Aacp paperwork
• Aim is provide comprehensive paperwork for
• Compiled for ease of use in either office or
• For adult and child • Axis 1 and Axis 11 considerations to help
classify difficulty and treatment outcomes of
• Medical and Dental History Office
– Adult – Child
• History of Pain Condition Surgery • Intraoral Examination • Differential Diagnosis of OFP • Records check Office/Surgery • TMJ Symptoms Review Sheet • Adjunct Paperwork Office/ Surgery
– Pain diary – Sleep diary
Adult/Child Medical Dental History
• Office Use data • History of Medications
– Prescription. OTC, Homeopathic – Reason using them – Time of intake – Dosage – Everybody Lies
• Dr R Kulich Tufts
Adult/ Child Medical History
• History of past Treatment
– May give an indication of types of treatment that wil or wont
– May indicate nature of chief complaint, eg neuropathic,
• Systems Review
– Organizes the medical conditions logical y – Al ows patterns/ relationships to be seen clearly – Can be important in later facial pain/ headache diagnosis
• SSI • 3 questions are a quick screening tool for pain of TMD
• Sensitivity/specificity >0.95
Adult/ Child Medical Dental History
• Axis 11 psychosocial screening questionnaires • More indicative of treatment outcomes than Axis 1 pain
• Are used to classify patients by difficulty of treatment • Are not meant to be used by dentists to diagnose anxiety or
depressive disorders
• Mandatory if pain present > 6mths • Or if previous unsuccessful treatment • Identify barriers to treatment response • Contributors to chronicity • Alternative targets for therapeutic intervention
Adult/ Child Medical Dental History
• Questions 1-9 • PHQ 9 for depression • Cutoffs at 5 mild • 10 moderate • 15 mod-severe • 20 severe • Levels of depression
Adult/ Child Medical Dental History
• Q 10-16 • GAD 7 for anxiety • Cutoffs 10
• 15 severe • Q 1-14 • PHQ15 for physical symptomms • 5 low • 10 medium • 14 high somatic symptom severity
TMD Symptom Questionnaire
• Q1-7 • Enables diagnosis of new headache disorder • Headache due to TMD • Requires temporal headache • And change in pain intensity with function • Q 8-14 establish presence of disc displacement • MRI required for definitive diagnosis of disc
• CT for definitive Diagnosis of DJD • Exception is DDWOR with limited opening(<40mm)
Adult/ Child Medical Dental Hisotry
• JFLS • Asses global limitation of function of jaw • GCPS • Broken into Characteristic Pain Intensity (CPI) • Q1-5 • ≥ 50/100 is high intensity • Pain Disability Rating • Q 6-8 • No of days pain interferes with work • Measurement of disability
Adult Medical Dental History
• Please note Child form does not have
comprehensive Axis 11 screeners
• There is no reliable screening tool for Axis 11
disorders for children
• The best tools at present have sensitivity/
spec around 0.4 so not included
Adult/ Child Medical Dental History
• Sleep Screening • Adult form has Epworth • Subjective screening tool for tiredness • And Berlin Questionnaire • Slightly less subjective than ESS
Adult/ Child Medical Dental History
• Child Screening has Pediatric Daytime
Sleepiness Scale
• Endorsed by ATS • Screens for sleepiness and negative sghool
outcomes in middle school ages 11-15
• Has similar characteristics to ESS
Adult/ Child Medical Dental History
• History of missing teeth, premature birth,
extractions and hypermobility given by Prof
Guilleminault at recent conference as risk
• Mostly unpublished data but reasonable
Adult/ Child Medical Dental History
• Pain Drawing • Useful to see
– Overal pain experience – Referral patterns for myofascial pain in head and
– Localized pain areas in the head may indicate
localized problems
– Widespread pain indicates the need for referral
for further investigation
History of Pain Condition
• 1st job is to work out • WHO SHOULD NOT BE IN YOUR CHAIR • Screening for life threatening secondary causes of
• Systemic symptoms • Neurologic signs or symptoms • Onset sudden • Onset> 40 • Pattern change
History of Pain Condition
• Systemic symptoms or disease • May be indicative of encephalitis, bacterial
infection, cancer, HIV, immunotherapy
