9371_ajceh_november2011.indd
AUSTRALIAN JOURNAL
OF CLINICAL AND
EXPERIMENTAL
HYPNOSIS
VOLUME 39 (2)
Australian Society of Hypnosis
All submissions to the AJCEH are subject to a (blind) peer refereed review process; this
includes expanded research-based analytical reviews of books, but does not include film
reviews or short book reviews, unless otherwise noted. The rejection rate for first submissions
of research-based articles currently runs at about 25%.
Submissions will generally be acknowledged within two weeks of receipt, and feedback
on reviews within four months. The time span for publication of articles can take up to 12
months from date of first receipt, depending on the amount of changes required in the article
and the timing of the submission of the final draft.
The opinions and views expressed in the materials presented in this journal are not necessarily
those of the Editor, Editorial Board and Consultants, or of the Australian Society of Hypnosis.
Each author is responsible for ensuring the authenticity, accuracy, and legality of their
submitted works and to ensure that case studies are written in a way that protects the subjects'
privacy. Where necessary, permission should be obtained for unusual case studies that could
identify a client or research participant. In particular, we ask you to verify your sources and to
ensure that your facts are correct, and that your submissions in no way contain any material
that could be interpreted as libel, defamation, or slander. The AJCEH cannot be responsible
for any complaints arising from the publication of such case studies or articles.
AVAILABLE NOW IN ELECTRONIC FORMAT
Annual Subscription rates 2012
Note that all Australian subscriptions quoted include GST
Australia: Individuals
Institutions and Libraries
Institutions and Libraries
Price per single copy
Individuals $45.00
(including back copies from 1999 to present
Institutions and Libraries
available only as PDFs)
Subscription enquiries to Australian Society of Hypnosis Ltd
Email: [email protected]
PO Box 3009 Willoughby North NSW Australia 2068
AUSTRALIAN JOURNAL OF CLINICAL AND
NOVEMBER 2011
VOLUME 39 (2)
The Treatment of Warts with a Little Help From "The Simpsons": A Case Example of the Treatment of an 11-Year-Old BoyElke Kellis . . . . . . . . . . . . . . . . . . . .
The Use of Hypnosis in The Management of Needle Phobia Charlotte Weigold . . . . . . . . . . . . . . . . . .
Smoking Cessation: A Combined Cognitive Behavioural Therapy and Hypnotherapy Self-Help Treatment Protocol Jillian M. Hely, Graham A. Jamieson, and Debra Dunstan . . . . .
AUSTRALIAN JOURNAL OF
CLINICAL AND EXPERIMENTAL HYPNOSIS
Copyright The Australian Society of Hypnosis Limited 2011
Graham A. Jamieson, PhD, University of New England
Associate Editors
Norm Barling, PhD, Bond University
Amanda Barnier, PhD, University of New South Wales
Greg J. Coman, PhD, University of Melbourne
Allan M. Cyna, MB, Women's and Children's Hospital, Adelaide
June Henry, PhD, Clinical psychologist, Toowoomba
Joseph Barber, PhD, University of Washington School of Medicine
Graham Burrows, AO, KCSJ, MD, FRANZCP, FRCPsych, University of Melbourne
Peter B. Bloom, MD, Pennsylvania Hospital and University of Pennsylvania
Harold B. Crasilneck, PhD, PC, University of Texas
Kevin M. McConkey, PhD, University of Newcastle
Michael Nash, PhD, University of Tennessee
David Oakley, PhD, University College, London
Peter W. Sheehan, PhD, Australian Catholic University, Sydney
David Spiegel, MD, Stanford University
Wendy-Louise Walker, PhD, Sydney
Jeffrey K. Zeig, PhD, The Milton Erickson Foundation
FEDERAL EXECUTIVE OF
THE AUSTRALIAN SOCIETY OF HYPNOSIS LIMITED
President: Gayre Christie, PhD, MBBS, CEP
President-Elect: Jim Fletcher, BA (Hons Psych)
Past President: Brian Allen, BSc, BPsych, FWASMH, MAPS
Federal Treasurer: Ken Jureidini, MBBS, FRACP
Federal Secretary: Hasser Graham, BA (Psych), MAPS
Chair of the Board of Education: James Auld, BDS, MSc, FIDC, FASH
Manuscripts and editorial matter should be addressed to the Editor, Graham Jamieson,
Welcome to Volume 39 (2) of the Australian Journal of Clinical and Experimental Hypnosis. This edition features two valuable clinical case studies by Elke Kellis and by Charlotte Weigold which highlight issues around the suitability of clinical hypnosis for interventions in children and adolescents utilizing the continuity of hypnotic suggestion with the everyday activities of fantasy and imagination. Kellis outlines the sensitive exploration and adaptation of imaginary scenarios for hypnotic suggestion based on a boy's idiosyncratic fantasy involvements and clinical needs to treat his dermatological condition. Of particular interest is the potential for this approach to be adapted to creatively reframing the experience of children undergoing physically and emotionally threatening medical procedures. While the engagement of fantasy is one component commonly utilized in hypnotic interventions, so is the capacity for profound relaxation which Weigold employs as a key element in her treatment of needle phobia in an adolescent girl. Strategically building on her client's available aptitudes and resources, Weigold structures a series of hypnotic sessions around the theme of relaxation paired first with imaginary exposure (in age regression) and then constructing positive response expectancies through age progression. There are many thoughtful issues raised here for those considering the use of hypnosis in behavioural medicine. What makes hypnosis an appropriate modality for treatment for this problem and in this individual? What are the characteristics that would make one consider an alternative approach? What is the role of particular personal attributes and skills of the client (e.g., imagination, relaxation, response expectancies, hypnotizability) in the selection of an intervention approach? How are we to gauge the effectiveness of a chosen intervention as it unfolds and in retrospect? These case studies gently reflect and communicate this thought process in a way that many will find informative.
A large section of this edition is given over to a report of initial clinical
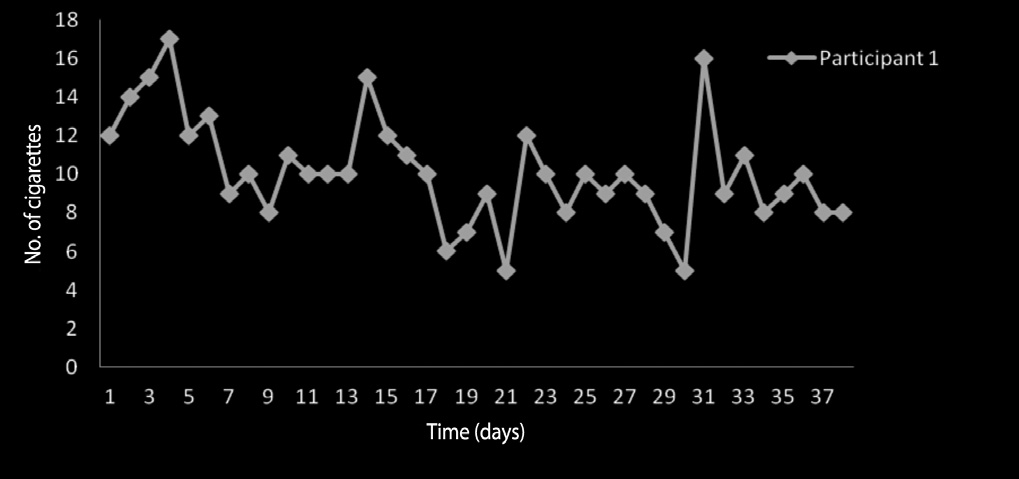
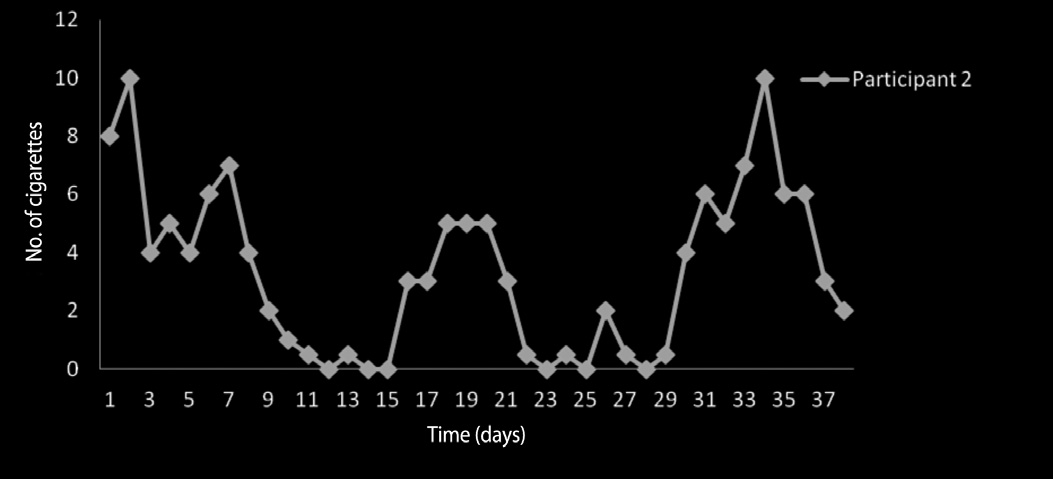
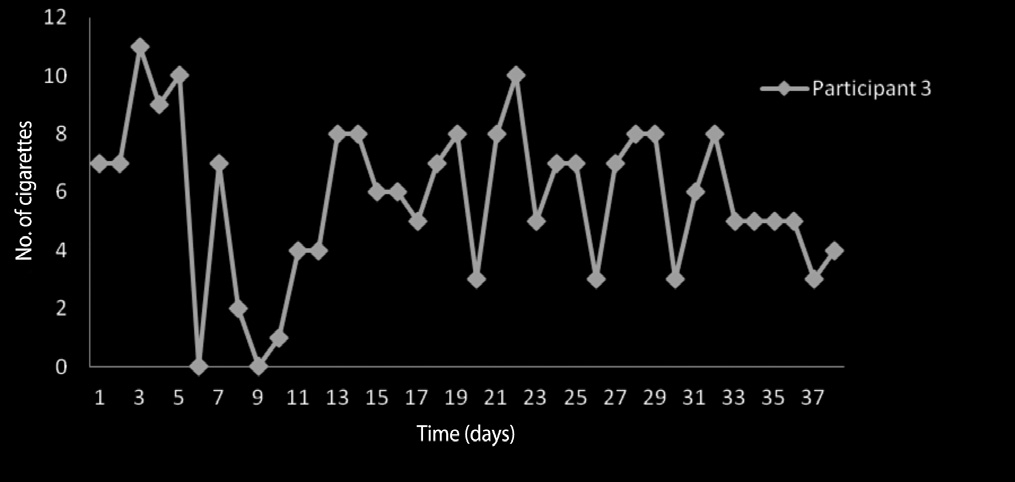
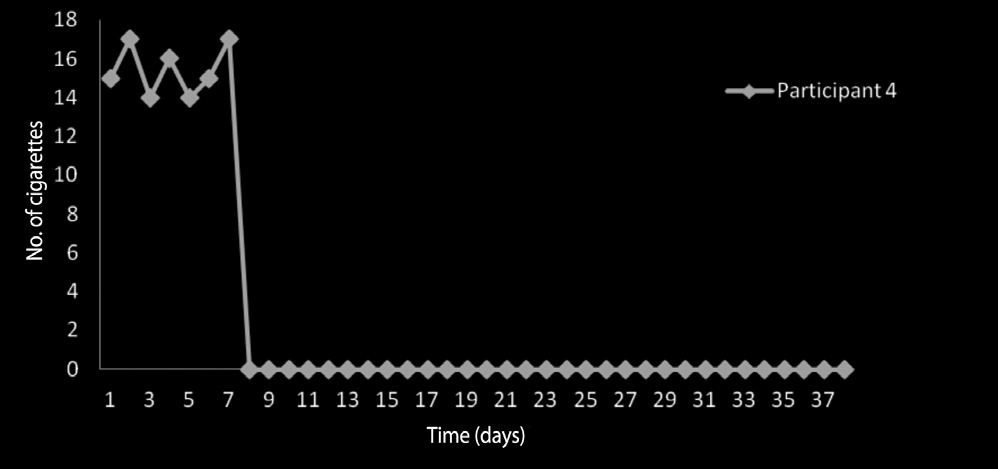
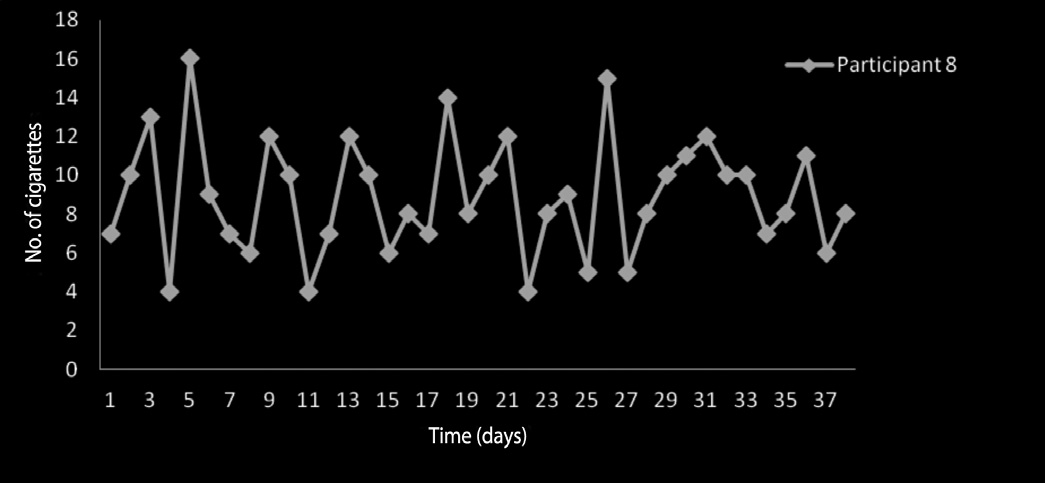
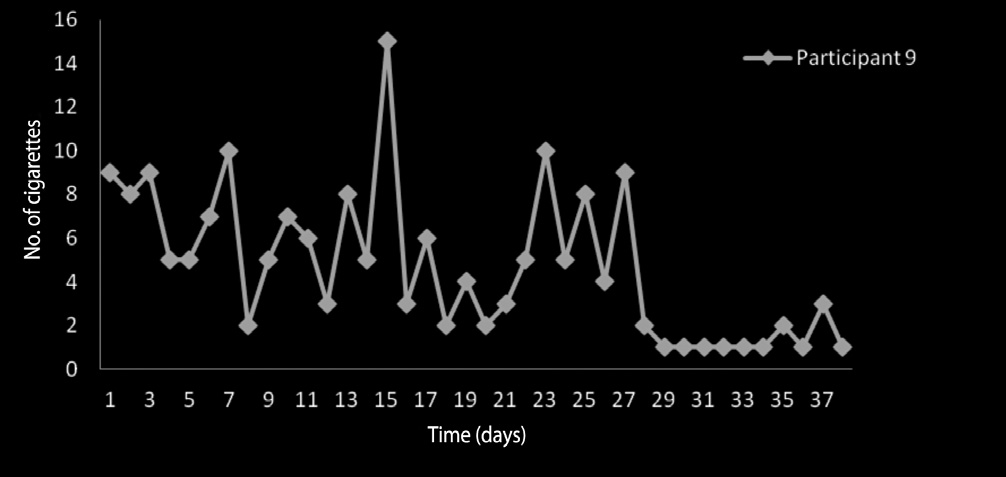
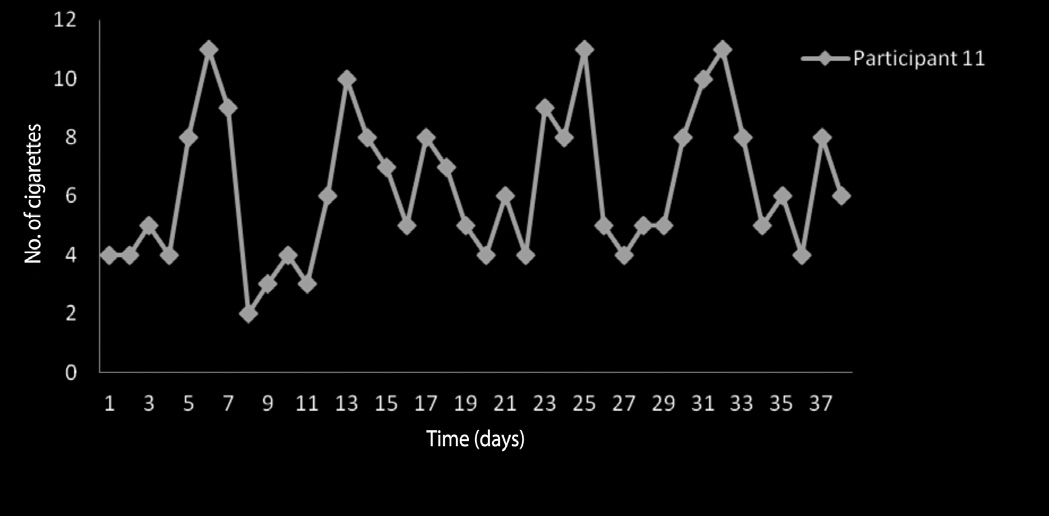
research by Jill Hely and colleagues at the University of New England on a smoking cessation protocol developed by Steve Lynn and Joseph Green seeking to combine hypnosis and cognitive behavioural approaches into a self-help program which can be administered by a range of health professionals (available on request from Joe Green, email: [email protected]). Using the single case time series method which many ASH members will recall from the national conference presentations of Mike Nash and later Amanda Barnier, this preliminary clinical research found direct statistical evidence for
iv Editorial
a reduction in smoking as a consequence of this intervention in three out of seven case studies investigated. Hopefully, randomized control trials will now follow. This study highlights the way in which clinicians working individually or in cooperation may use the single case time series design (see http://www.ClinicalResearcher.org) to make a scientifically valid contribution to the empirical clinical literature. Of further note was the use of a brief phenomenological assessment of hypnotic skills using the Phenomenology of Consciousness Inventory developed by Ron Pekala and colleagues (see http://www.quantifyingconsciousness.com), a brief clinically based hypnotic assessment tool increasingly utilized by North American practitioners.
