative nodes) the probability of long term
were not available in Sri Lanka during this study.
survival is 75 to 90% depending on the age and for stage
IV 50% to 70%15,16.
Majority of patients with retinoblastoma have extensive
disease within the eye at diagnosis with either massive
90% of patients with apparently localized Ewing
tumour involving more than one half of retina, multiple
sarcoma have occult metastatic disease17 and survival is
tumours diffusely involving the retina, or obvious
poor if an aggressive treatment approach is not adopted.
seeding of the vitreous. The goals of therapy are two
This is quite evidently seen in our series. There were no
survivors in period 1. In periods 2 and 3 survival rates
Our experience with limited number of nasopharyngeal
improved and in period 3 the philosophy of radical
cancer is that they remained local and loco-regional.
surgery for "expendable bones" (like the fibula) was
Systemic spread was not seen and 54.5% survived 3
adopted. This reduced the tumour burden and better
years. Yolk sac tumours were extensive (Stage III/IV)
results were seen with chemotherapy. Hence, three-year
survival figure of 44.4% in period 3. Soft tissue
uncontrollable with chemotherapy. Different results
sarcomas (STS) consists of a malignant tumour
presumably originating in the primitive mesenchymal
Dysgerminomas gave good results with radiation
tissue and exhibiting no rhabdomyoblastic differen-
therapy. No chemotherapy was used in the treatment of
tiation formed a definite entity when compared to
rhabdomyosarcoma. Abdominal rhabdomyosarcomas
did poorly as almost all the tumours were inadequately
Langerhan-cell-histiocytosis gave mixed results. As
debulked, resulting in a large tumour burden. There
classically stated, eosinophilic granuloma was treated
were no 5 year survival in this group. CNS extension
with surgical 'scooping' followed by low dose radiation
has been reported as a complication in head and neck
therapy which gave 100% survival. Low dose radiation
rhabdomyosarcomas, none were seen in this series;
therapy had a definite place in the management of
however their presentation is late. 26% five year sur-
'punched out' areas in bone with 100% local control.
vival was seen in this group. It is reported to be more
than 60% in those children who receive optimal treat-
Although cure is being achieved for a sizeable number
ment18. Our results are way below the best figures given,
of children with multimodal therapy, late effects from
in view of the late presentation and lack team
these treatment have been identified in a significant
number of long term survivors. Children withstand all
forms of treatment remarkably well; however the late
Osteogenic sarcoma was one other tumour that had
effects will manifest when the child matures. Hence,
dismal survival figures in our series - 43.3% three year
observation of late effects has been documented in this
survival in period 3. Patients who survived were those
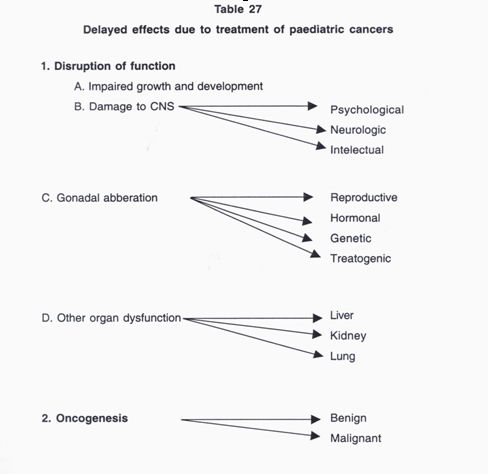
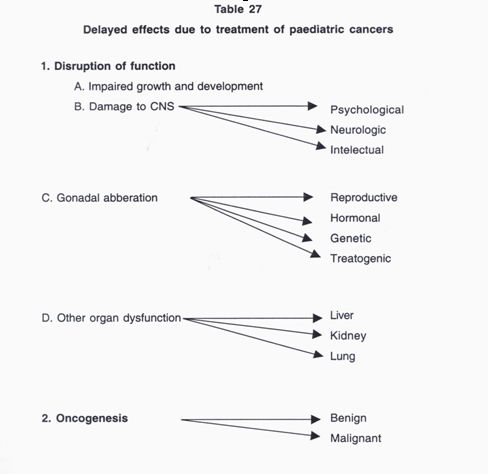
series 5 years after being pronounced cured. Table 27
consented to amputation/disarticulation as these cases
outlines the possible delayed effects.
had extensive tumours. Presentation was late because all were treated by Ayurvedic practitioners.