– Fever – Weight loss – Arthralgias – Stiff neck – Rash
History of Pain Condition
• Neurological Signs or symptoms • Confusion, clumsiness, weakness, aphasia,
numbness, dizzyness, visual problems
• Need to rule out primary headache disorder
eg migraine, basilar migraine
• Or may be TIA, stroke, mass lesion, infiltrating
lesion affect CNs, artereovenous
malformations, thrombotic disease,
malignancy, infections
History of Pain Condition
• Onset Sudden • Sudden onset severe general or localised headache • To be considered severe until proven otherwise • DD Subarachnoid or intracerebral bleed • Ruptured or unruptured aneurysm • Cerebral venous thrombosis • Carotid or vertebral artery dissection • Cerebral infarction • Encephalopathy • CNS infections
History of Pain Condition
Headaches brought on by a cough, sneeze, straining,
Headache awakening from sleep rule out causes of
increased intracranial pressure
post traumatic headache can be due to fracture,
hematoma, infection
Positional headache Worse standing better lying may be CSF leak Worse lying better standing may be intracranial mass Headache in morning OSA, MOH, Tumour, Parafunction
History of Pain Condition
• Onset after 40 • New onset or change in pattern • Most migraines before 30yo • Ha in older no prior history may be tumour,
vascular disease/ hormonal
• ESR rules out giant cell arteritis • CBC (blood) anemia anad blood dyscrasias • T4 rule out thyroid disease
History of Pain Condition
• Pattern Change • 1st or worst headache • Change in frequency, • Severity, • Associated symptoms, • Quality • Warrant investigation
History of Pain Condition
• Location • Has it changed • Does it cross the midline • Does it change during the pain episode • Use 1 finger • Site is not always source • Is chief complaint stimulated by pushing
History of Pain Condition
• Onset • Was there an event associated with onset eg
trauma physical/emotional
• When • Time of day • Sudden or gradual
History of Pain Condition
• Quality • Types of pain eg burning sharp dull can be associated with
different causes
• This must be taken with caution • Musculoskeletal
– Dull – Aching – Pressure – Depressing – Tight – Stiff – Can be sharp
History of Pain Condition
Diagnosis only after exclusion of al possible causes
History of Pain Condition
• Intensity • Subjective • Affected by emotional state and sleep status and
medication (can increase or decrease it)
• 0-10 where 0= no pain 10 = most extreme pain
• VAS = 10cm line • Sensory changes may affect intensity • Can be related to intracranial disorder,
neuropathic, or central pain
History of Pain Condition
• Frequency and Duration • Does pain occur in clusters • Are there periods of remission. How long • Normal pain is not continuous • Some headache disorders have characteristic
durations of pain
History of Pain Condition
• Associated Symptoms • May aid diagnosis • Visual or sensory changes may go with
• Drooping eyelids, conjuctival tearing may be
associated with cephalalgias
History of Pain Condition
– Numbness – Hyperalgesia – Paraesthsia – Allodynia – dysesthesia
– Increased by increasing ICP eg valsalva, physical activity, bending over – Sensitivity to light, sound – Nausea, vomitting
Musculoskeletal pain
– Flushing – Hyperalgesia – Can be referral – Worsens with function
History of Pain Condition
• Alleviating/ triggering • Jaw function yes/no • Posture • Sleep • Wind/touch/shaving/stress • How much medication and types • Massage/ PT
Sleep Complaints
Can you fall asleep
Do you stay asleep
Do you have trouble going back to sleep
Do you wake often
Do you wake with a fright
Do you dream/ nightmare
Do you snore/ stop breathing/ grind/ clench
Do you go to the toilet
Do you sleep talk/walk/act out dreams
Do you wake with a headache/ dry throat/ sore neck/blocked nose/red eyes
Do you feel good in the morning
Do you nap during the day
Do you consume alcohol, coffee, tea, soft drink, dairy gluten after 2pm and
Intraoral Examination
• Make sure that their dental examinations are
• Do they have or need current BW x-rays • Check probing depths for perio/ root