The future scope and development of the journal is of great importance
to ASH members and indeed to all readers of AJCEH. I ask that together we carefully consider and discuss whom the journal is targeting, both as contributors and readers, what sort of papers we are seeking to publish and why. I believe that in order to continue to attract quality contributions, from national and international contributors, AJCEH must be electronically accessible and thus widely available to be read. My hope is to expand the range of material published and solicited. I therefore invite position papers and discussion papers on all relevant professional and educational matters related to the practice of clinical hypnosis. Contributions to open and ongoing discussions of published papers (and replies by authors) in subsequent editions will be most welcome. In addition, reviews of recently published relevant research in other academic journals and book reviews are actively solicited.
Graham A. Jamieson
Australian Journal of Clinical and Experimental Hypnosis
Vol 39, No. 2, 2011, 181–188
THE TREATMENT OF WARTS WITH A LITTLE HELP
FROM "THE SIMPSONS": A CASE EXAMPLE OF THE
TREATMENT OF AN 11-YEAR-OLD BOY
Registered Psychologist, Melbourne
The following case example illustrates how clinical hypnosis can be highly effective and successful in the treatment of warts in a young boy. The case demonstrates that children can be highly hypnotizable and make excellent subjects for hypnotic interventions. It also highlights that careful preparation is of key importance, particularly in thoroughly educating the subject about warts and how treatment will work as well as in assisting in the selection of useful material to be included in the induction and suggestions stages of the hypnotic interventions. It is argued that a creative application of material generated by the child can greatly facilitate the therapeutic process of the hypnotic intervention. Possible applications of this process in other areas of medicine are also briefly discussed. It is concluded that clinical hypnosis in the treatment of warts in children can be considered a treatment of choice due to its non-invasive and painless nature and effectiveness.
Keywords: paediatric psychology, hypnosis, children, fantasy, warts.
PRESENTING PROBLEM
An 11-year-old boy, Julian, was referred to the practitioner by his mother for
the specific treatment of warts on his feet and hands. These warts had appeared
some time ago and had gradually worsened in terms of number and size.
Julian's warts had not responded to medical and pharmaceutical treatments
and were increasingly painful, particularly when wearing shoes and walking.
Correspondence regarding this paper should be sent to Elke Kellis at [email protected].
182 Kellis
Previous medical treatments had required the grating of dead skin around the warts and subsequent topical administration of ointments and patches. Since previous treatments were unpleasant and cumbersome to administer with no visible relief, Julian and his mother were reluctant to persist with these. Julian's mother had researched alternative forms of treatment and had found out that hypnosis may present a non-invasive and painless alternative to traditional treatments.
Julian presented as a very polite, friendly, and mature boy for his age. He was well groomed and quietly spoken, almost shy, but displayed confidence and curiosity, particularly with respect to hypnosis. Julian had no history of prior psychological, family, or social problems and was very content at school and amongst his friends. He had no other siblings. His medical history included some isolated incidents of asthma related to colds as well as a minor peanut allergy. He had been hospitalized for pneumonia at age three and as a consequence disliked any sort of needles. Following clinical interview with him and his mother, there were found to be no contra-indications for the use of hypnosis in the treatment of Julian's warts. Both his parents consented fully and without reservations to treatment and demonstrated high levels of motivation and a strong belief that the treatment of Julian's warts through clinical hypnosis would be successful. Julian demonstrated creativity and an eagerness to comply, as well as a capacity for vivid imagination and suggestibility.
CONSIDERATION OF THE SUITABILITY OF THE
PATIENT FOR HYPNOTIC PROCEDURES
Children have been found to be excellent candidates for hypnosis (Gardner & Hinton, 1980; Hammond, 1990; Kohen, 1990; Yapko, 2003). It has been argued that children are "typically more easily hypnotizable than adult subjects" as they "generally have very active fantasy lives" (Hammond, 1990, p. 475). A child is not, as yet, restricted by rigid thinking styles that develop with age and maturity, and is wonderfully flexible in responding well to hypnotic suggestions.
Furthermore, hypnosis in the treatment of skin conditions, particularly
warts, has been found to be highly effective (Elton, 1995; Jackson & Merrington, 1980). It has been well established that many skin conditions can
Treatment of Warts in an 11-Year-Old Boy 183
have a considerable emotional component, thus indicating hypnosis as a form of treatment (Crasilneck & Hall, 1990; Elton, 1995). Since previous treatments had been unpleasant and, at times, painful, Julian wanted to avoid these at all costs, thus motivating him to comply fully with hypnotic treatment. Due to a keen interest in hypnosis as well as his high level of motivation, Julian was deemed to be a suitable candidate for hypnosis. His history indicated that there were no contra-indications prohibiting treatment through clinical hypnosis. Julian was found to have good to excellent capacity for suggestibility due to a creative and vivid imagination. He also appeared to have a high degree of positive expectancy and a strong belief that this form of treatment would be successful, in addition to his high level of motivation, which further supported the use of hypnosis in his case (Crasilneck, 1980; McConkey, 1995; Rossi,
Ryan, & Sharp, 1992).
APPLICATION OF HYPNOSIS TO THE PARTICULAR
CONDITION AND THE RATIONALE FOR CHOOSING
THIS APPROACH
Prior to the commencement of the hypnosis session, three important areas of preparation were addressed and attended to. First, there was psycho-education provided to both Julian and his mother about what hypnosis is and how it works in simple language pitched to Julian's educational level in order to explain the process and what would happen as well as answer any questions he may have prior to treatment. This process further assisted in the building of positive expectancy and confidence in both the treatment and the practitioner (Crasilneck, 1980; Gardner & Hinton, 1980; Gerschman, Reade, & Burrows, 1980). Consent for the planned treatment was sought from both Julian and his mother to further engage and build Julian's compliance.
Second, education and information was provided about warts and how
they grow and stay alive in the human body. Special attention was given to the way a wart's root system taps into the body's veins and feeds off the body's blood supply, similarly to a plant tapping into water from the ground. It was explained that a wart needed the body's blood for food to survive and that it would die if prevented from feeding, just as a plant would die if it was starved of water. The example of a clogged straw was also provided to further illustrate this point.
A third and final preparatory step involved asking Julian about his
favourite TV program. The importance of adapting induction procedures and
184 Kellis
suggestions to the age of the child has been highlighted by Hammond (1990), Yapko (2003), and Kohen (1990). Imagining a TV program has previously been suggested as a useful induction technique for children (Hammond, 1990; Gardner & Hinton, 1980). Julian volunteered with excitement that he loved "The Simpsons" TV cartoon show. He was asked to relate features of his favourite episode, which he did with passionate detail. He was asked to share as much detail as possible about the episode as well as the characters of the show in general. These details were then used to form the elements of the hypnotic induction and a vehicle for therapeutic suggestions.
DETAILS OF HYPNOTIC TECHNIQUES AND
INTERVENTIONS USED
As previously highlighted, the hypnosis session was not conducted until after a detailed and thorough preparation of the subject. Only one hypnosis session was conducted with Julian. The script for this session was largely based on material generated through discussion with Julian himself but also utilized a mix of segments from other scripts with special focus on the disappearance of warts (Gibbons, 1990; Tasini & Hackett, 1990) and enhancing well-being (Wilson & Barber, 1990). Following a brief induction, where he was invited to gently allow his eyelids to close and remain in a restful position in addition to allowing his whole body to feel relaxed and light, Julian was invited to picture himself watching his favourite Simpsons episode on a TV screen. After some of the detail of the episode was described in order to assist his imagination and deepen the hypnotic state, Julian was asked to imagine that he had a magic remote which, at the push of a button, would allow him to become part of the episode. He was invited to push the button on the remote and found himself inside the TV as part of the episode which he confirmed through a gentle nod when asked by the practitioner.
In this particular episode, Homer Simpson, a main character in the show,
buys a gun for his protection after a soccer riot. It was suggested to Julian that he visits Dr Nick, another character in the show, with Homer and his gun for help with his warts. Further suggestions encouraged Julian to imagine that Dr Nick filled the gun with special tiny capsules containing a special healing ointment which he then squirted into Julian's mouth, similarly to having a drink from a water pistol. This suggestion was designed to avoid the use of needles which Julian did not like since his time in hospital. It was suggested to Julian that these special capsules would enter Julian's bloodstream and find
Treatment of Warts in an 11-Year-Old Boy 185
where the warts' roots were intruding into the bloodstream and clog up these access points, thus starving the warts of food. It was further suggested that the healing ointment that would make Julian feel healthy and well as well as ensure that no warts would form in future. Julian was told, in accordance with education provided in the preparatory stage of treatment, that the warts would starve, die, and disappear in a week or so.
Julian was then invited to thank and say goodbye to Dr Nick and the rest
of the Simpsons gang and, when ready, push that magic button on his remote again, which would take him back to the consultation room. His hypnosis session was then brought to a comfortable close by re-alerting him to the present surroundings.
GOALS OF THERAPEUTIC INTERVENTION AND
MANAGEMENT
The goal of the hypnotic interventions provided was to treat and eliminate Julian's warts. It was anticipated that a single session of clinical hypnosis would suffice and no additional sessions were scheduled at the time of the original consultation, although it was mentioned that a second session of hypnosis could be conducted if the need should arise.
Julian and his mother were informed that there was no need for a continued
therapeutic management regime or any other form of treatment ,after the hypnosis session as the hypnosis would do its work over the coming days. They were invited to go on with their day-to-day activities and schedule without necessarily paying any particular attention to the warts and that they would receive a follow-up phone call at the end of a week to check in with them and see how treatment had progressed. Julian's mother was encouraged to contact the practitioner immediately if she noticed any adverse reactions or side effects following treatment but was assured that these were unlikely to occur.
It is important to note that all material used in designing the hypnotic
intervention was generated through careful discussion with the child about his favourite TV show as well as details of the intervention applied. Some practitioners and parents may feel concern that a suggestion is given here that involved putting a gun into a child's mouth. It is important to keep in mind that this suggestion was only given after careful consideration and discussion with the child and in a very special context where the child was aware of the special medical nature of the gun and that his motivation was clearly one for healing and painless treatment, not one of reckless endangerment or suicidal tendencies.