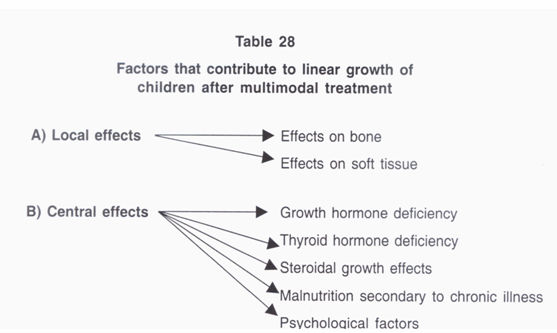
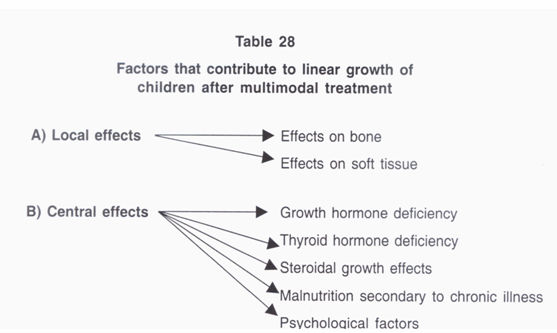
Linear growth is an important aspect in the growth and
normal counterparts19. It has been suggested that lower
development of a child; two factors contribute to this
height in ALL children was present at diagnosis20 or
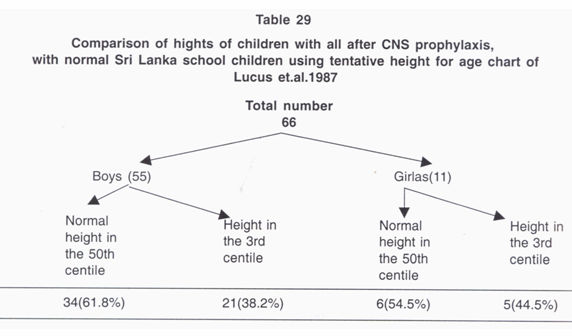
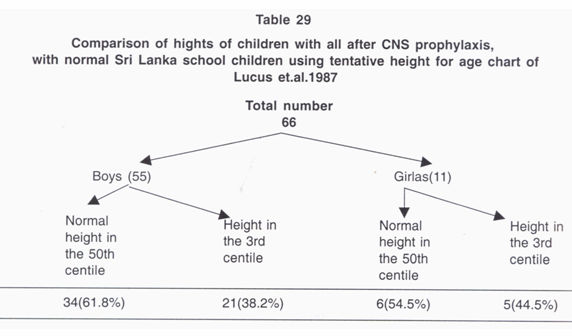
(Table 28). Sixty six children cured of ALL have been
consequence of disease. This is consistent with a recent
compared with normal children using Sri Lankan
study documenting an abnormality in endocrine function
height/weight chart18a (Table 29). 21 (38.2%) boys and 5
as a manifestation of ALL21. Cranial irradiation of doses
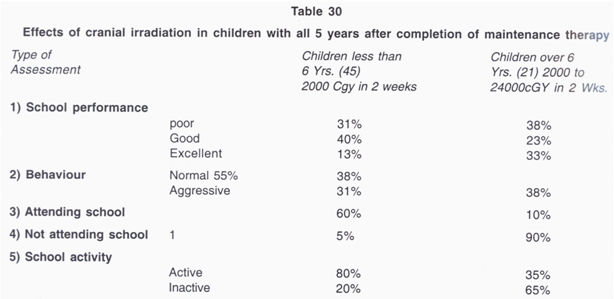
(44.5%) girls had growth retardation possibly due to
2400cGy to children less than 10 years shows an IQ of
effects of cranial irradiation. Pituitary hormone studies
85 to 99 - a drop of 10 to 11 points22. A proportion of
were not done due lack of facilities. Neuropsychological
ALL children in this series above 6 years who had this
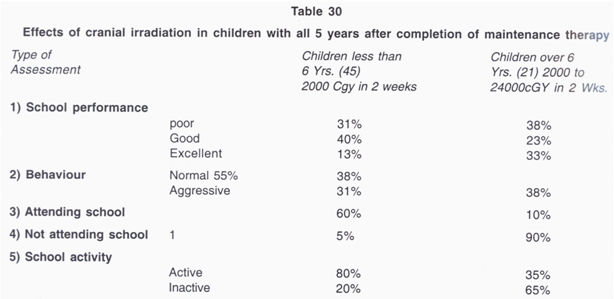
effects have been studied in children who have had
dose of radiation showed inability to compete and was
cranial prophylaxis and interesting results have been
inactive at school. A comparison of cranial irradiation
observed (Table 30). A significant proportion of
doses of 1800cGy versus 2400cGy has shown normal
children over 6 years of age (90%) did not attend
growth rate and IQ with 1800cGy and not with the
school, the primary cause being that they were not able
latter23. Higher doses of radiation to the brain show
to compete with the normal children and 65% of
significant neurological and mental disturbances24. 20 to
children in this group were not active in school. It is
30% of medulloblastomas receiving higher dose of
possible that this is a direct effect of the radiation
radiation showed CNS disturbances with up to 50% of
therapy given. Recent investigations have revealed that
them needing special educational institutions25.
children treated for ALL were significantly smaller than
In this series all cases of HL had chemotherapy and
Acute myelomonocytic leukaemia (AMML) and
no endocrine dysfunction was seen. 44% of HL and
supratentorial gliomas made up 27.2% each. Char-
17% of NHL had elevated levels of TSH when
acteristically the gliomas were all supratentorial
treated with radiation therapy to the neck with mean
which is not in keeping with classical presentation of
interval of occurrence of 18 to 31 months26.
brain tumours in children. Table 33 shows the
distribution of the second malignancies.