• Rule out dental/ periodontal/ mucogingival • Examine intraoral tissues including base of
Intraoral Examination
Check occlusal issues
Correlative data only
Unilateral x-bite
>6 missing posterior teeth
Interferences to CO
Consider denture patients may have all/most of these
examine/ palpate associated structures
Temporal arteries
Salivary and lymph glandss
pontaneous flow, colour and consistency of saliva
Refer when appropriate

Intraoral Examination
• Muscle Palpation • Muscle Pain • Myalgia
– Localized. Confined to site of palpation – Myofascial pain with spreading beyond site of palpation – Myofascial pain with refera lbeyond boundary of muscle
– Record location of referral
• 1kg pressure for 2 seconds for myalgia • 1kg for 5 seconds for spreading/referral
Intraoral Examination
• Myalgia • Provocation tests • Pain on opening jaw muscles • Pain on palpation of the temporalis and masseter • Lat Pterygoid only able to be tested by provocation….
Push jaw forwards against pressure
• Buccinator in approximately position of Lat Pterygoid • Is often tender in cases without TMD • Always ask DOES THIS REPLICATE THE FAMILIAR PAIN
Intraoral Examination
– Height – Weight – BMI – Neck circumference – BP – O2 saturation (if sleep)
Intraoral Examination
• Cervical examination for middle age person • Normal CROM lateral is 65-75 degrees
• Lateral tilt 35-45 degrees • Flexion 50-60 degrees • Extension 60-70 degrees • CROM decreases by 5 degrees extension and 3
degrees other movements over 10 years
• Head on chest and move left and right = C1/C2 • Look symmetry and pain

Intraoral Examination
• Mandibular Range of Motion • Vertical norm = 40-55mm • Max opening + overbite • Lateral = 7mm • Active mouth opening = unassisted • Passive = assisted mouth opening • Record pain and joint noises during opening • Deviation and deflection • Provocation tests- hard/soft end feel
Intraoral Examination
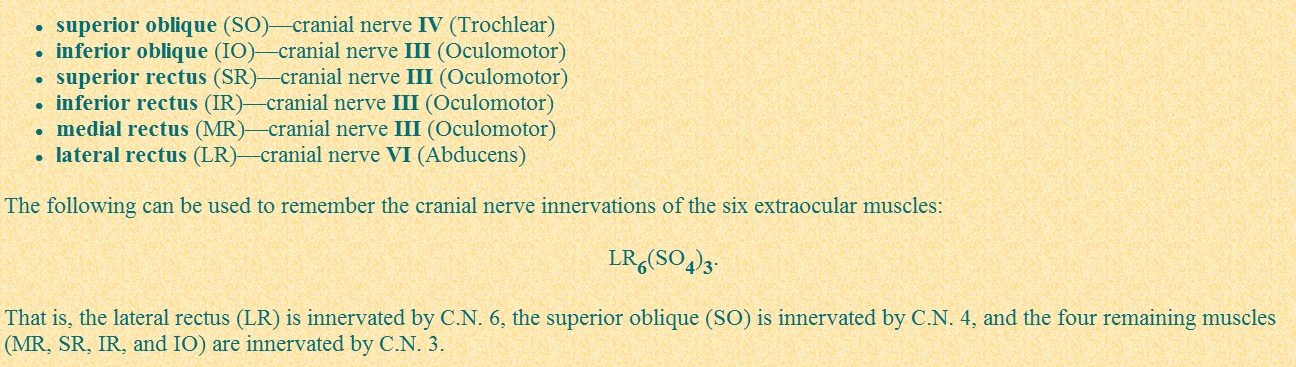
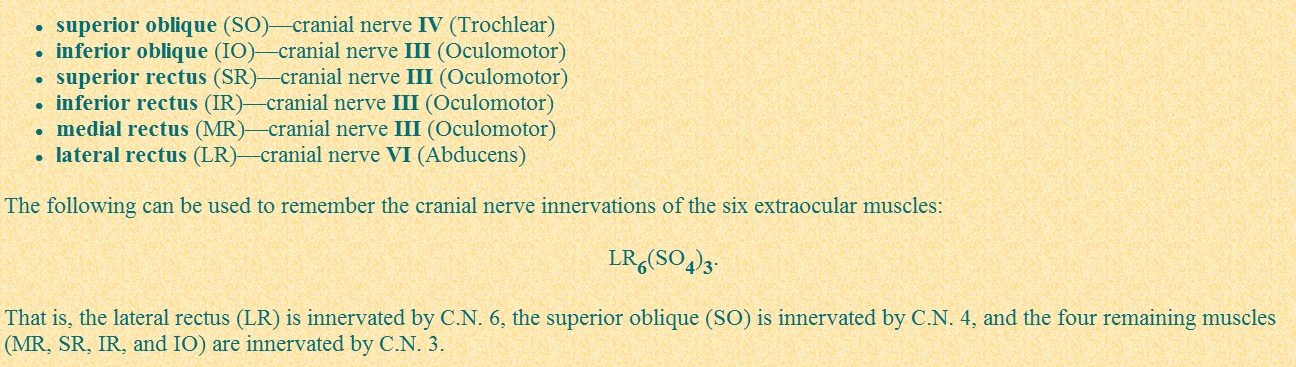
• Cranial Nerve Eval • 1 Olfactory camphor, coffee, vanilla • 2 Optic Visual aacuity, visual field P • 3 Occulomotor Pearl, eyelid elevation,
• 4 Trochlear Downward gaze in

Intraoral Examination
Intraoral Examination
• 5 Trigeminal Light touch to face,
muscles of mastication,
Downward gaze in
Facial expressions, corneal
reflex, taste to ant 2/3
Hearing, nystagmus on EO
tests, caloric testing (COWS)
Intraoral Examination
• 9 Glossopharyngeal gag, taste to post 1/3
Speech, palatouvula
• 11 Accessory
SCM and traps against
• 12 Hypoglossal Tongue bulk, strength
• Make sure to record deficits position and size on

Differential Diagnosis
• Axis 1 structural • Axis 11 psychosocial • Can change during course of lifetime in each
• Record need for MRI/ MRA/ med CT pr if
Differential Diagnosis
• Intracranial
– Acute ischaemic cerebrovascular disease – Intracranial haemorrhage traumatic/ nontraumatic – Unruptured vascular formation – Venous thrombosis – CSF pressure high/low – Chiari Malformation – Neoplasm – Infection – Noninfectious inflammatory disesase
Differential Diagnosis
• Acute Ischaemic Cerebrovascualr Disease • Pain mild-mod • Nothing pathognomic about qualilty, severity, location • Person>50 • Neurologic deficits and related to time of head pain • Different headache from familiar • Vertebral and basilar artery more likely to cause pain
• Diplopia, weakness, vision obscured, numbness,
altered cognition, dysarthria, aphasia ataxia
Differential Diagnosis
• TIA deficits resolve in 20min-24 hrs • Vascular risk factors, (diabetes, coronary disease HBP,
High cholesterol, nicotine)
• Can use CT esp if acaute bleed • MRI (diffusion weighted) better • DD • migraine, • Older migraineur new neurologic symptoms
considered to have vascular issue until proven
• Usual y treated with vasoactive drugs

Differential Diagnosis
Intracranial Haemmorhage
Epi or subdural haemotoma
Epidural haematoma after blunt trauma
Pain and change in cognition rapid
RAPID surgical drainage
High Suspicion after Trauma
Subdural haematoma can be acaute, subacute, chronic
Older > risk due to falls and fragile veins
Trauma may be minimal/ indirect
Symptoms several hours to days after.