186 Kellis
Many medical interventions involve the use of syringes in areas such as
diabetes or pain management through cortisone injections. Other areas, such as treatment of cancer through chemotherapy or radiotherapy, also involve needles for the purpose of anaesthesia and intravenous drug administration, and other medical equipment, such as external beam radiotherapy, MRI or X-ray machines that could lend themselves to the analogy of a ray-gun or squirt gun. This type of intervention can therefore also be applied as an adjunct to medical treatments in this area where medical intervention may be enhanced through hypnotic techniques that can assist the child in the management of applications of needles or anaesthesia, or alternatively in visualizing and deepening the impact of medical interventions using suggestions from the child's favourite TV or book heroes and stories.
The most important aspect here is that any ambiguous suggestion is explored
and discussed to avoid endangering the patient through misinterpretation of a suggestion or its context.
Directly following the hypnosis session, Julian expressed how much he enjoyed the session and, in particular, his adventure with the Simpsons. He reported that it "felt really nice" and presented in a calm and relaxed state.
At the follow-up phone call a week later Julian reported that his warts
were gone. He reported that they had simply shrunk and disappeared. Julian's mother confirmed that the warts had gone and that treatment did not have any negative side effects.
A further phone call was scheduled for six-week follow-up. At this time,
Julian and his mother confirmed that the warts had gone and no further warts had appeared. Both mother and son were extremely satisfied with the treatment outcome and its non-invasive, painless nature.
DISCUSSION AND CONCLUSIONS
Working with this young boy was not only interesting but also fun. It illustrated how well a child can respond to hypnotic interventions due to his capacity to enjoy a vivid imagination and fantasy life. Furthermore, this case demonstrated how important thorough preparation of the subject is, particularly when working with children in the treatment of warts. In the spirit of Milton H. Erickson, it was highlighted how material for healing stories can be directly generated by the client. It was further demonstrated how creative use of this
Treatment of Warts in an 11-Year-Old Boy 187
material together with psycho-educational aspects required in the treatment of warts can allow for the weaving together of both factual and creative material to generate a therapeutic hypnotic intervention.
As a consequence, it can be concluded that hypnotic interventions can form
a highly effective basis for the successful and painless treatment of warts in children without any negative side effects if there are not contra-indications prohibiting the use of hypnosis with the subject. It is argued here that this process, of generating suggestions through preparatory discussions with the child that explore the child's favourite stories and characters, can have wider applications in other areas of medical intervention. The importance of thorough preparation and clarification of potentially ambiguous suggestions is highlighted. In conclusion, it can be argued that the non-invasive and painless nature of clinical hypnosis make this a treatment of choice in the treatment of warts in children.
Crasilneck, H. B. (1980). Clinical assessment and preparation of the patient. In G. D.
Burrows & L. Dennerstein (Eds.), Handbook of hypnosis and psychosomatic medicine (pp. 105–118). Amsterdam: Elsevier/North Holland.
Crasilneck, H. B., & Hall, J. A. (1990). Hypnotic technique for treating warts. In C. D.
Hammond (Ed.), Handbook of hypnotic suggestions and metaphors (pp. 223–224). New York: W. W. Norton.
Elton, D. (1995). Hypnosis in the treatment of dermatological conditions. In G. D.
Burrows & R. Stanley (Eds.), Contemporary international hypnosis: Proceedings of the XIIIth International Congress of Hypnosis, Melbourne, Australia, August 6–12, 1994 (pp. 249–253). New York: Wiley.
Gardner, G. G., & Hinton, R. M. (1980). Hypnosis with children. In G. D. Burrows &
L. Dennerstein (Eds.), Handbook of hypnosis and psychosomatic medicine (pp. 205–231). Amsterdam: Elsevier/North Holland.
Gerschman, J. A., Reade, P. C., & Burrows, G. D. (1980). Hypnosis and dentistry. In G. D.
Burrows & L. Dennerstein (Eds.), Handbook of hypnosis and psychosomatic medicine (pp. 443–449). Amsterdam: Elsevier/North Holland.
Gibbons, D. E. (1990). Suggestions for warts (modeled after Hartland). In C. D. Hammond
(Ed.), Handbook of hypnotic suggestions and metaphors (pp. 224–225). New York: W. W. Norton.
Hammond, D. C. (1990). Hypnotic suggestions with children. In C. D. Hammond (Ed.),
Handbook of hypnotic suggestions and metaphors (pp. 475–477). New York: W. W. Norton.
188 Kellis
Jackson, J. A., & Merrington, H. N. (1980). Hypnosis in family medicine. In G. D. Burrows
& L. Dennerstein (Eds.), Handbook of hypnosis and psychosomatic medicine (pp. 185–204). Amsterdam: Elsevier/North Holland.
Kohen, D. P. (1990). Hypnosis with children. In C. D. Hammond (Ed.), Handbook of hypnotic
suggestions and metaphors (pp. 480–481). New York: W. W. Norton.
McConkey, K. M. (1995). Believing in hypnosis. In G. D. Burrows & R. Stanley (Eds.),
Contemporary international hypnosis: Proceedings of the XIIIth International Congress of Hypnosis, Melbourne, Australia, August 6–12, 1994 (pp. 63–67). New York: Wiley.
Rossi, E. L., Ryan, M. O., & Sharp, F. A. (Eds.). (1992). Healing in hypnosis: The seminars,
workshops, and lectures of Milton H. Erickson: Vol. I. London: Free Association Books.
Tasini, M. F., & Hackett, T. P. (1990). Suggestions for immunodeficient children with warts.
In C. D. Hammond (Ed.), Handbook of hypnotic suggestions and metaphors (p. 226). New York: W. W. Norton.
Wilson, S. C., & Barber, T. X. (1990). An example of positive suggestions for well-being.
In C. D. Hammond (Ed.), Handbook of hypnotic suggestions and metaphors (pp. 112–113). New York: W. W. Norton.
Yapko, M. (2003). Trancework: An introduction to the practice of clinical hypnosis (3rd ed.). New
York: Brunner/Routledge.
Australian Journal of Clinical and Experimental Hypnosis
Vol 39, No. 2, 2011, 189–195
THE USE OF HYPNOSIS IN THE MANAGEMENT
OF NEEDLE PHOBIA
Charlotte Weigold
Hypnosis was used in the management of anxiety for a 15-year-old girl who had developed a fear of needles originating from a negative experience during the first of a series of three school vaccinations. A treatment approach incorporating hypnosis within a cognitive therapy framework was designed and implemented to achieve a successful outcome. Age regression and progression were utilized to acknowledge, harness, and then practise the desired response and post-hypnotic suggestion enabled these lessons to be generalized and applied to other aspects of the client's experience.
Keywords: needle phobia, anxiety, age regression, age progression.
This case-study outlines the use of hypnosis in the management of a client experiencing severe phobia toward needles in the form of injections and/or vaccinations. The case involved a 15-year-old girl who had developed a fear of needles originating from a negative experience during the first of a series of school vaccinations. The client was seeking help to manage the anxiety she felt when she anticipated the subsequent vaccinations necessary to complete the series.
The client, Violet, had originally presented for anxiety a year earlier. This anxiety had surfaced when Violet was under pressure at school and with CBT
Correspondence regarding this paper should be sent to Charlotte Weigold at cha888@bigpond.
net.au.
190 Weigold
and relaxation techniques she was managing well. Violet enjoyed school and spoke confidently about her friends, family, and her schoolwork, although she said that she would like to be more relaxed in some situations.
Violet explained that her school had a vaccination program through which
all students in Violet's year would receive a series of three doses of Gardasil by injection. A few months earlier Violet had received her first dose of Gardasil at school. She described her emotions at the time as slightly apprehensive but not overly anxious about the vaccination. She had noticed on the day that some other girls waiting for their turn were getting very upset; however, as she had not had any bad experiences with vaccinations in the past she was not concerned. The vaccination itself had gone well with Violet experiencing only slight discomfort, but as she left the room and went outside she noticed some girls were now extremely upset. As she attempted to exit the area she began to feel dizzy, and then fainted. It was this experience that upset Violet and she subsequently developed a fear of vaccinations and the needle itself. Violet wanted to manage her fear so that she could successfully receive her remaining vaccinations with her peers as part of the school program, without fainting, embarrassment and anxiety.
Violet had previously displayed a strong ability to relax under instruction
and therefore when she asked for assistance with her fear of needles I decided that she would be a good candidate for hypnosis. This decision was supported by clinical studies conducted by Gow (2006), during which he found evidence that supported the additive effects of hypnosis to therapy to enable patients to receive injections required for medical treatment. Gow has described cases where hypnosis was repeatedly used along with anxiety management techniques to overcome dental needle phobia.
With evidence that hypnosis was an appropriate intervention for the
presenting issue and also an initial judgment that the client was a good candidate for hypnosis, I questioned Violet about things she enjoyed doing and places she found relaxing, that might be useful during such an intervention. She described a beach that she associated with happy and relaxing times and I decided to use that where appropriate.
The goal of therapy was to help Violet manage her anxiety toward needles and a successful outcome would enable her to calmly anticipate and receive her remaining vaccinations at school with her peers. We discussed this goal
Hypnosis in the Management of Needle Phobia 191
and I proposed a treatment approach that would use hypnosis within a cognitive therapy approach to achieve the desired results. Violet was keen to understand more about the hypnosis component of this treatment plan, which prompted me to explain the process using descriptors such as guided relaxation, dissociation, and also the notion of hypnotic suggestion. I invited Violet to describe to me her understanding of hypnosis that I discovered was based largely on "stage hypnosis" seen on television. Together we discussed this common misrepresentation and I explained that hypnosis was not magical and that hypnotic subjects were in control of themselves at all times while in a trance.
Violet confirmed that she was eager to try hypnosis and trusted my ability
to elicit a response from her. Spanos and Barber (1974) claimed that hypnotic performance is actually enhanced by a client's willingness to cooperate with the therapist. However, this alone does not guarantee a successful outcome. Spiegel and Spiegel (2004) maintain that it is important for the client also to have the capacity to experience the hypnotic state and I therefore decided to begin the initial hypnosis session with an arm levitation. Violet responded positively, confirming that she did exhibit the capacity to enter a trance. Her arm levitation also enhanced Violet's confidence in her own hypnotic ability, as well her understanding of hypnosis.
Having established Violet's confidence with using hypnosis, the remainder
of this session was used to explain the cognitive structures that she was using to create and maintain her anxiety. I explained the theory behind the "fight or flight" response and how "faulty alarm systems" can sometimes cause our bodies to react to situations with fear, the result being an elevated pulse and shallow breathing that will eventually lead to feeling faint (as experienced by Violet). I also reinforced Violet's initial positive attitude toward the vaccinations and also her favourable experience during the actual vaccination. This enabled me to separate her fainting reaction from the actual needle and helped Violet to understand that it was the way she was thinking about the experience immediately afterward that had created the symptoms of anxiety that she had since attached to the needle.
It became obvious to Violet that she had associated her fainting with the
needle and had now developed a fear of a repeat of this bad experience. I explained how unlikely it was that she would ever faint again following a needle and that worrying about things that were unlikely to happen wasn't helpful and increased her anxiety. We also discussed how the needle itself did not create the response that she had, that it was actually events following that.
192 Weigold
I asked Violet to consider what we had discussed and return for a hypnosis
session the following week to reinforce these understandings and prepare for the vaccinations that were scheduled that week.
Violet returned for her hypnosis session feeling positive about the outcome.
She explained that she had been thinking about her reaction to the thought of having the vaccination and understood that her anxiety was a response to her thoughts about her reaction rather than any bad experience with the needle itself. However, she was still very concerned that she would react in a similar way following the next vaccination.
I congratulated her on this understanding and I invited her to make herself
comfortable for hypnosis that would reduce this fear and help her manage her anxiety when anticipating the vaccination. I employed a conversational indirect induction based on visual imagery whereby I invited her to visualize herself on a special beach, her beach, and I invited her to imagine a scene of her choosing. I encouraged her to be aware of all her senses which included the smells, sounds, colours, and also the texture and sensation of the wind, sand and water. It's a wonderful feeling lying on the beach without a care in the world, the soft dry sand absorbing the warmth of the sun, listening to the deep breath of the sea breeze, staring out at the glistening water, amazed, relaxed, mesmerized. I described the feeling of weightlessness as she floated in the water and the feeling of being grounded and supported by the sand as she lay on the beach. In turn I observed that her body was motionless and seemed to be supported by the chair, while giving the impression of heaviness, that I presumed to be evidence of catalepsy, and that she had entered a trance-like state.
In order to deepen her trance I described the flow of the waves ebbing in
and out on the sand: and as you hear the sound of the water flowing slowly toward the shore, across the sand, from the depths, sand rising toward the water, water sinking toward the sand, the sound and momentum of the water building as it flows toward its most natural state, the wave, the journey becomes the destination, as the wave peaks and then dissipates across the shore, slowly reaching out toward the sand, and then slowly slipping away, deeper, away from the shore, water floating up and away from the sand, sand sinking away from the water, deeper and deeper, naturally, comfortably with everything exactly as it should be.
I explained to Violet that she was welcome to terminate the session at any
time and to enable her to communicate with me while remaining in trance I established ideomotor responses with her. I asked her to nominate a yes finger and a no finger and informed her that I would check in with her during the session and that she would be able to speak to me or alternatively use these
Hypnosis in the Management of Needle Phobia 193
signals to communicate with me.
I then proceeded with a series of suggestions about learned responses and
how logic dictates that if you can learn responses you should also be able to re-learn or un-learn them and that was exactly what she was there for. I also explained, under hypnosis, how she had negatively hypnotized herself to be fearful of needles and injections and that was powerful knowledge because that meant she also had the ability to positively hypnotize herself. That is, I reframed her capacity to be fearful of needles to an ability to learn comfort with needles. This meant that Violet was able to see her anxiety as something that she was in control of and at the same time feel confidence in her ability to achieve her goal.