The cumulative risk of developing a second malig-
nant neoplasm following radiation therapy in long
term survivors of childhood cancer has been
Incidence of second malignancy after 7 years of
estimated as high as 10% by 10 years following
disease free follow up
initial treatment and 17% by 20 years27,28. The annual
Total number of cases evaluated
risk of developing second malignancy during or after
Number of cases surviving 5 years
treatment for ALL is 62.5 per 100.00029.
Number of second malignancies
malignancy. In many instances it is difficult to
Types of second malignancy
chemotherapy is given before during or after
radiation therapy. Both modalities may affect DNA-
Acute myelomonocytic leukaemia
RNA moieties and nucleic acid metabolism. Both
these modalities are also immunosuppressive.
Table 31 shows 1268 cases in this series evaluated, of
Acute undifferent leukaemia (AUL)
which 528 (41.6%) cases survived beyond 5 years
and 11(2%) had a second malignancy. The types of
Follicular carcinoma of thyroid
second malignancies are shown in Table 32.
Table 33 Distribution of second malignancies
Children who were treated for HL and retinoblastoma
malignancy following treatment for HL in children
had the highest number of second malignancies viz.
and adolescents is 18.7% at 15 years after diagnosis,
36.3% (4/11). The cumulative risk of second
with predominance of bone sarcoma30. In our series,
one out of 4 cases were bone sarcomas;Three out of 4
8. Magrath I. Malignant Non Hodgkin's Lymphoma in
were acute leukaemias. One case of follicular
children In; Pizzo PA, Poplack DG: Principles and
carcinoma was seen in a patient with a
practice of Paediatric Oncology. Philadelphia
retinoblastoma, who had chemotherapy. It has been
JB.Lippincott, 2nd.ed, 1993; pp 537-5.
estimated that 20 to 30% of individuals exposed to
external thyroid irradiation had developed single or
9. Levanthal B G, Donaldson S S, Pizzo P A, Poplack
multiple thyroid nodules; approximately 30% of them
D G. Principle and Practice of Paediatric Oncology.
are malignant-follicular or mixed types rarely
Philadelphia JB. Lippincott, 2nd ed. 1993 pp 577-94.
anaplastic. A single case in our series had a bone
sarcoma and this was in a case of retinoblastoma.
10. Cohen M E, Duffman P K, editors. Brain tumours
Retinoblastomas are known to get bone sarcomas. All
in children. Principles of Diagnosis and treatment.
our cases of second malignancies had a fatal outcome
2nd. ed. New York: Raven Press 1994.
within a year in spite of active treatment.
11. Halperin E C, et al. Selection of a management
strategy for paediatric Brain Stem Gliomas.
Medical and Paediatric Oncology 1989; 17(2):
I wish to thank all my Registrars from 1980 to 1999.
It is too long a list to name them separately.
12. Gallie B L, Dunn J M, Chan H S, et al: The
genetics of Retinoblastoma, relevance to the
patient. Paediatric Clinics of North America 1991;
1. Meadows A T, Krejmas N L, Belasco J B. The
medical cost of cure. Sequelae in survivors of
childhood cancer, in Van Eys J, Sullivan M P
13. National Wilms tumour study committee: Wilms
(editors): Status of the curability of childhood
tumour status report. Journal of Clinical Oncology
cancers. New York City, Raven Press, 1980; pp
1991; 9(5): 877-87.
14. Adams G A, Schuchat S J, Smith E I, et al.
2. Murphy S B, Hustu H O. A randomized trial of
Thoracic neuroblastoma; a Paediatric oncology
combined modality Therapy of childhood Non-
group study. Journal of Paediatric Surgery 1993;
Hodgkin's Lymphoma Cancer 1980; 45:630-7.
3. Birch J M, Marsden H B. A classification scheme
15. Hayes F A, Grece A, Hustu H O, et al.
for childhood cancer. Int. J. Cancer 1987; 40: 620-
Surgicopathological staging of Neuroblastoma;
prognostic significance of regional node metastasis.
Journal of Paediatrics 1983; 102(1): 59-62.
4. Pui C H, Grist W M. Biology and treatment of
acute lymphoblastic Leukaemia. Journal of
16. West D L, Shamberger R C, Maklin R M, et al.
Paediatrics 1994; 124(4): 491-503.