Pain not always chief CO
Anticogulants, NSAIDs increae risk
Neurologoical deficit, personality change, somnolence, visual disturbance,
hemiparesis, hemisensory changes, visual field disturbance
May be surgical y treated but usual y monitored
Differential Diagnosis
• Nontraumatic • Intracerebral haemmorhage • Acute neurologic deficits • Related to HBP, neoplasm arteriovenous
• Occurs in brain parenchyma • Can cause coma, death • Effect dependent on cause and size and resultant
destruction of cerebral tissue
• Can be compression of CV 111
Differential Diagnosis
• Subarachnoid hemorrhage • Characteristic HA • Sudden onset thunderclap headache • Max intensity seconds to 1 minute • Eg stopped in middle of sentence, hit by baseball
• Nausea, vomiting, stiff neck, loss of
• Send to emergency via ambulance • Head CT, lumbar puncture (blood)

Differential Diagnosis
• Arteritis • Initial presentation can be severe unilateral temporal headache • Giant cell aerteritis (temporal A) may lead to blindness • Occlusion of carotid artery • To be ruled out in al especial y women >50 with new/ persistent
headache 1 or both temples worse with cold and with jaw
claudication (tiredness, pain on chewing), pain combing hair,
polymyalgia rheumatica, stiff/sore neck, shoulders, proximal arms
• Tests ESR (>90), biopsy • High dose sterids • Enlarged tender temporal arteries reduced pulsatility
Differential Diagnosis
• Carotid or Vertebral Artery Pain • Ipsilateral pain in neck, face, head • Neurological symptoms/ TIA/ stroke • May be associated with pulsatile tinnitus or Horner
Syndrome (ptosis, annihydration, constriction of pupil, red
conjunctiva, enopthalmours)
• due to sympathetic fibres on Carotid Artery • May be trauma (surfing, chiro, blunt trauma), spontaneous,
arterial damage (fibromusculr dysplasia, migraine)
• Listen for bruits over orbit or temporal bone • Refer to neurologist
Differential Diagnosis
• Unruptured Vascular Malformation • Saccular aneurysms, arteriovenous malformations,
dural arteriovevenous fistulae, venous cavernous
• May be present long term and silent or nonspecific
• May mimic migraine/TTH and respond to same
• Any age • May be pulsatile tinnitus, family history • May use MRA/ CTA
Differential Diagnosis
Venous Thrombosis
Pain may be acute severe- subacute- chronic
Severe new headache with visual disturbances
Predisposing factors, dehydration, oral controceptive, postpartum,
prothrombotic blood dyscrasias, neoplasms, mild-mod head trauma, local
Refer to neurologist
Modify predisposing factors/ 6mths anticoagulant therapy
Signs of increased intracranial pressure
– Nausea – Vomitting – Pappil edema – Seizures – Neurologic deficits
Differential Diagnosis
CSF pressure change
Nonspecific headache in any region, but commonly hoocephalic daily headache,
intermittent visual disturbances, pulsatile tinnitus
Worsens with valsalva, supine
Associated with nausea, vomiting, visual problems, neurologic deficits, blindness
Watch for extraoccular movement abnormalities
Especially diplopia, early papil edema
Young obese females
OC/ tetracycline
Beware of papil edema and bilateral abduces paralysis
Normal MRI, lumbar puncture pressure > 200-250mmHg
Treat with modification of risk factors, acaetazolamide ( dec CSF), steroids (dec
edema), multiple lumbar puncture
Differential Diagnosis
• Low CSF • Increaed headache standing and decreased with supine within
minutes (Effect decreases with time)
• Neck pain/stiffness, tinnitus, hyperaccusia, photophobia, nausea,
paresthesia of neck, arms
• May be iatrogenic (dural/lumbar puncture) • Spontaneous (meningeal diverticulae, connective tissue disease,
weakened dura mater
• Traction on dura mater and sensitive pain sensitive vasculature on
standing due to sagging brain
• MRI with gadolinium • Treatment bed rest 2-3 days no head elevation • Mild OTC analgesics, caffeine, theophyl ine, epidural blood patch • Headache gone 48-72 hours after treatment
Differential Diagnosis
• Chiari Malformation • Herniation of cerebel ar tonsils3-5mm below FM • May include hydocephalus, myelomeningocele,
sysssringomeliaspinal cord cavitations, distortion of
contents of middle and posterior cranial fossa,
flattening pons, kinking of brainstem
• May cause traction or compression of CN • Headaches, hemifacial spasm, coughing, inability to
speak, dysphagia, nystagmus, weakness of limbs
• Can be congenital/ acquired • May require surgical decompression
Differential Diagnosis
• Neoplasm • Headaches in approx 50% of cases • Primary presenting symptom in 20% • May have focal neurologic symptoms or seizure • May be due to increased ICP, or meningitis • Weight loss, personality changes, weakness,
numbness, trouble walking, visual disturbances,
progressive neurologic disturbances
• New headache plus above needs investigation
Differential Diagnosis
• Infection • Bacterial meningitis, lymphocytic meningitis, encephalitis,
brain abscess, subdural epyema
• Holocephalic headache associated with fever, arhtralgias,
stiff neck, photophobia, nausea, altered consciousness,
• Can occur within minutes to hours • Menigitis patients have stiff necks, cant flex • Positive Kernig and Brudzinski sign • HSV most common cause of nonepidemic viral encephalitis,
also fungal and HIV
• Blood cultures, CSF testing
Differential Diagnosis
• Noninfectious Inflammatory Disease • Neurosarcoidosis • Aseptic meningitis • May be severe headache with or just after
IHS classification
17% of women and 6% of men in the US have migraine
5 attacks of Idiopathic recurring headache lasting 4-72 hours
70% as migraine without aura
30% as migraine with aura
Usually unilateral, but bilateral in 40%
Most commonly occur on wakening
Both photophobia and phonophobia must be present
2 major theories of causation, that the migraine begins central y and then
activates the peripheral branches of the trigeminal nerve
Or that the peripheral braches of the trigeminal system are activated and
the central involvement of the trigeminal system is a form of central
sensitization, explaining the allodynia experienced on he facial skin.