My general strategy was to use a combination of age regression and age
progression to help Violet discover how her initial response was learned, then to recreate that event using the knowledge and realizations from the present, and specifically what she had learned in our initial session. Having achieved this, I then asked Violet to travel forward in time and see herself, using this information once again to successfully face the next round of vaccinations in the near future.
It was necessary to take Violet back to the original vaccination, and to the unpleasant event following it when she learned the unwanted response. She was encouraged to view this scene as if on a movie screen. Once she was there (as indicated by ideomotor signals) I asked Violet to let me know how she was feeling as she anticipated and received the vaccination, explaining to her that she would be able to speak easily and remain deeply relaxed as she did. I acknowledged, congratulated and reinforced how well she experienced the vaccination. I asked her to imagine what resources she had used to manage the situation up until this point and to picture these resources as a list on a screen, and to raise her yes finger once she had done this. I then asked her to change the story from this point, and use these resources as well as her newly learned understanding of how she could create her own end to this story, and imagine a more positive response to the vaccinations as she exits the room. In this version Violet was to imagine herself restructuring her thoughts about the experience, and instead of leaving the vaccination room feeling anxious she was to see herself congratulating herself on how calm she is, and how well the vaccination went. She was advised to look around as she left and if
194 Weigold
her peers around her were reacting excitedly she could notice how well she was managing her own levels of anxiety. This would allow her to build more confidence.
Violet was then asked to progress forward to the upcoming vaccination. The age progression was another opportunity for Violet to visualize a positive outcome and to associate this with the event she was previously dreading. I proceeded to lead Violet through the day of the vaccination; anticipating, lining up, receiving and leaving the vaccination area successfully. Throughout this visualization Violet was reminded of her strengths as she imagined herself calmly approaching and undertaking this scenario: and as you float through this experience feeling proud, confident, relieved, empowered, you see the credits roll, signalling the end of the movie, and as they roll you notice that they are actually listing your resources, the same resources that you identified earlier. She was congratulated on her new learned response to the needles and also on the way she understood her body and its reactions to fear: the feeling of empowerment and success spreads through your body, replacing any tension that could have been present with warmth and relaxation, and you realize that this is how your body feels best and that this is the response that you have chosen because it's your choice and you are in control.
Violet was asked to return to the present time, bringing with her the responses she had learned, the resources she had discovered, and the pride and comfort in the knowledge that she had coped so well and managed her fears. It was suggested that she take this feeling and apply it to other aspects in her life where she felt anxious, feeling confident that she had the resources and strength to learn and relearn all that she had to for success. More specifically, it was suggested that Violet would readily recognize when her body was responding in an undesirable way and that she would be able to manage and control these reactions comfortably and confidently in the future.
Violet re-oriented comfortably through an indirect, conversational process:
and I invite you, as you reflect on what you have learned today, as you marvel at what an eye-opening experience this has been, to enjoy the feeling that new and exciting resources have been awakened within you, and it feels like such a deep breath of fresh air, to realize that you had the answers all along, that you just had to wake up and smell the roses, and appreciate what was right before you. As she opened her eyes
Hypnosis in the Management of Needle Phobia 195
we chatted briefly about school and then she left, claiming to feel confident about the upcoming vaccination and promising to let me know how it went.
Violet informed me later that week that the she had attended the vaccinations at school confidently and experienced no adverse reactions. Violet recognized anxious thoughts as they arose and dissipated them with logic and confidence, telling herself that her fears were unfounded and were actually more detrimental than the vaccination itself. She was excited by this result and explained that her ability to visualize herself immediately afterward, leaving the vaccination calmly and confidently, was instrumental to her facing the situation that she had previously dreaded.
Violet presented as a client who could respond well to hypnosis and the nature of her problem was also conducive to this approach. There were only two weeks available to deliver this intervention, which meant that I had to decide whether to spend both sessions on the hypnotic intervention itself or instead to use the first session to embed some cognitive suggestions and create homework as preparation for the actual hypnotic therapy. I decided on the latter, and during the first session I was also able to test Violet's hypnotic capacity. Given this decision and the fact that this left only one session for the actual problem, I was very pleased to discover that this single session was sufficient to create a positive outcome.
I attribute this outcome partly to the therapeutic relationship that I had
already established with Violet and also to her confidence that this hypnotic intervention would be successful.
Gow, M. A. (2006), Hypnosis with a 31-year-old female with dental phobia requiring an
emergency extraction. Contemporary Hypnosis, 23, 83–91.
Spiegel, H., & Spiegel, D. (2004). Trance and treatment: Clinical uses of hypnosis (2nd ed.).
Washington, DC: American Psychiatric Publishing Inc.
Spanos, N. P., & Barber, T. X. (1974). Toward a convergence in hypnosis research. American
Psychologist, 29, 500–511.
Australian Journal of Clinical and Experimental Hypnosis
Vols 39, No. 2, 2011, 196–227
SMOKING CESSATION: A COMBINED COGNITIVE
BEHAVIOURAL THERAPY AND HYPNOTHERAPY
SELF-HELP TREATMENT PROTOCOL
Jillian M. Hely, Graham A. Jamieson, and Debra Dunstan
University of New England, Armidale
Cigarette addiction is a major health issue, with cessation interventions having modest success. Combining interventions may result in improved treatment outcomes. Self-help formats appeal to smokers, but existing protocols have had low success rates. A benchmark comprehensive psychological treatment regime is yet to be established. CBT and hypnosis are possibly efficacious for smoking cessation, alone and in combination. Time-series analysis was used to assess the efficacy of an Australian version of Lynn and Green's combined CBT and hypnotherapeutic treatment protocol in its self-help format in seven smokers over six weeks. Three smokers significantly reduced cigarette intake from baseline, one achieved abstinence. This study provides preliminary evidence supporting the effectiveness of combining CBT and hypnosis in a self-help format for a subset of individuals.
Keywords: smoking cessation, hypnosis, CBT, single case time series.
Nicotine addiction is a major public health issue both in Australia and globally, with 650 million smokers worldwide (Wise & Correia, 2008), half of all smokers dying of a smoking-related illness (Le Foll & George, 2007), and a cost to the Australian public health system estimated at over a billion dollars per year (Collins & Lapsley, 2002). Being a smoker is the biggest risk factor for developing ischaemic heart disease, cerebrovascular disease and lung cancer,
Correspondence regarding this paper should be sent to Graham Jamieson at [email protected].
We would like to acknowledge and sincerely thank Dr Steven Jay Lynn, Dr Joseph P. Green and Dr Tom Brandon for the provision of their treatment protocol for use in this study and suggestions as to study design. Professor Don Hine of the University of New England kindly provided the loan the Vitalograph equipment used in this study.
CBT and Hypnosis Treat Smoking 197
the top three diseases occasioning death in Australia (Department of Health and Ageing [DoHA], 2006). Major disability and morbidity are also faced by smokers in the form of chronic obstructive pulmonary disease (COPD), from which nearly all smokers of 20 or more cigarettes per day suffer to some degree, as well as from a range of other serious illnesses (USDHHS, 1984).
Smoking is an addictive behaviour classified as a substance dependence
disorder; the latter is defined in the Diagnostic and Statistical Manual IV, Text Revision (DSM-IV-TR; 2000) as a clinically significant impairment indicated by three or more of the following criteria: tolerance, withdrawal, higher consumption than intended, desire or failing efforts to control use, excessive time spent in substance-related activities, reduction in other activities due to substance use, and use of the substance despite knowledge of suffering from health problems occasioned by the substance use. Substance dependence disorders are notoriously obstinate to treat and run a chronic course (DSM-IV-TR, 2000; O'Brien & McLellan, 1996). Of all substance dependence disorders, nicotine addiction has the lowest treatment success rate, with only 20–30% successfully abstinent at 12 months when treated in a specialized clinic, compared to 50% of those treated for alcohol dependence and 60% of those treated for opiate dependence in similar clinics (O'Brien & McLellan, 1996). Although 80% of smokers report a desire to quit smoking in any one year, only 5% succeed without treatment (DSM-IV-TR, 2000). Smokers, however, are useful in the study of addictions due to the fact that neural mechanisms found to be involved in nicotine addiction have also been implicated in other addictions (Wonnacott, Sidhpura, & Balfour, 2005), suggesting that nicotine addiction operates in a similar way, and as such, treatment methodologies may be usefully cross applied.
Success at smoking cessation has been found to be related to a number
of variables. Social support from family and friends in regard to quitting has been found to be related to success (Lawhon, Humfleet, Hall, Reus, & Munoz, 2009). However, Alemi, Stead, White, and Barnes (2003) have posited a role theory of social support, which suggests that there may be either a positive or a negative effect on addictive behaviours dependent upon the type of social support one may have. Gender differences have been found in smoking cessation rates, with fewer women successfully quitting smoking than men (Wetter et al., 1999). Depression appears to be higher amongst smokers than the general public, and lower cessation rates have been found for depressed than for non-depressed smokers (Hitsman, Borrelli, McChargue, Spring, & Niaura, 2003). Many smokers cite putting on weight as a disincentive to quit
198 Hely, Jamieson, and Dunstan
smoking, and poor body image has been found to be related to decreased cessation rates (Klesges, Meyers, Klesges, & LaVasque, 1989). Higher levels of nicotine dependence have been found to be related to lower cessation rates (Fagerstrom & Schnieder, 1989; Hyland et al., 2006). A higher number of previous quit attempts has been found to be predictive of successful smoking cessation (Rigotti, 2009). Motivation to quit has also been found to be related to successful cessation (Crittenden, Manfredi, Warnecke, Ik Cho, & Parsons, 1998).
Non-pharmacological techniques for quitting smoking include both clinical
hypnotherapy and cognitive behavioural therapy (CBT). CBT may be defined as a range of treatments which aim to change the cognitions and behaviours related to a disorder or problem with psychological components (Spiegler & Guevremont, 2003), and is based to a large extent on learning theory. CBT intervention for smoking cessation involves utilizing techniques such as stimulus control, positive reinforcement, competing behaviours, assertiveness training and cognitive restructuring, as well as relaxation procedures to provide an alternative response to stress. Hypnosis is widely believed to involve the induction of "an altered state of consciousness in which a person is able to bypass certain aspects of reality, tolerate logical inconsistency, experience distortions of perception and memory as real, and feel a compulsion to follow cues from an outside source" (Covino & Bottari, 2001, p. 340). Clinical hypnotherapy for smoking cessation involves the induction of such a state by the use of relaxation, suggestion and visualization, with therapeutic suggestions and imagined experiences administered while the individual is in the state of hypnosis. These may include suggestions which reinforce the health benefits of quitting smoking, change the individual's cognitions regarding smoking, and improve their ability to deal with nicotine cravings.
Psychological interventions for smoking cessation may be classified as
minimal, intensive, or self-help interventions. Minimal assistance includes issuing advice to quit, the provision of written information, and advice on available therapies (Zwar et al., n.d.). Minimal assistance has been found to result in two- to three-fold increases in smoking cessation rates (Janz et al., 1987). Intensive assistance involves the provision of multiple one-to-one sessions, each usually lasting an hour or so. Self-help interventions provide detailed guidance, materials and instruction based on a particular intervention program to be implemented by the individual. Although success at quitting smoking increases with the intensity of the behavioural intervention (Fiore et al., 2000, as cited in Elkins, Marcus, Bates, Rajab, & Cook, 2006), it has been
CBT and Hypnosis Treat Smoking 199
acknowledged that smokers are unlikely to seek treatment in intensive therapy, with a preference for less demanding treatment strategies (Brandon, 2001; Janz et al., 1987). As such, health-care-practitioner based minimal assistance and self-help modes of intervention appear to be more agreeable to smokers considering quitting. Self-help treatments have been found to have a significant but small effect upon smoking cessation in a Cochrane Review of 68 trials, with improvements of just 1% compared to control groups (Lancaster & Stead, 2005). As such the potential benefits of being more agreeable to smokers must be weighed up with the cost of having a small success rate compared to other levels of intensity of psychological treatments.
Despite similar success rates of some psychological treatments to
pharmacological treatments, research into psychological interventions for smoking cessation has waned somewhat since the advent of pharmacotherapies, potentially as a result of the high levels of funding available by drug companies in order to build a body of evidence for such treatments (Brandon, 2001). It is difficult for research into behavioural interventions for smoking cessation to meet the research standards that pharmacotherapies have established due, in part, to funding constraints. Research into pharmacotherapies is also less prone to methodological difficulties than is research into behavioural therapies, such as difficulty arriving at a suitable placebo, and measurement of the "active ingredient" (Hajek, 1996, p. 704) in terms of both how much of the treatment is necessary for success and in terms of separating the effect of this ingredient from the effect of other factors such as therapist attention (Hajek, 1996). As such, continued investigation into psychological therapies for smoking cessation remains warranted, despite the apparent dominance of, and large body of evidence for, pharmacotherapies.
Randomized controlled trials (RCTs), involving comparisons between
two groups of participants randomized to the control group or the treatment group, are the dominant paradigm in psychological research as well as pharmacological research. This is due to the fact that they are able to effectively determine the efficacy of certain treatments, unlike clinical anecdotes and group designs with low participant numbers, which have been criticized for being insufficiently rigorous to provide evidence that the independent variable has had any effect upon the dependent variable. However, further design and analysis techniques have been developed based on studying individual change over time that surpass original case study methods. Time-series designs are able to validly provide information regarding possible treatment efficacy by comparing individual results in a baseline and treatment phase, with each
200 Hely, Jamieson, and Dunstan
participant's baseline serving as their own control. It has been argued that time-series designs are sufficiently rigorous to stand beside group designs (Barlow & Hersen, 1984; Bergin & Strupp, 1970; Kazdin, 1982, 1992, as cited in Borckardt et al., 2008), and they have recently been recognized by the American Psychological Association as an important method for assessing treatment efficacy (Chambless & Ollendick, 2001, as cited in Borckardt et al., 2008). Time-series designs also offer substantial benefits over other designs, particularly for clinical practitioners, in being able to draw useful inferences about treatments from small populations. They are also useful in displaying detailed information about the process of individual change in response to intervention – information which is lost in RCTs – and in conducting valid preliminary clinical research which may form the justification for large-scale RCTs.