Stage III neuroblastoma over one year age at
diagnosis. Improved survival with intensive
5. Stiller C A, Bunch K J. Trends in childhood cancer
multimodal therapy including multiple alkylating
survival in Britain 1971-1985. B J of Cancer 1990;
agents. Journal of Clinical Oncology 1993; 11(1):
6. Buckely J D, et al. Remission induction in children
17. Evans R G, Nesbit M E, Gehan E A, et al.
with Acute Non Lymphoblastic Leukaemia using
Multimodal therapy for the Management of
localized Ewing's sarcoma of pelvic and sacral
daunorubicin: a report from children cancer study
bones: a Report from the second inter group study.
group. Medicine and Paediat Oncology, 1989;
Journal of Clinical Oncology 1991; 9(7): 1173-80.
18. Crest W, Gehan E A, Ragab A L, et al. The third
7. Sanders J F, Thomas E D, Buckner C D. Marrow
inter group Rhabdomyosarcoma study. Journal of
transplant for children. In first remission of Acute
Clinical Oncology 1995; 13(3): 610-30.
Non Lymphoblastic Leukaemia, an update. Blood
18a. Lucas G N, Samarasuria K, Perera W. Tentative
height for age and weight for age charts for Sri
Lankan school children. Ceylon Journal of Child Health 1987; 16(1): 33-46.
19. Berry D H, et al. Growth in children with ALL: A
25. Danoff B F, et al. Assessment of long term effects
paediatric oncology Group study. Medical and
of primary radiation therapy for brain tumours in
Paediatric Oncology 1983; 11:39.
children. Cancer 1982; 49:1580.
20. Robinson C C, et al. Heights of children
26. Glatstein E, et al. Alteration in TSH and thyroid
successfully treated for ALL. A report from late
function following radiotherapy. J Cli Endcrinol
effects study committee of children cancer study
Metab 1971; 32: 833.
Group. Medical and Paediatric Oncology1985;
27. Meadows A T. Pattern of second malignant
neoplasm in children. Cancer l 977; 40:1903.
21. Perrone, et al. Endocrine function in childhood
acute lymphoblastic Leukaemia before and during
28. Li F P, Cassidy J R, Jaffe N: Risk of second tumour
therapy. Am. J. Paed. and Haemat 1988; 10(2):
in survivors of Childhood cancer. Cancer 1975;
22. Meadows A T, et al. Decline in IQ scores and
29. Mik V, Meadows A T, d'Angio G D. Incidence of
cognitive dysfunction in children with acute
second malignant Neoplasm in children. Results of
lymphoblastic leukaemia treated with cranial
an international study. Lancet 1982; 2:1326.
irradiation. Lancet 1981; 2:1015.
30. Kushne B H, Zuber A, Tan C T C. Second
23. Cocognani A, et al. Different of 18Gy and 24Gy
malignancy after childhood Hodgkin's Lymphoma.
cranial irradiation growth rate and growth hormone
Cancer l988; 62:1364.
release in children with prolonged Syrvivd after
acute lymphoblastic leukaemia. Amer J Dis Child
24. Bloom G J G, Wallace E N K, Henk J M. The
treatment and prognosis of medulloblastoma in
children - a study of 82 verified cases. AJR 1969;
Source: http://dailynation.lk/wp-content/uploads/2015/02/Sri-Lanka-study1.pdf
Weak 50-mRNA Secondary Structures in Short EukaryoticGenes Yang Ding, Premal Shah, and Joshua B. Plotkin* Department of Biology, University of Pennsylvania *Corresponding author: E-mail: [email protected]. Accepted: September 21, 2012 Experimental studies of translation have found that short genes tend to exhibit greater densities of ribosomes than long genes ineukaryotic species. It remains an open question whether the elevated ribosome density on short genes is due to faster initiation orslower elongation dynamics. Here, we address this question computationally using 50-mRNA folding energy as a proxy for translationinitiation rates and codon bias as a proxy for elongation rates. We report a significant trend toward reduced 50-secondary structure inshorter coding sequences, suggesting that short genes initiate faster during translation. We also find a trend toward higher 50-codonbias in short genes, suggesting that short genes elongate faster than long genes. Both of these trends hold across a diverse set ofeukaryotic taxa. Thus, the elevated ribosome density on short eukaryotic genes is likely caused by differential rates of initiation, ratherthan differential rates of elongation.
Non-Clinical Safety, Pharma Research, F. Hoffmann-La Roche Ltd., Basel, Switzerland The Patchliner®temperature-controlled automated patch clamp system was evaluated for Ralf Franz Kettenhofen, Axiogenesis testing drug effects on potassium currents through human ether-à-go-go related gene AG, Germany (hERG) channels expressed in Chinese hamster ovary cells at 35–37˚C. IC50 values for a