Familial Hemiplegic migraine related to mutations in 3 different ion
Phases of a Migraine
– The Prodrome Phase – Occurs in 30% of migraineurs – Occurs equal y in migraine with and without aura – Starts from hours to days prior to a migraine attack – Changes in mood or behaviour – Depression, craving for special foods, yawning
– Aura – A series of idiopathic recurring neurologic symptoms – Develop gradually over 5-20 minutes, but <1hr – Onset of headache within 60 mins of aura abating – Not all auras are fol owed by a migraine – Visual Disturbances fortification pattern, photopia, scotoma – Adults may have sensory symptoms such as unilateral
paresthesias, numbness, tingling,unilateral weakness,
aphasia and speech disturbances
– Aura symptoms are reversible
• Nausea/ vomitingPhase 3
– The Headache Phase – Throbbing moderate to severe headache – 2-4 of – Usual y unilateral, throbbing headache – Photophobia and phonophobia – Nausea and vomiting – Pain aggravated by routine physical exercise – Pain in adults may present as a headache, or pain in the
teeth, masticatory muscles,or the middle or lower third of
• Phase 4 • Termination • Phase 5 • Postdrome
– May be exhausted/ confused/ fatigued – Loss of appetite and aching muscles – Dul diffuse aching headache for 1-2 days
Episodic Versus Chronic Migraine
• Chronic Migraine
– p> 80% have a Past history of migraine – Transformation of an acute episodic migraine to a daily attack – Typical y a slow process – Headaches increase in frequency – Intensity declines – Periodic superimposed attacks of migraine – 15 days/ month for >3months without MOH =chronic migraine – Photophobia/ phonophobia/ GIT features are absent – Similar to TTH – Migraineurs taking triptans and other analgesics are susceptible
– Status migranosus migraine>3days
Migraine Therapy
1. Patient Education and Recognition of migraine triggers
Migraine Therapy
2. Nonpharmacologic
• Biofeedback training • Cognitive behavioural therapy • Psychotherapy • Exercise programme • Dietary modification • Migraine and TMD comorbid conditions • To treat migraine the TMD needs to be treated • And vice versa
Migraine Therapy
3. Abortive Therapy
Use a Phase Specific concept
Stratified Care approach
Start with OTC analgesics, eg paracetamol, NSAIDs, fiorinal , caffeine to abort
migraine in the prodrome or aura period
Use a stronger rescue medicine in the late stage
Major rescue medications are 5HT receptor agonists
– Injectable – Quickest:- average to relief 41minutes – Short ½ life so recurrence commmon – Max al owance 2 x 6mg subcutaneous injections in 24 hrs – Oral – Usually 50-100 mg – Nasal Spray – For use in patients with nausea and vomitting – Comparable efficacy to oral dose, but bitter taste – Triptans have cardiovascular side effects, but not likely at the dose used for
migraine treatment
Migraine Therapy
4. Prophylactic Therapy
If headaches are control ed at 6 months t aper or withdraw medication for a trial
– Suppress peripheral beta adrenergic receptors that promote vasodilation – Propanolol and atenolol most common – Should not be used in asthmatics or people with depression or Raynauds disease – Antidepressants – TCA – Efficacy only established for amitriptyline – Start at 10mg titrate to 25-75 mg at bedtime – SSRI – Major side effect bruxism – NSAIDS – Use at times when migraine most likely to be triggered, eg the week before menses – Need to take NSAID before and not after PG formation – Calcium Channel Blockers – Not as effective as beta blockers – Anticonvulsants – For use in people who cannot take other classes of prophylactiv drugs – Oeriodic liver function and monitoring of blood levels recommended – Botox – Just approved by FDA for chronic migraine
Tension Type Headache
• 74% of the population may experience this 1/year • Dull non-pulsatile tightness felt in the occipital, parietal,
temporal and frontal regions
• 90% of the time it is bilateral, mild-moderate • 30 minutes-72hours • Photophobia or phonophobia, but not both • Etiology unclear • TTH is NOT the same as pain from referral of myofascial
trigger points, headache associated with sleep bruxism or
with sleep apnoea(?)
Tension type Headache Management
• Identify triggers (headache diary) • Reduce caffeine, alcohol and headache medications. • Avoid stressors • No evidence based protocol for best medications • TTH can be secondary, and the cause of the
headache needs to be identified.