Hypnotherapy is a popular method used by those seeking assistance to quit
smoking, even with the increasing emphasis on pharmacotherapies. It has a lengthy history in the treatment of addiction, dating back to the nineteenth century when it was reportedly used successfully to treat alcoholism in a large number of individuals (Martensen, 1997, as cited in Potter, 2004). Ongoing controversy has surrounded the phenomenon of hypnosis throughout the history of its use. Debate has continued as to whether it is a genuine phenomenon or simply the result of demand characteristics plus the trait of suggestibility in the participant (Wagstaff, 1991, as cited in Eysenck, 2004). Kirsch (1999) has posited a response-expectancy account of hypnosis, which states that the effect of hypnosis is primarily a result of the individual's belief in hypnosis. However, recent neuro-imaging studies (Egner, Jamieson, & Gruzelier, 2005; Faymonville et al., 2003; Raij, Numminen, Narvanen, Hiltunen, & Hari, 2005; Rainville, Duncan, Price, Carrier, & Bushnell, 1997) suggest that hypnosis does in fact create specific and unique changes to information processing in the brain, supporting the view that hypnosis engages a neuropsychological state distinct from alert waking consciousness. It is important to note, however, that the core mechanisms in either account by no means exclude those of the other (Lynn & Green, 2011).
Despite the popularity of hypnotherapy for smoking cessation, there
is little consensus as to its efficacy. A Cochrane Review of hypnotherapy for smoking cessation (Abbot, Stead, White, & Barnes, 1998) concluded that existing evidence was insufficient to recommend it as a treatment for nicotine addiction. This conclusion was based on the fact that few studies met the methodological requirements of being RCTs with a six-month
CBT and Hypnosis Treat Smoking 201
follow-up necessary to be included in the meta-analysis. The studies that were included had heterogeneous results, with quit rates varying from 4% to 88% at six months. This may be accounted for somewhat by the variety of hypnotherapeutic interventions used, both in terms of suggestive content and level of assistance. Heterogeneity of results may have also been influenced by the methodological flaws of some studies included, such as only half the people randomly assigned to the hypnosis treatment group actually receiving the hypnotic intervention in one trial of 180 participants (Lambe, Osier, & Franks, 1986, cited in Abbot, Stead, White, & Barnes, 1998). This may be viewed as having skewed the results of both this study and the meta-analysis.
Since the publication of the Cochrane Review of hypnotherapy for
smoking cessation (Abbot et al., 1998) however, a number of further studies have been performed. Elkins et al. (2006) randomly assigned 20 participants to eight weekly individual sessions of hypnotherapy or to a wait list control group in a preliminary trial of intensive clinical hypnosis. During their first session, those in the hypnosis group received information regarding hypnotic procedures and misconceptions about hypnosis, standard smoking cessation self-help material from the National Cancer Institute (Glynn & Manley, 1990, as cited in Elkins et al., 2006) as well as a 30 minute counselling session involving readiness to change, dealing with trigger situations and setting a quit date. They were then provided with a taped copy of a hypnotic intervention to listen to between then and their quit date on a daily basis. During the eight weekly hypnosis sessions, hypnotic suggestions were administered as follows: an eye-focus induction, relaxation, comfort, calming mental imagery, commitment to quitting, dissociation from craving, post-hypnotic suggestions, instructions to practise self-hypnosis, and positive imagery regarding not smoking (Elkins et al., 2006). Six out of 10 participants in the hypnosis group were abstinent from cigarettes at 12 weeks and 4 out of 10 at 26 weeks, based on self-report verified by expired carbon monoxide concentration of 8 ppm or less.
Carmody et al. (2008) conducted a randomized controlled trial with 286
participants assigned to either two hour-long hypnosis sessions or two hour-long counselling sessions, both in combination with nicotine patches. The hypnotic intervention included suggestions and guided imagery to promote "relaxation, commitment to quitting, self-image as a non-smoker, ability to resist the urge to smoke, mood management, and development of a healthy lifestyle" (Carmody et al., 2008, p. 813). These were based on techniques developed by Spiegel (1994, as cited in Carmody et al., 2008), Lynn et
202 Hely, Jamieson, and Dunstan
al. (1993 as cited in Carmody et al., 2008), Green (1996, 1999 as cited in Carmody et al., 2008) and Gorassini and Spanos (1986 as cited in Carmody et al., 2008). Taped copies of the intervention were also provided in order for participants to practise entering into hypnosis on their own and to assist in maintaining the effects of the intervention via the participants being able to review the hypnosis treatment at a later date. Additional support was provided to those in the counselling group in the form of three 20 minute follow-up calls. Carmody et al. (2008) found that 26% of the hypnosis group were abstinent at six months, compared to 18% in the counselling group, and that 24% of the hypnosis group were abstinent at 12 months compared to 16% in the counselling group. The abstinence rates for the hypnosis group compare favourably with those of nicotine replacement therapy alone of 17% at six months or longer (Silagy, Lancaster, Stead, Mant, & Fowley, 2007), as well as with the abstinence rates for varenicline of 23% and for bupropion of 14.6% between weeks 9 and 52 (Jorenby et al., 1999). Furthermore, those with a history of depression had greater quit rates than those without a history of depression in the hypnosis group, whereas this relationship was reversed in the counselling group. This suggests that hypnosis may offer incremental benefits over other treatments for those suffering from depression, for whom treatment with varenicline or bupropion is sometimes contraindicated due to potential exacerbation of depressive symptoms and risk of suicidal ideation in people diagnosed with mood disorders (US Food and Drug Administration [USFDA], 2009).
Recent meta-analysis by Green, Lynn, and Montgomery (2008) of 24
studies and a total of 5,704 participants, which used a variety of different study designs and follow-up rates to assess the impact of clinical hypnosis on quitting smoking, found an overall smoking cessation rate of 26.3% at follow-up. Like other interventions for smoking cessation (Fiore et al., 1994; Wetter et al., 1994, as cited in Green et al., 2008), females were less successful at achieving abstinence, with 23.4% of females and 30.6% of males successfully quitting smoking at follow-up. Success at achieving smoking abstinence correlated positively with the intensity of the treatment in terms of hours of clinical hypnosis received. The results of the meta-analysis suggest that hypnosis may be considered a possibly efficacious treatment for smoking cessation and that further exploration of the intervention is warranted (Green et al., 2008).
Clinical hypnotherapy has been examined by a number of studies as to
whether treatment effect is related to scores on measures of hypnotizability. Studies have had varying results as to the predictive validity of hypnotizability
CBT and Hypnosis Treat Smoking 203
when assessed using clinical hypnosis for a range of conditions, for example, pain, with positive findings by some (Spinhoven & ter Kuile, 2000) and null findings by others (Goran, 1991), as well as positive correlations between hypnotizability and reduction of asthma symptoms (Ewer & Stewart, 1986) and anxiety (Delmonte, 1985). Schubert (1983) also found a significant relationship between hypnotizability and reduction in cigarette smoking following clinical hypnosis. Lynn and Kirsch (2006) pointed out that in no studies was there a negative relationship between hypnotic susceptibility and treatment gains. Due to the inconsistency of findings on the usefulness of hypnotizability in predicting treatment effects, further studies are warranted in order to examine the utility of assessing hypnotizability in clinical hypnotherapy.
CBT for smoking cessation has also been used successfully in a number
of trials. A randomized controlled trial by Sykes and Marks (2001) of 260 smokers in a lower socioeconomic area used a treatment involving a combination of 30 CBT methods in a self-help format including handbook, audiotape, and progress chart. One in four participants in the CBT group had quit or significantly reduced their cigarette intake at six months, compared with 1 in 18 in the control group. A Cochrane Review of 53 studies of group behaviour therapy (Stead & Lancaster, 2009) concluded that behavioural programs do produce increased quit rates. Behavioural treatments are now widely accepted elements of programs for smoking cessation (Covino & Bottari, 2001), with integration into many self-help formats such as the Quit Pack issued free by NSW Health (2007). Support from such services as the Quitline is also routinely recommended by general practitioners in Australia when commencing pharmacological treatments.
Multimodal treatment has been found to have incremental benefits over
using one treatment method at a time when combining pharmacotherapies such as bupropion and NRT (Jorenby et al., 1999) or NRT and behavioural treatment (Buchkremer & Minneker, 1989; Hegaard, Kjaergaard, Moller, Wachmann, & Ottensen, 2003; Reus & Smith, 2008). Carmody et al. (2008) found increased cessation rates when combining hypnosis with NRT. Telephone counselling in combination with minimal interventions, such as doctor's advice to quit, has been found in a meta-analysis of 22 studies to result in incremental increases in quit rates (Pan, 2006). Few studies, however, have assessed the benefits of a multimodal program for smoking cessation based on a combination of solely psychological approaches. It has, however, been demonstrated that adding hypnosis to CBT can improve treatment effects for some conditions such as anxiety (Schoenberger, Kirsch, Gearan,
204 Hely, Jamieson, and Dunstan
Montgomery, & Pastyrnak, 1997, as cited in Kane & Reinecke, 2006), and obesity (Bolocofsky, Spinler, & Coulthard-Morris, 1985, as cited in Kane & Reinecke, 2006). One previous study has also found that a combination of CBT and hypnotherapy for smoking cessation resulted in quit rates of 31% at three months (Jeffrey, Jeffrey, Greuling, & Gentry, 1985, as cited in Kane & Reinecke, 2006). A meta-analysis by Kirsch et al. (1995, as cited in Kane & Reinecke, 2006) of 18 studies found a mean effect size that was significantly greater for combined CBT–hypnotherapy treatments for a range of conditions than CBT treatments alone.
It has been suggested that hypnosis may operate not just as an addition to
CBT in order to increase treatment effect, but may make the CBT itself more effective by increasing the focus upon, and acceptance of, suggestions which aim to change smoking-related cognitions (Kane & Reinecke, 2006). As such, it is hoped that incremental improvements in cessation rates can be made by combining cognitive behavioural and hypnotherapeutic techniques which improve the effectiveness of CBT. A comprehensive non-pharmacological program may also provide the best treatment option for those for whom pharmacological approaches are sometimes contraindicated, such as pregnant women, people with mood disorders, or those who have suffered significant side effects from previous pharmacologically assisted attempts to quit. Such an approach, when presented in a self-help format for increased appeal to smokers, may result in an effective treatment for smoking cessation. It is time for a cutting edge, well-researched program to provide a benchmark non-pharmacological treatment protocol in order for barriers regarding variations in hypnotic interventions to be resolved and research into this area to progress. Using a self-help format also provides a standardized treatment to all participants and reduces confounding variables such as client–therapist rapport.
Lynn, Green, and Brandon (2009) have been in the process of refining a
two session group smoking cessation program incorporating both CBT and hypnosis components, which includes education regarding the health effects of nicotine dependence and withdrawal, identifying and managing triggers, as well as teaching cognitive and behavioural responses to cravings and relapse prevention strategies. It also includes education regarding hypnosis as well as a hypnotic intervention including smoking cessation related suggestions aimed at increasing confidence, self-efficacy, positive self-image and ability to manage stress in order to quit smoking (Lynn et al., 2009). This program has been delivered in a group format (Lynn & Kirsch, 2006) and has also been formatted
CBT and Hypnosis Treat Smoking 205
as a self-help program in the form of CDs and DVDs. The hypnotherapeutic element of this program was the basis for the hypnosis treatment condition in the Carmody et al. (2008) study, as cited above, which provides evidence for the efficacy of the program's hypnosis component. As yet, studies have yet to be completed which support the efficacy of the combined treatment in its self-help format. However, an earlier revision of the group program achieved six-month abstinence rates of between 24% and 39%, varying between trainers (Lynn & Kirsch, 2006). It is reasonable to expect that the self-help format of the treatment protocol is also likely to be of significant benefit to those who wish to stop smoking.
In view of evidence supporting both clinical hypnosis and CBT for
smoking cessation, it appears that hypnosis and CBT are both, indeed, effective treatments to assist people in smoking cessation. There is also evidence to support that combined CBT and hypnosis treatments improve response rates. Furthermore, there is sufficient evidence to assume that smoking cessation programs presented in a self-help format are also of benefit to some smokers wishing to quit, although resulting in less impressive quit rates than intensive in-person therapies. One may assume, therefore, that a smoking cessation program incorporating both hypnotherapeutic techniques and CBT presented in a self-help format is also likely to be of assistance to those who wish to quit smoking. As such, it is hypothesized that a combined hypnosis and CBT self-help treatment protocol will result in a significant decrease in cigarette consumption from the baseline phase of the study to the intervention phase of the study in regular smokers. This study aims to provide preliminary evidence in support of a hypnotherapy and CBT treatment protocol based closely on Lynn at al.'s (2009) protocol in its self-help format. Therefore the following hypothesis is posited: Mean cigarette consumption per day will be higher in the baseline phase than in the intervention phase consisting of use of the self-help CBT and hypnosis materials.
Recruitment was conducted by placing information sheets for potential participants in the waiting rooms of health professionals, as well as directly approaching smokers in the central business district of a regional city in New South Wales, Australia. Potential participants were provided with an
206 Hely, Jamieson, and Dunstan
information sheet regarding the details of the study in order for informed consent to be gained. Eleven members of the general public volunteered to participate, including four males and seven females. Participants were between the ages of 18 and 43 with a mean age of 34 years, and all were determined to have a degree of dependence on nicotine as determined by the Fagerstrom Test for Nicotine Dependence (Heatherton, Kozlowski, Frecker, & Fagerstrom, 1991). Two participants dropped out of the study prior to commencing the intervention phase. Two further participants did not complete the intervention diary. Prior to recruitment, approval to perform this study was granted by the University of New England Human Research Ethics Committee. Anonymity of participants was ensured by assigning each participant with a participant number at the commencement of testing, with contact details kept in a separate document. Informed consent was gained via first providing each participant with an information sheet detailing the nature of the study. Those who indicated that they suffered from a psychotic illness were excluded from the study due to uncertainty in the use of hypnosis for such conditions.
A demographic questionnaire was distributed to participants, including items regarding age, gender, education level, occupation, medical and psychiatric diagnoses, number of cigarettes per day, years as a smoker, number of previous attempts to quit smoking, previous interventions for smoking cessation used, and a Likert-type rating scale item on body image.