• Treat the cause of the tension, eg TMD, OSA, bruxism
(Okeson and Leeuw 2011)
Cluster Headache
• Presentation • Male:female 3-4:1 , 0-09-0.32% • Onset between 20-40 years • Attacks occur in clusters over weeks or months • 15-180 minutes • May occur every few days to 8x/day • Attacks occur in clusters from 2weeks- few
Cluster Headache
• May be precipitated by alcohol, nitroglycerine,
• Precipitating factors do not initiate an attack
during remission
• May be related to changesin the posterior
• Episodic >1 month of headache free days/ year • In 10% attacks may become chronic= >1 year with
no remission or remission <1 month
• Often misdiagnosed as dental/ sinus/ TN pain
Cluster Headache
• Pain is boring, there's a hot poker in my eye,
my eyebal is being pushed out
• Rarely throbbing • Rapid onset • Builds to a peak in 10-15 minutes • Unilateral centred around orbit or the
Cluster Headache
• Autonomic symptoms due to parasympathetic
overactivity and always accompany the pain
• Ipsilateral lacrimation
• Conjunctival injection
• Ptosis and miosis
• Pain in the distribution of the carotid artery, eg maxil ary
posterior teeth and anterior temporalis region
• 50% may have ipsilateral posterior cervical tenderness
• Ipsilateral forehead and facial sweating/ pal or
• Bradycardia, ataxia,vertigo,syncope,hypertension,
• Increased gastrointestinal acid
Cluster Headache Management
• Abortive • Oxygen 7-10l/minute for 15minutes • Effective in 70% of patients within 5 • minutes (CDB 2008 weak evidence only) • Triptans sumatriptan 6mg subcutaneously/ • zolmitriptan 10mg intranasal (CDB 2010) • often terminates attacks within 5 minutes • Dihydroergotamine (DHE-45) • Most effective • Injectable< IM< Nasal spray for speed of onset
Cluster Headache Management
Verapamil 120-480mg/day
Start at 80mg and titrate to 160mg tid-qid
C.I. cardiac conditons
Lithium Carbonate
Especial y effective in the chronic cluster headache patient
Monitor toxicity through blood tests
Ergotamine Tartrate
Useful in nocturnal attacks when taken at bed time
Divided doses up tp 4mg/day
Radiofrequency Ablation of the pterygo-palatine ganglion
Only in those refractory to pharmacologic management
Occipital nerve stimulation last line of chhoice
Paroxysmal Hemicrania
• Shorter attacks than CH • 2-30 minutes/ more frequent • Female>male • Unilateral predominantly periorbital • Autonomic symptoms as per CH • Episodic = attacks from 7 days- 1 year with pain
free periods of 1 month
• Attacks>1 year withotu remission or remisison <
1 month= Chronic
• 100% responsive to indomethacin
• Short-lasting Unilateral Neuralgiform headache attack
with Conjunctival injection and Tearing
• Unilateral supraorbital / orbital/ temporal stabbing or
• Lasts 5-240 seconds with 3-200 attacks /day • Includes autonomic symtoms • If only 1 of tearing or conjunctival injection is presenet,
or if there are other autonomic symptoms = SUNA
• Short-lasting Unilateral Neuralgiform headaches with
cranial Autonomic Symptoms
Differential Diagnosis SUNCT/SUNA
• TN • SUNCT attacks more likely to be located in V1 • SUNCT/SUNA less likely to have a cutaneous trigger
• SUNCT/ SUNA less likely to have a refractory period
SUNCT/ SUNA not responsive to high-flow oxygen like CH SUNCT/SUNA not responsive to indomethacin like PH SUNCT/SUNA treated with lamotrigine/ topiramate/
Secondary Headache Disorders
• Headaches secondary to another medical condition • Can include
– Temporal arteritis – Post traumatic Headache – Medication Overuse Headache – Mountain Sickness – Headache Related to TMD – Phaeochromocytoma ( neuroendocrine tumour of medulla of the
– Intracranial hypertension – Intracranial Infection – Intermittent hyprocephalus – Glaucoma – Optic neuritis
Headache Related to TMD
• A Headache that is affected by jaw movement, function or
• Can replicate headache with provocation testing of the
masticatory system
• Must hav • Headache of any type in the temple AND • Headache modified with jaw movement, function or
• Must be able to stimulate familiar headache with palpation
of temporalis muscles or vertical lateral or protrusive
movements of the mandible
• Headache is not better accounted for by any other
headcahe diagnosis
Medication Related Headache
Medication related headache may be due to medication overuse, or the
side effects of a prescribed medication
MOH is a subset of chronic daily headache
Overuse is defined as the use for more than 3 months of at least one
acute treatment medication
Ergotamine, triptans, and/or opioids used on 15 or more days/month or
simple analgesics
The headaches worsen (usual y in frequency) with the medication
May account for ½ the cases of CDH, and is the most common form of
secondary chronic daily headache.
The headache initial y worsens when the medications are withdrawn,
and then improves
Neuropathic Pain
Episodic or continuous
Trigeminal Neuralgia
Episodic unilateral pain in the distribution of 1 or more division of CNV
Brief electric shock like pains 155/1 000 000
Precipitated by nonpainful stimuli trigger zone) or may be spontaneous
Pain may last seconds to minutes
Refractory period
May get fusion of paroxysms
May have remission for days to years which decrease with time
Pain does not usual y disturb sleep
No neurological deficits
V11 and V111 most common V1 only 1-2%
RHS>LHS, does not cross miudline
May be bilateral in 3-5%
Average age of onset = 50 years
• Demyelination or loss of myelin sheath • Most commonly from compression of trigeminal nerve root by
blood vessel at level of entry into pons
• Leads to spontaneous neve firing and ephaptic cross talk of nerve
• May also be related to
– Compressive tumours – Arteriovenous malformations – Saccular aneurysm – MS increases OR for TN x 20- beware of bilateral TN or TN early onset – Infarction of brainstem – Angioma – Genetic eg Charcot-Marie Tooth Disease – Demyelination does not explain al of the characteristics of TN
• Triggering may explain
– Light touch trigger zone – Amplification (spreading response beyond original area_ – Stop mechanism (lasting pain response and abrupt stop) – May have ectopic pacemakers sites at points of
demyelination that are hyperexcitable and fire with little or
– Some sites may have continuous firing for dull background
– Ephaptic transmission or crosstalk amplifies transmission – Hyperpolariztion explains both stop and refractory period
TN Classification
• >85% are classical TN with Microvascular compression • Symptomatic or secondary caused by verifiable lesion ( tumour,
• Must use imaging and CN evaluation • Must be differentiated from
– dental pain, – sinus disease – Head and neck neoplasms and infections – Postherpetic neuralgia – Persistent idiopathic facial pain – Headache associated with TMD – SUNCT/SUNA – Jabs and Jolts
• Medical • Anticonvulsants • Tegretol (carbamazepine) most effective • Initial response 70% decreases to 20% after 5-16 years • Start 100mg/day • Increase by 100mg every 2 days to max of 1200mg/day
in divided dose can be 2-4 x/day as needed
• Side-effects drowsiness, dizzyness, nausea, anorexia,
feel foggy. Aplastic anaemia and trnsient leukopenia
• Need to monitor blood levels and kidney function
• Gabapentin (neurontin) • Minimal side-effects cf carbamazepine • No RCTs • Pregabalin (lyrica) • Also used • Personal experience is that carbamezepine is most
• If unwanted side effects use in a reduced dosage in a
cocktail with other medication types or other
• Best to let GP deal with medication
• Oxcarbazepine (trileptal) • Ketoanalogue of carbamazepine • No bone marrow or hepatic toxicity • Start at 150mg twice daily • Increase as tolerated to 300-600mg twice daily
up to max of 2400mg/day
• Same side effects as carbamazepine except is an
increased risk of hyponatremia (low sodium-
cerebral edema, headache, confusion, seizures,
• Other anticonvulsants • Lamotrigine (lamictal) • For rerfractory cases especially related to MS • 100-400mg daily • Stevens Johnson type rash can be associated with this, as
wel as diplopia, ataxia, dizzziness, headache, GIT
• Topiramate ( topamax) • Start at 25mg bd • Increase by 100 mg/day every 1-2 weeks aiming for 100-
400 mg dasily in 2 doses
• Anorexia, weight loss, somnolence, anxiety fatigue
• Other Medications • No others have evidence ( Cochrane Data Base) • Others used include • Baclofen centrally acting muscle relaxant GABA
• Reduce carbamazepien 25% before adding • 5mg tid increase by 5-10 mg every 2-3 days • Max dose 80mg/day
• Clonazepam • Benzodiazepine with anticonvulsant effects • Start 0.5-1mg/day in divided dose • Increase by 0.5-1mg every 3-7 days to max of
• Dental Management • Make sure that patient is dental y fit. • Check for dental causes eg TA/ TMD/ root fracture • Local Anaesthetics • LA in the trigger zone wil temporarily remove the pain of TN • As LA is a membrane stabilizing agent it may help to decrease the
number and severity of the events
• There have been some reports that the adrenaline in some LA
agents can upregulate pain in TN
• Patients with TN are at risk for exacerbation of the TN after complex
dental procedure, and especial y RCT
• Discuss with GP if can increase anticonvulsant therapy levels prior
to and just after dental visits
• Topical Agents • Applied via a neurosensory stent • Avoids GI 1st pass effects • Systemic absorption depends on the vascularity of the area • Can use any med that can be used systemical y in a PLO gel • Lignocaine
• Amytriptyline
• To be made by a compounding pharmacy
TN Surgical Therapy
– MVD – Stereotactic radiosurgery (Gamma Knife) Delayed onset of pain relief and 61-
90% recurrence 10-27%
– Neurectomy 50-64% short term only – Cryotherapy short term 6-12 months can have AFP and sensory deficits – Alcohol injection Higher recurrence fewer side effects than above. SE include
hypo and paraesthesia, dysesthesia, fibrosis, necrosis, reactivation of Herpes
Zoster Pain relief<1year
– Near Gasserian Ganglion – Radiofrequency thermocoagulation – Percutaneous glycerol – Bal oon microcompression Immediate pain relief 91-100%, 2-5% recurrence at
18months, 19% at 5 years and 32% at 20 years
Pretrigeminal Neuralgia
• Continuous dull achy pain sometimes
• Diagnosis is dull tooth-ache like pain normal
neurologic and dental exam and normal CT or
Glossopharyngeal Neuralgia
• Similar character of pain to TN • In distribution of glossopharyngeal nerve and auricular
and pharyngeal branches of vagus
• Location ear, base of tongue, tonsil ar fossa, below
• Unilateral, seconds up to 2 minutes • Provoked by swal owing, chewing, talking or yawning • Comorbid with TN in 10-12% • Normal CN evaluation • MRI with contrast to exclude symptomatic GN
Nervus Intermedius Neuralgia
• Rare • Unilateral paroxysms of pain in inner ear • Last seconds to minutes • Trigger zone in posterior wall of auditory canal • Disorders of lacrimation, salivation, taste
sometimes present
• Often associated with Herpes Zoster • Rx medical as per TN • Can resect nervus intermedius or chorda tympani
Other Neuralgias
• Painful Opthalmoplegia
– Orbital pain with paralysis of 1 or more cranial nerves – 111, 1V, V1 – Pain relief within 72 hours of steroid therapy
• Superior Laryngeal Neuralgia
– Severe paroxysmal pain in throat, submandibular area,
– Duration minutes to hours – Triggered by swallowing, straining the vboice, turning the
– Trigger point on lateral of throat over the hypothyroid
Continuous Neuropathic Pain
• Idiopathic Trigeminal Neuropathic Pain • Atypical Facial Pain/ Peripheral painful trigeminal traumatic
neuropathy/ Atypical odontalgia