Along with the demographic questionnaire, the Fagerstrom Test for Nicotine
Dependence (FTND; Heatherton et al., 1994), a popular public-domain six-item self-report test which correlates reasonably well with physiological measures of nicotine dependence (r = .39) as well as number of years smoked (r = .57) and shows good test-retest reliability (Pomerleau, Carton, Lutzke, Flessland, & Pomerleau, 1994), was administered. The Depression Anxiety Stress Scale Short Form (DASS-21; Lovibond & Lovibond, 1995), another public domain test comprised of 21 items with scoring of the three subscales of depression, anxiety and stress based on normative data from the Australian population, was also administered. The DASS-21 has been found to have good construct validity when compared with similar measures such as the Positive and Negative Affect Schedule (PANAS; Henry & Crawford, 2005; Watson, Clark, & Tellegen, 1988) and is able to reliably assess the three factors of depression, anxiety and stress in large samples (Crawford & Henry, 2003).
CBT and Hypnosis Treat Smoking 207
Also included was the Multidimensional Scale of Perceived Social Support (MSPSS; Zimet, Dahlem, Zimet, & Farley, 1988). The MSPSS is a widely used test of the construct of social support which has been used in a broad variety of populations, and has internal reliability coefficients of .90 and above between the three subscales of family, friends and significant others (Dahlem, Zimet & Walker, 2006).
The Phenomenology of Consciousness Inventory – Hypnotic Assessment
Procedure (PCI-HAP; Pekala, Kumar, & Maurer, 2005) was used in order to gain information about participants' level of hypnotic responsiveness as well as their expectations about hypnosis. It was also included in order to familiarize participants with the process and experience of hypnosis prior to providing any clinical intervention, as it has been found that first-hand experience of hypnosis reduces negative attitudes and incorrect assumptions about hypnosis (Green, 2003, as cited in Lynn et al., 2009). The PCI-HAP includes a pre-assessment questionnaire (PCI-HAP Pre-Assessment) regarding participant's expectations about the experience of hypnosis, as well as a brief standardized hypnotic induction procedure script (HAP Induction Procedure) involving relaxation, visualization, and suggestion, a Post-Induction Debriefing Form, and the Phenomenology of Consciousness Inventory (PCI). The PCI is a 53-item questionnaire with items regarding the experiences participants may have had during the hypnotic induction procedure rated on a 7 point Likert-type rating scale. The Hypnoidal State Score that the PCI-HAP provides correlates highly with the Harvard Group Scale of Hypnotic Susceptibility at .60, as well as being found to have good convergent and discriminant validity (Forbes & Pekala, 1993; Pekala & Kumar, 1984, 1987, 2007; Pekala, Kumar, Maurer, Elliott-Carter, & Moon, 2006).
In order to obtain a biochemical measure of cigarette consumption, a measure of each participant's alveolar carbon monoxide (CO) level was obtained using a Vitalograph BreathCO model 2900, which detects parts per million (ppm) of carboxyhaemoglobin (COHb) exhaled in an individual's breath.
Diary number one (Baseline Diary) included one double page for each
day over a one week period, asking participants to record a tally of the number of cigarettes smoked per day as well as the specific antecedent occurrences and thoughts of two cigarettes per day, in order to capture some of the triggers involved in the participant's smoking behaviour. Diary
208 Hely, Jamieson, and Dunstan
number two (Intervention Diary) also had space for participants to record a tally of cigarettes per day over a six-week period, as well as antecedents of smoking as described above. The Intervention Diary also included pages in which to complete exercises as detailed in the CBT CD-ROM. Diaries were designed to be the approximate size of a cigarette packet so that they could be stored with cigarettes and readily accessed while smoking. CD-ROMs were distributed containing an audio and PowerPoint presentation of a local version of Lynn and Green's most recent revision of their Self Empowerment Programme for Smoking Cessation (2009) recorded with an Australian voice. Materials for clinicians and researchers wishing to use the Self Empowerment Programme for Smoking Cessation are available from co-author Dr Joseph Green of Ohio State University (email: [email protected]).
This contained an educational component of information regarding
the detrimental effects of smoking, how smoking is a learnt behaviour that needs to be unlearnt, and strategies to assist participants enlist known factors in successful smoking cessation such as social support, formal intervention, motivation, self-efficacy, and dietary adjustments. It also contained instructions for CBT exercises including listing reasons to quit, visualizing success, identifying triggers, stimulus control, stress and urge management, and relapse prevention. The CD-ROM also had a hypnosis track at the end, with relaxation, visualization and anchoring instructions, where participants were instructed to remember a positive life event where they showed good coping skills, and anchor this to a thumb-and-finger touch gesture in order to summon the memory and positive feelings associated with it whenever necessary to cope with cravings and stress. A CD with the hypnotic intervention was also distributed. This included relaxation instructions, formulation of a key phrase regarding quitting smoking to be used later, imagining writing out reasons to stop smoking, visualization of one's proud non-smoking self, visualization of successfully resisting the urge to smoke around others, regression to the negative reasons one started smoking and recognition of the fact that those reasons are no longer in operation, and remaining calm while observing the urge to smoke fade and vanish.
During the initial session, which was held either individually or in pairs of people who knew each other, according to the participants' preferences, participants were asked to complete demographic questionnaires, the FTND
CBT and Hypnosis Treat Smoking 209
and the DASS as outlined above. Participants then were asked to give a carbon monoxide reading by taking a deep breath, holding their breath while the researcher counted to 10, and then breathing out slowly into the BreathCO device while the researcher counted to 20. The researcher then asked the participant to complete the PCI-HAP Pre-Assessment. Participants were next asked to make themselves comfortable in a high backed chair, and the researcher read the hypnosis script provided in the PCI-HAP in a suitably calm and modulated voice. Following the hypnotic procedure, participants completed the PCI-HAP Post-Induction Debriefing Form and the PCI. At the conclusion of the initial session, participants were provided with a diary and requested to keep this diary for one week, by adding to a daily tally of their cigarette consumption each time they had a cigarette, as well as record the details of two cigarettes per day, one in the morning and one in the afternoon or evening, in order to capture smoking-related thoughts and antecedents.
After week 1 (baseline), diary number one was collected and participants
were provided with the CBT CD-ROM and Hypnosis CD, along with written instructions regarding the use of the CD-ROM, CD and Intervention Diary. Participants were asked to specify a date in the near future when they planned to cease smoking and instructed to view the CD-ROM on that day. This date signified the commencement of week 2, and the beginning of the intervention phase. They were advised to complete the exercises contained within the CBT CD-ROM presentation as well as listen to the hypnosis track at the end of the presentation on their quit date. Participants were requested to listen to the hypnosis CD on the day following their specified quit date, and to continue to listen to the CD on a daily basis for at least the next week. A second diary was also provided in which to complete exercises on the CD-ROM and to continue to record their smoking thoughts and behaviours. Diaries continued from week 2 until week 6.
Following week 6, all diaries were collected. At this time participants again
provided a reading of their CO concentration using the BreathCO device and procedure, in order to validate their self-report of whether their attempt at smoking cessation was successful or not.
Study Design and Analysis
A time-series design was utilized in order to examine both success in smoking reduction and the mechanisms of change in each participant, by assessing whether initializing the intervention phase had an effect on the mean number
210 Hely, Jamieson, and Dunstan
of cigarettes consumed per day for each participant when compared to their baseline phase. Time-series designs are an effective way of evaluating data derived from clinical interventions performed with single cases or a small number of participants. Time-series analysis may be conducted utilizing a range of statistical methods such as simulation modelling analysis (SMA) or similar techniques, in order to address the phenomenon of data autocorrelation and ensure that the assumption of independence of observations is met. Significance testing is then able to be performed once this has been addressed, with a reduced risk of type I error.
Participants commenced baseline measures and treatment intervention
at varying times over a four-month period in a non-concurrent multiple baseline design across subjects, in order to provide some degree of control for potential history effects, such as those which may have occurred as a result of changes to the cost of cigarettes or further restrictions to smoking areas. In order to address the autocorrelation of the time-series data the dependence of one data-point upon another in having come from one individual over time, which violates the assumption of independence and leads to an unacceptably high chance of type I error, SMA was conducted using Simulation Modeling Analysis for Windows Version 8.3.3 prior to significance testing. A regularly updated version of this software is freely available for readers to download from the ‘Software' page at http://www.ClinicalResearcher.org. Following SMA, Pearson product-moment correlations were run between treatment phase (A or baseline and B or treatment) and the dependent variable (cigarettes per day) in order to determine the direction and degree of change between baseline and intervention phases for each participant. SMA corrects for autocorrelation in the time series and uses a bootstrap procedure to estimate significance. For an accessible introduction to this statistical technique written for clinical practitioners please see Borckardt et al. (2008) or Borckardt and Nash (2008). An alpha level of .05 two-tailed was used to determine significance for all statistical tests.
Hypnoidal State Scores were categorized as non-hypnoidal, mildly, moderately, or highly hypnoidal according to standard cut-offs on the PCI-HAP, of 1 to 3 being a non-hypnoidal state, 3.01 to 5 being a mild hypnoidal state, 5.01 to 7 being a moderate hypnoidal state, and 7.01 to 9 and above being a high hypnoidal state. Scores on the predicted helpfulness of hypnosis (hypnotic
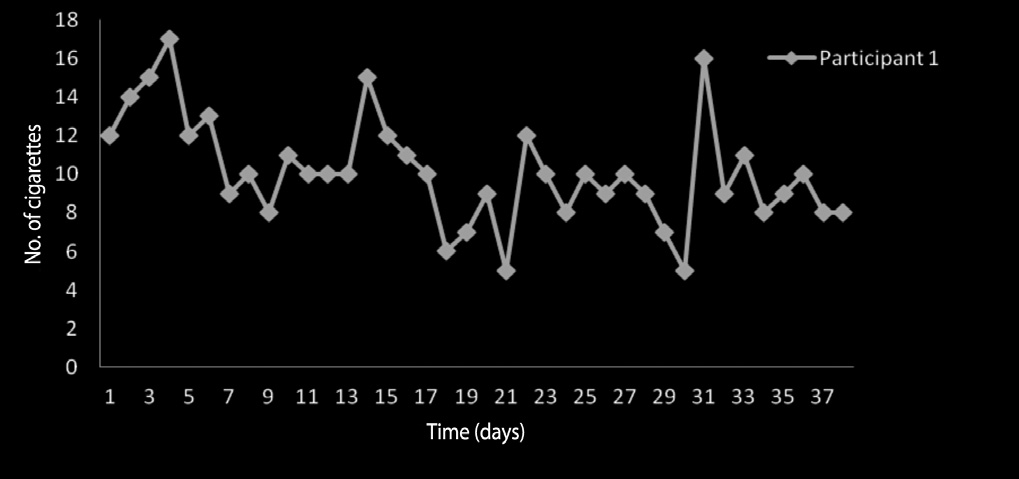
CBT and Hypnosis Treat Smoking 211
treatment expectancy) item of the PCI-HAP were categorized as 1 to 3 being low expectancy, 4 to 7 being moderate expectancy, and 8 to 10 being high expectancy. Scores on the MSPSS were categorized as low, moderate or high according to where they fell in the range of possible scores between the lowest of 12 and the highest of 84, with scores ranging from 12 to 36 being categorized as low social support, scores from 37 to 60 as moderate social support, and scores from 61 to 84 as high social support. Scores on the FTND were categorized as suggested by Heatherton et al. (1991), as 0–2 indicating very low dependence, 3–4 indicating low dependence, 5 indicating medium dependence, 6–7 indicating high dependence, and 8–10 indicating very high dependence. Scores on the three dimensions of depression anxiety and stress of the DASS were grouped as normal, mild, moderate, severe, and extremely severe according to standard published cut-offs relevant to population norms (Lovibond & Lovibond, 1995).
Participant 1 rated in the mild range for hypnotizability, the moderate
range for hypnotic treatment expectancy, the high range for level of social support, the moderate range for nicotine dependence, and the normal ranges for depression, anxiety and stress. He significantly reduced his cigarette consumption from a baseline mean of 13.14 cigarettes per day to a treatment mean of 9.45 (r = -.52, p = .01). Visual inspection of participant 1's cigarette consumption over time shows a general reduction in the treatment phase, with two episodes of heavy cigarette consumption. Participant 1's cigarette consumption over the baseline and treatment phases is presented in Figure 1.
Figure 1: Participant 1: Consumption of Cigarettes per Day Over Baseline and
Intervention Phases
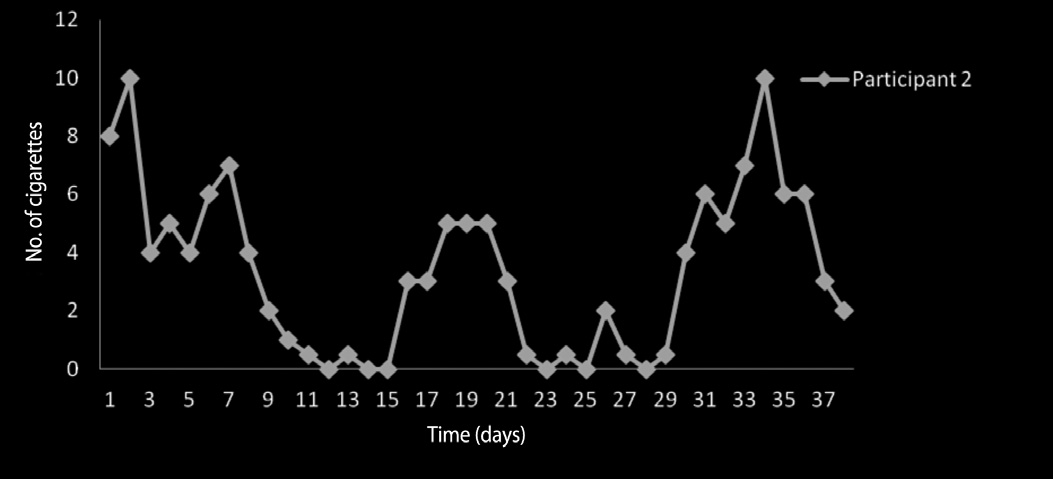
212 Hely, Jamieson, and Dunstan
Participant 2 rated in the moderate range for hypnotizability, the moderate
range for hypnotic treatment expectancy, the low range for level of social support, the high range for nicotine dependence, the severe range for depression, the mild range for anxiety and the moderate range for stress. She did reduce her cigarette consumption from a baseline mean of 6.28 to a treatment mean of 2.47; however, this change was not significant (r = -.49, p = .12). Participant 2 attributed her lack of success at quitting smoking to stressful events. Visual inspection of participant 2's cigarette consumption over time shows two periods of relative success interspersed with two relapse periods. Participant 2's cigarette consumption over the baseline and treatment phases is presented in Figure 2.