• Diagnosis by exclusion of al other conditions • Begins with partial or complete deafferentation, eg pulp extirpation
• Negative symptoms = sensory loss or decrease • Positive symptoms may be processesof regeneration and
• Dysesthesia, paresthesia, hyperalgesia • 3-7% of RCT may end with AO • Postimplant neurosensory disturbance = 0.6-36% • Dull aching persistent pain, often with history of multiple dental
AO versus Pulpal pain
• No local pathologies or radiographic findings • Constant pain in tooth with no known source or pathology • Local provocation does not consistently alter the pain • Toothache is unchanging cf pulpal pain which resolves or
• Repeated dental therpies fail to resolve the pain • Response to local anaesthesia is equivocal (peripheral +
• Pain must have been present for >4 months • No referred pain • May be a history of trauma or deafferentation • Rx TCAs gabapentin, pregabalin, tramadol, topical lidocaine
Postherpetic Neuralgia
• Normal recovery from herpes zoster = 3-4 weeks • Some have irreversible damage to skin and sensory
• Infrequent in general population but 50-75% in older
• Painn develops in aacute phase and recurring or persisting
for >3 months
• Burning with brief stabbing with hyperalgesia and allodynia • Risk factors age, female, prodrome, severe rash and pain • Rx high dose gabapentin, carbamazepine +clomipramine
and desipramine, and tramadol, topical lignocaine
Anesthesia Dolorosa
• Painful area of anaesthesia or dysesthesia • Arises after damage to CNV, ganglion, or nuclear
• Most common after surgical therapies for TN • Bal oon microcompression, MVD and gamma knife
surgery not typical y associated with it
• Accompanied by increased sensitivity to pain and
temperature in one or more divisions of the trigeminal
• Treatment anecdotal TCAs, and anticonvulsants • Microsurgical repair effective in only 1/7
Central Post Stroke Pain
• Pain, dysesthesia, impaired sensation to pinprick and
temperature (>50%)
• Due to a lesion of the spinothalamic pathway not the
trigeminal nerve
• Most commonly a vascular lesion • Pain usually in half of the body contrlateral to the
• Also caused by MS, syringobulbia, trauma,
neurosurgical lesions, tumour, vascular malformations,
some inflammatory disorders
• Rx amitriptylene, lamotrigine
Complex Regional Pain Syndrome
• CRPS 1 was called reflex sympathetic dystrophy and
CRPS11- causalgia
• Persistent burning pain with allodynia and hyperalgesia • At some stage there is swelling, changes in blood flow,
and/or abnormal sudomotor activity
• CRPS1 symptoms are disproportionate to a mild injury • CRPS 11 there is evidence of nerve damage preceding the
• For diagnosis must have ¾ reported and 2/4 at time of
evaluation of sensory, vasomotor, sudomotor/edema, and
motor/trophic changes
• Usually in upper and lower extremities
Burning Mouth Syndrome (BMS)
• Probably neuropathic but with peripheral and central
• Burning of the mucosa/ dysgeusia/ xerostomia with no
pathology/abnormalities
• Primary (neuropathic) or secondary • Prevalence 0.7-15% • Rare under 30yo, most common in postmenopausal
• Bilateral symmetric distribution, often anterior 2/3rds of
tongue, dorsum and lateral surface, anterior hard palate
and mucosa of lower lip
• 17-33% link onset to upper respiratory tract infection,
dental procedure, or medication
• In 50% pain decreases with distraction oral
intake or stimulation
• Pain increases
– during the day – With stress/ fatigue – Acidic/ hot/spicy food
• May be associated with reduced salivary gland
function/altered composition
• May be autonomic involvement
• Behavioral approaches • Topical therapies including anxiolytics, analgesic,
antimicrobials, artificial sweeteners, LLLT
• Systemic therapies
– Antidepressants, aniolytics, anticonvulsants – Antioxidants – Atypical analgesics – Histamine receptor antagonists – Salivary stimulants – Dopamine agonists – Herbal supplements
Clonazepam 1st line treatment
• Mental Nerve Neuropathy • Numbness, paresthesia and rarely pain in
distribution of mental nerve
• Most commonly after dental procedures • LA, implants, RCTs, dental pathology • If no dental cause known considered a red flag • Investigate for systemic malignancy • Other causes MS, bisphosphonates, vagal and
hypoglossal paralysis, leukemic vasculitis
Occlusal Dysesthesia
• Uncomfortable/incorrect bite • Usually plus emotional distress • History of repeated /failed dental procedures • From complex restorative to orthodontic
• Occlusal hyperawareness • SNRI improved symptoms in 5/6 patients
TMDs Radiography
Traumatic TMJ hypoplasia
Adaptational condylar change
Degenerative condylar change
Osseonecrosis/ DJD secondary to
radioation for Pleiomorphic adenoma
Close fracture of condylar neck
Source: http://www.aacfp.com.au/library/AACP%20paperwork.pdf
AM P: SLTOPHO Acknowledgments The content of this booklet was researched and written by Dr. Janet McKeown (MD, CCFP, DipSportsMed), Cristina Sutter (Registered Sport Dietitian) and Susan Boegman (Registered Sport Dietitian) with input from Dr. Penny Miller (Clinical Pharmacologist), Dr. Susan Hollenberg (Family & Travel Medicine Physician), and Dr. Reka Gustafson (Medical Health Officer).
ARIMIDEX® (anastrozole) Tablets The primary endpoint of the trial was disease-free survival (ie, time to occurrence of a distant or local recurrence, or contralateral breast cancer ordeath from any cause). Secondary endpoints of the trial included distant disease-free survival, the incidence of contralateral breast cancer and overall survival. At a median follow-up of 33 months, the combination of ARIMIDEX and tamoxifen did not demonstrate any efficacy benefit when comparedwith tamoxifen in all patients as well as in the hormone receptor positive subpopulation. This treatment arm was discontinued from the trial.