Figure 2: Participant 2: Consumption of Cigarettes per Day Over Baseline and
Intervention Phases
Participant 3 rated in the moderate range for hypnotizability, the high range
for hypnotic treatment expectancy, the moderate range for social support, the low range for nicotine dependence, the extremely severe range for depression, the extremely severe range for anxiety, and the severe range for stress. She did reduce her cigarette consumption from a baseline mean of 7.28 to a treatment mean of 5.45; however, this change was not significant (r = -.27, p = .19). Participant 3 reported considerable stressors interfering with quitting smoking over the course of the intervention. Visual inspection of participant 3's cigarette consumption over time shows an unstable baseline, an overall pattern of decreased consumption, with an initial decrease at the beginning of the intervention in line with her quit date, a lengthy relapse, then a consistent reduction in the final week. Participant 3's cigarette consumption over the baseline and treatment phases is presented in Figure 3.
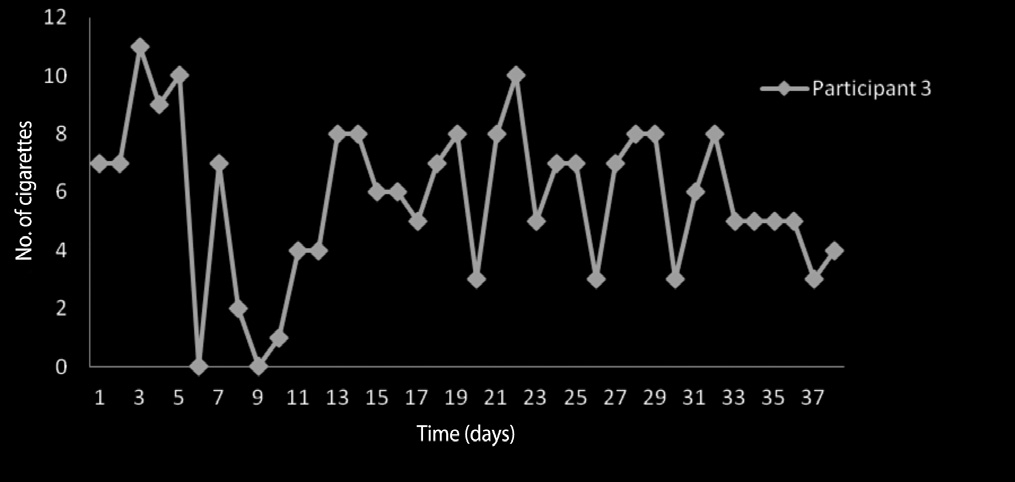
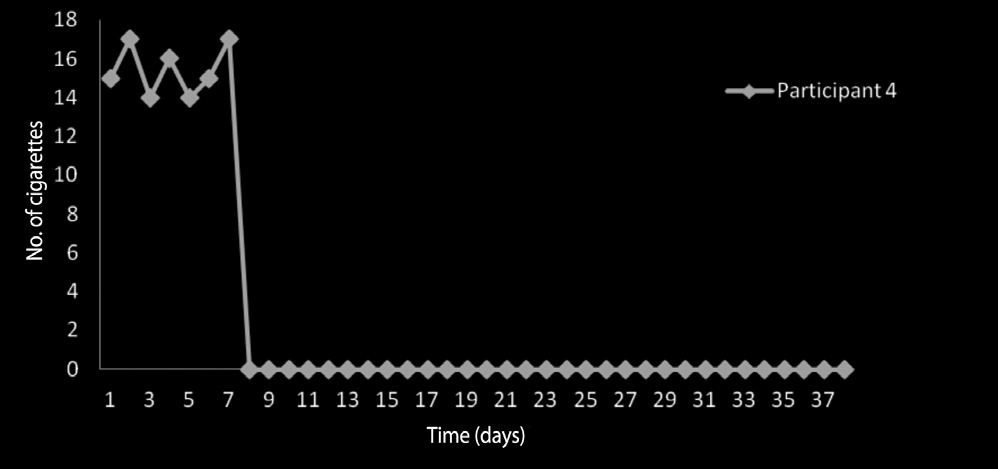
CBT and Hypnosis Treat Smoking 213
Figure 3: Participant 3: Consumption of Cigarettes per Day Over Baseline and
Intervention Phases
Participant 4 rated in the moderate range for hypnotizability, the moderate
range for hypnotic treatment expectancy, the moderate range for social support, the medium range for nicotine dependence, the moderate range for depression, the extremely severe range for anxiety, and the mild range for stress. She ceased smoking during the intervention phase, with a baseline mean of 15.43 and a treatment mean of zero (r = -.996, p = .0001). This result was supported by biochemical verification of smoking cessation with a CO level of 2 ppm. Visual inspection of participant 4's cigarette consumption over time shows a stable baseline consumption with little variability in the number of cigarettes per day and illustrates complete smoking cessation commencing on day one of the intervention followed by continuous abstinence. Participant 4's cigarette consumption over the baseline and treatment phases is presented in Figure 4.
Figure 4: Participant 4: Consumption of Cigarettes per Day Over Baseline and
Intervention Phases
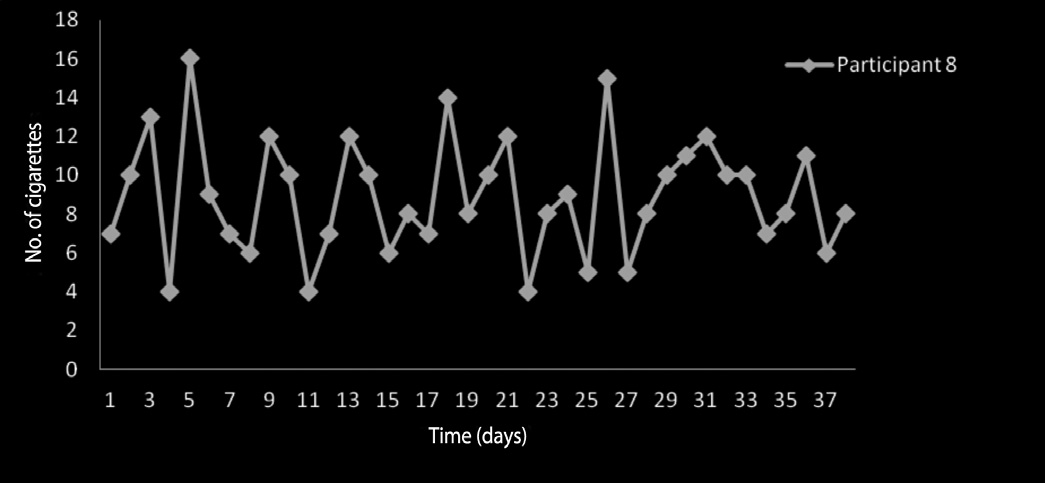
214 Hely, Jamieson, and Dunstan
Participants 5, 6, 7 and 10 failed to complete the study. All four rated in
the high range for social support, and the normal ranges for depression, and normal to mild ranges for anxiety and stress. Their hypnotizability scores were all in the mild to moderate ranges. Their hypnotic treatment expectancy ranged from low to high. Their nicotine dependence ratings varied from the very low to the high categories.
Participant 8 rated in the moderate range for hypnotizability, the low range
for hypnotic treatment expectancy, the high range for social support, the low range for nicotine dependence, and the normal ranges for depression, anxiety and stress. He did not significantly reduce his cigarette consumption (r= -.08, p = .51) from a baseline mean of 9.43 to a treatment mean of 8.84. Participant 8 reported low motivation in regard to quitting smoking, with external pressure to quit cited as the major reason he had participated in the study. Also of note is his expectancy regarding the utility of hypnosis on the PCI-HAP being self-rated at one 1 of 10. Visual inspection of participant 8's data shows no discernable pattern of change between baseline or intervention phases. Participant 8's cigarette consumption over the baseline and treatment phases is presented in Figure 5.
Figure 5: Participant 8: Consumption of Cigarettes per Day Over Baseline and
Intervention Phases
Participant 9 rated in the high range for hypnotic susceptibility, the
moderate range for hypnotic treatment expectancy, the moderate range for social support, the high range for nicotine dependence, and the severe ranges for anxiety, depression and stress. She significantly reduced her cigarette consumption from a baseline mean of 7.57 per day to a treatment mean of
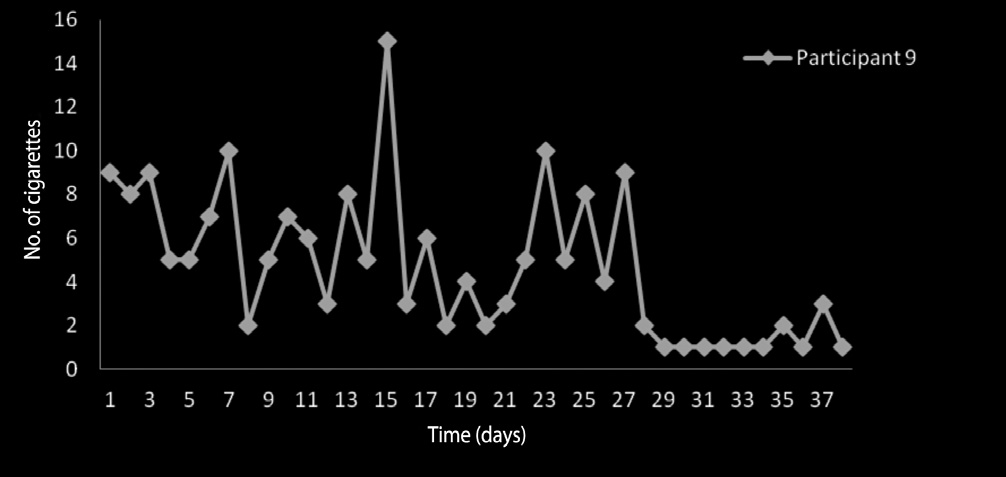
CBT and Hypnosis Treat Smoking 215
3.85 per day (r = -.40, p = .037). Visual inspection of participant 9's cigarette consumption over time shows a modest decrease in consumption at initiation of the treatment phase, one binge episode, and a considerable, consistent decrease in consumption towards the end of the treatment phase. Participant 9's cigarette consumption over the baseline and treatment phases is presented in Figure 6.
Figure 6: Participant 9: Consumption of Cigarettes per Day Over Baseline and
Intervention Phases
Participant 11 rated in the mild range for hypnotic susceptibility, the low
range for hypnotic treatment expectancy, the high range for level of social support, the very low range for nicotine dependence, and the normal ranges for depression, anxiety and stress. He did not significantly reduce his cigarette consumption (r = -.02, p = .93) from a baseline mean of 6.43 to a treatment mean of 6.29. Participant 11 also reported low motivation in regard to smoking cessation. Visual inspection of participant 11's cigarette consumption over time shows an initial decrease following treatment initiation with no discernable pattern to consumption for the rest of the treatment phase. Participant 11's cigarette consumption over the baseline and treatment phases is presented in Figure 7.
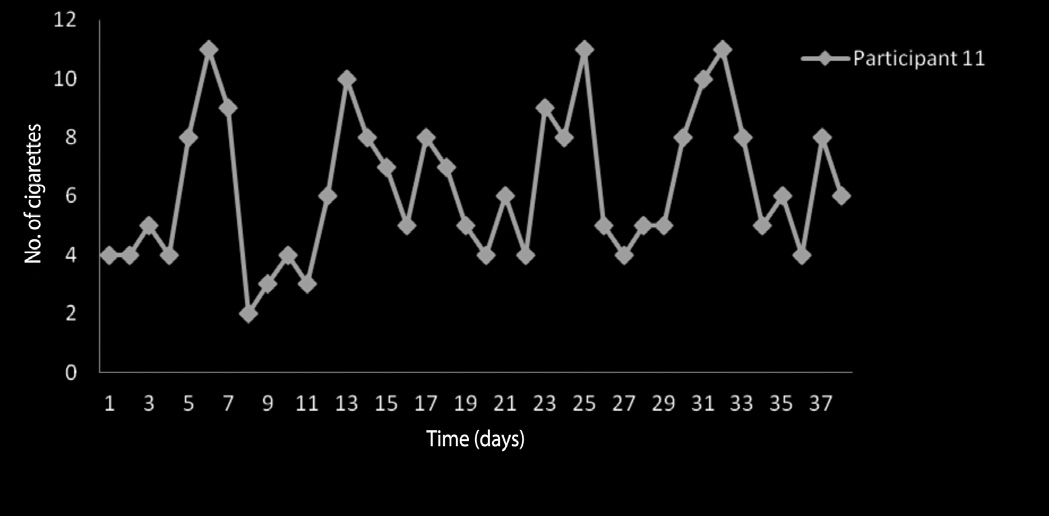
216 Hely, Jamieson, and Dunstan
Figure 7: Participant 11: Consumption of Cigarettes per Day Over Baseline and
Intervention Phases
A summary of demographic and descriptive data is presented in Table 1.
Three of the seven participants who completed the study significantly reduced their nicotine intake, with one participant out of seven managing to achieve complete abstinence immediately after commencing the program. All participants changed their smoking behaviour in the predicted direction. As such, it appears that the hypothesis – that instigation of the combined CBT and hypnosis self-help treatment protocol will significantly reduce cigarette consumption – is supported by the study's results in regard to three of the seven participants. Furthermore, although individual results should be viewed independently in a time-series study of this nature, particularly with a low number of participants limiting the ability to perform further statistical testing, the total abstinence rate of one in seven compares favourably with success rates of other self-help interventions, which have been assessed in a Cochrane meta-analysis as increasing quit rates by only about 1% from no intervention quit rates (Lancaster & Stead, 2005).
All participants who significantly reduced their nicotine consumption had
a moderate to high level of expectancy regarding the efficacy of hypnosis. They also had a moderate to high level of social support. No further patterns regarding the characteristics of successful participants were discernable. Of note is the lack of discernable patterns in regard to hypnotic susceptibility and successful smoking reduction. There did not appear to be a relationship
CBT and Hypnosis Treat Smoking 217
Table 1: Participant Demographics and Scores on Measures of Cigarette Consumption,
Hypnotizability, Social Support, and Depression, Anxiety and Stress
Participant no.
mean (cigarettes/day)
(nicotine dependence)
between hypnotic susceptibility and response to the intervention, with the three participants who managed to reduce their cigarette intake ranging in hypnotizability from being mildly susceptible to highly susceptible, and a similar variation in hypnotizability levels in the unsuccessful participants. It
218 Hely, Jamieson, and Dunstan
remains inconclusive as to whether hypnotic susceptibility is related to this clinical hypnotherapy treatments outcome.
The above finding regarding participants' expectancies for the efficacy of
hypnosis may be viewed as supporting Kirsch's (1999) response expectancy theory, that the individual's belief in hypnosis is primarily responsible for treatment effects. This highlights the similarities between hypnosis and placebo, where response to a suggestion is facilitated by belief in the mechanism that will enable such as response, for example believing that a tablet will result in pain relief enables a person to actually experience pain relief after taking a tablet. Alternatively, a lack of trust or belief in the treatment methodology may result in participants preventing the treatment from working. It is common to a range of psychotherapies including CBT (Ahmed & Westra, 2008) and family therapy (Morrisey-Kane & Prinz, 1999) that some degree of confidence in the treatment is necessary in order for treatment to be successful; however, this does not necessarily imply that such therapies are placebos. Similarly, self-efficacy, or belief in one's own abilities, has been found to be related to treatment success amongst a wide range of disorders (Svengalis, Nygaard, Cervone, & Kreder, 1995); however, no claims have been made that self-efficacy operates simply as a placebo. Belief may simply be a prerequisite for many treatments to work. Borkhardt and Nash (2008) recommend ongoing assessment of hypnotizability in research, in order to gain further information regarding its predictive validity, and in order to shed further light on the nature of hypnosis and hypnotherapy in the ongoing controversy regarding how and why hypnosis works.
Those who did not significantly reduce their smoking behaviour appeared
to have additional impediments which affected their ability to quit. The two female participants of the four who did not significantly reduce their cigarette intake were amongst the highest for depressive symptoms. These two participants did have reductions in their cigarette intake; however, the change was not significant. The two male participants of the four who were unsuccessful in moderating their tobacco use reported low motivation to quit, having enrolled in the program under external pressure. A formal measure of motivation and readiness to quit such as Prochaska DiClemente, Velier, and Rossi's (1993) Stages of Readiness to Change measure would have been a useful addition to this study in order to more formally assess motivation in regard to smoking cessation. These two participants also had the lowest scores regarding their expectancy of the benefits of hypnosis. This again suggests that treatment expectancies are a core element of treatment success.
CBT and Hypnosis Treat Smoking 219
Over half of the participants who completed the study indicated suffering
depression, whereas none of the people who dropped out of the study appeared to have depressive symptoms. Carmody et al. (2008) found that success rates for hypnosis were higher in depressed participants than in participants not suffering from depression. Brown et al. (2001) found a similar result with CBT for heavy smokers with a history of depression. Depression, in this study, appeared more related to treatment adherence than to success. The lack of depressive symptoms in all of the participants who dropped out of this study suggests that hypnosis and/or CBT may hold more appeal to depressed participants, or possibly that non-depressed participants were generally happy with their smoking behaviour and as such did not have the motivation to complete treatment. Again, the inclusion of Prochaska et al.'s (1993) Stages of Readiness to Change measure would have been a valuable addition to the study in order to clarify whether this was a factor in people dropping out of the study. Depression has been found to be higher amongst smokers (Glassman et al., 1990), and as such, any program which appears to have greater appeal to depressed smokers may be of substantial benefit.
Another pattern discernable in the participants who failed to complete the
study was that they all reported high levels of social support, whereas levels of social support were variable amongst those who completed the study. It would be interesting to further explore the relationships between quitting smoking and depression as well as between quitting and social support. Alemi et al.'s (2003) role theory of social support suggests that social support may either increase or decrease health-related behaviours depending upon the role that one may play within a social grouping, and what type of social grouping they belong to. A gang leader, for example, may have a high level of social support, but that social support is likely to encourage unhealthy behaviours. This may hold true for some participants in this study, such as university students who may encounter social environments supportive of binge drinking or smoking. The type of social support may be more important than scoring highly on the overall measure of social support, and social support networks may potentially have the effect of either providing an environment conducive to quitting or exacerbating the addiction (Alemi et al., 2003). Smoking cessation programs and addiction treatment programs in general are often faced with high drop-out rates and an analysis of smoker's support networks may provide an insight into the potential reasons for this phenomenon, which may in turn lead to developments which improve treatment adherence.
220 Hely, Jamieson, and Dunstan
Time-series analysis reveals the individual process of smoking cessation and
reduction beyond providing the significance of differences in means between baseline and intervention phases, by enabling one to visually inspect patterns of change over time. The participant who succeeded at total abstinence appeared to cease smoking completely on her quit date, reinforcing the importance of this concept in successful smoking cessation, whereas no other participants appeared to adhere to the quit date instructions. Some other participants can be seen to have episodes of relapse, reportedly preceded by suffering from depressive symptoms in combination with the occurrence of stressful life events during treatment. Those with self-reported low motivation to quit smoking and low confidence in hypnosis can be seen to have had little pattern of change in their smoking behaviours in response to the instigation of the treatment phase. Being able to observe and analyse patterns of behaviour change is invaluable from a clinical perspective, as it may allow clinicians to determine individual issues and thus tailor treatment to the individual's needs, for example, increasing emphasis on stress management, adding grief counselling as a component of treatment, or assisting a client through the stages of change. In the field of addictions treatment, which is notoriously complex (Myers & Salt, 2007), information of this type is invaluable to clinicians. Furthermore, being able to validly conduct statistical comparisons between the baseline and intervention phases via use of techniques such as SMA increases the utility of time-series designs beyond unreliable "eyeballing" (Carbone & Gorr, 2007, p. 153) of the data to determine whether change has occurred.
Although from a clinical perspective a study of this nature provides
information which would be unable to be gleaned in an RCT, large-scale RCTs remain the benchmark in order to conclusively determine efficacy and examine interactions (Borckardt & Nash, 2008), particularly when pitting psychological interventions against pharmacological ones. They are also more amenable to incorporation in studies such as the Cochrane meta-analysis of hypnosis for smoking cessation (Abbot et al., 2008). It is, however, important for exploratory studies such as this to be carried out, in order to build support for treatment protocols and provide future justification for RCTs to be performed. This study, in particular, provides preliminary evidence which supports the potential value of further research regarding the treatment protocol in particular, and combining CBT and hypnosis in general. An expanded testing program involving a larger number of participants with more
CBT and Hypnosis Treat Smoking 221
diverse characteristics than Anglo-Australians from regional NSW appears warranted.
Despite the promise of this preliminary study, the benchmark for smoking
cessation remains six months of biochemically verified abstinence. Six months appears in previous research to be a point from which cessation rates become relatively stable and the occurrence of relapse decreases (Spiegel, Frischholz, Fleiss, & Spiegel, 1993). As such it would be useful to obtain a follow-up diary and measurement of carbon monoxide at the six-month point from each participant by the addition of a further follow-up phase, in order to assess success against this benchmark. It has been argued that complete abstinence is the required benchmark due to the claim that reduction in intake does not result in reduction in health problems (Godtfredsen, Holst, Prescott, Vestbo, & Osler, 2002; Le Foll & George, 2007). It can be argued, however, that cigarette reduction is in fact of benefit to smokers, both in terms of reduced health impact, with a reduction of cigarette consumption having been found to result in decreased toxin exposure and improved pulmonary function, and in terms of improving their chances of successfully quitting in the future via lessening the strength of their habit and moving through the stages of change into a preparatory stage (Le Houezec & Säwe, 2003). Reduction methods have in fact been shown to be somewhat effective for smoking cessation (Le Houezec & Säwe, 2003; Millatmal et al., 1994). It would also be of interest to examine whether any of the participants were successful at a further attempt to quit smoking within the next six months, as it has been shown that each attempt at quitting increases odds of quitting successfully in the future (Rigotti, 2009).
Continued advancement in the field of smoking cessation research is likely
to be of considerable benefit to smokers, to their families, and to the health system. As such, research regarding the efficacy of programs such as Lynn and Green's (2009) multimodal treatment protocol should be expanded in order to provide conclusive evidence regarding efficacy. A self-help program such as this, which appears in this preliminary study to potentially hold greater efficacy than previous self-help treatments, is likely to be of appeal and of benefit to smokers, particularly those for whom pharmacological treatment is contraindicated. Such a treatment may also potentially be combined in future with pharmacological intervention, in order to provide smokers with comprehensive treatment to maximize their chances of successfully quitting smoking.
222 Hely, Jamieson, and Dunstan
Abbot, N. C., Stead, L. F., White, A. R., & Barnes, J. (1998) Hypnotherapy for smoking
cessation. Cochrane Database of Systematic Reviews, 2.
Abbot, N. C., Stead, L. F., White, A. R., & Barnes, J. (2008). Hypnotherapy for smoking
cessation (Review). The Cochrane Library, 4, 1–19. Retrieved 3 September 2009, from http://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD001008/pdf_standard_fs.html
Ahmed, M., & Westra, H. A. (2008). Impact of a treatment rationale on expectancy and
engagement in cognitive behavioral therapy for social anxiety. Cognitive Therapy and Research, 33, 314–322.
Alemi, F., Stephens, R., Arendt, R., Llorens, S., Schaffer, D., & Nemes, S. (2002). The
Orientation of Social Support Measure. Addictive Behaviors, 28, 1285–129
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders,
text revision (4th ed.). Washington, DC: Author.
Borckardt, J. J., & Nash, M. R. (2008) Making a contribution to the clinical literature: Time-
series designs. In M. R. Nash & A. J. Barnier (Eds.), The Oxford handbook of hypnosis: Theory, research and practice. Oxford: Oxford University Press.
Borckardt, J. J., Nash, M. R., Murphy, M. D., Moore, M., Shaw, D., & O'Neil, P. (2008).
Clinical practice as a natural laboratory for psychotherapy based research: A guide to case-based time-series analysis. American Psychologist, 63, 77–95.
Brandon, T. H. (2001). Behavioural tobacco cessation treatments: Yesterday's news or
tomorrow's headlines? Journal of Clinical Oncology, 19, 64–68.
Brown, R. A., Kahler, C. W., Niaura, R., Abrams, D. B., Sales, S. D., Ramsey, S. E., Goldstein,
M. G., Burgess, E. S., & Miller, I. W. (2001). Cognitive behavioral treatment for depression in smoking cessation. Journal of Consulting and Clinical Psychology, 69, 471–480.
Buchkremer, G., & Minneker, E. (1989). Efficacy of multimodal smoking cessation therapy
combining transdermal nicotine substitution with behavioral therapy. Methods and Findings in Experimental and Clinical Pharmacology, 11, 219–22.
Carbone, R., & Gorr, W. L. (2007). Accuracy of judgmental forecasting of time series.
Decision Sciences, 16, 153–160.
Carmody, T. P., Duncan, C., Simon, J. A., Solkowitz, S., Huggins, J., Lee, S., & Delucchi, K.
(2008). Hypnosis for smoking cessation: A randomized trial. Nicotine and Tobacco Research, 10, 811–818.
Collins, D., & Lapsley, H. (2002). Counting the cost: Estimates of the social costs of drug abuse
in Australia in 1998–9. Canberra: Commonwealth Department of Health and Ageing.
Covino, N. A., & Bottari, M. (2001). Hypnosis, behavioral theory and smoking cessation.
Journal of Dental Education, 65, 340–347.
Crawford, J. R., & Henry, J.D. (2003). The Depression Anxiety Stress Scales (DASS):
Normative data and latent structure in a large non-clinical sample. British Journal of Clinical Psychology, 42,111–131 [Abstract]. Retrieved 5 August 2009, from http://cat.
inist.fr/?aModele=afficheN&cpsidt=14923247
CBT and Hypnosis Treat Smoking 223
Crittenden, K. S., Manfredi, C., Warnecke, R. B., Ik Cho, Y., & Parsons, J. A. (1998).
Measuring readiness and motivation to quit smoking among women in public health clinics: Predictive validity. Addictive Behaviors, 23, 191–199. Retrieved 30 July 2009, from http://psycnet.apa.org/?fa=main.doiLanding&uid=2002-06218-005
Dahlem, N. W., Zimet, G. D., & Walker, R. R. (2006). The multidimensional scale of
perceived social support: A confirmation study. Journal of Clinical Psychology, 47, 756–761.
Delmonte, M. M. (1985). Meditation and anxiety reduction: A literature review. Clinical
Psychology Review, 5, 91–102.
Department of Health and Ageing. (2006). Health Insite website. Viewed June 2006, at
Egner, T., Jamieson, G., & Gruzelier, J. (2005). Hypnosis decouples cognitive control from
conflict monitoring processes of the frontal lobe. Neuaroimage, 27, 969–978.
Elkins, G. R., Marcus, J., Bates, J., Rajab, M. H., & Cook, T. (2006). Intensive hypnotherapy
for smoking cessation: A prospective study [Abstract]. International Journal of Clinical and Experimental Hypnosis, 54, 303–315.
Ewer, T. C., & Stewart, D. E. (1986). Improvement in bronchial hyper-responsiveness in
patients with moderate asthma after treatment with a hypnotic technique: A randomized controlled trial. British Medical Journal, 293(6555), 1129–1132.
Eysenck, M. W. (2004). Psychology: An international perspective. Hove: Psychology Press.
Fagerstrom, K., & Schneider, N. G. (1989). Measuring nicotine dependence: A review
of the Fagerstrom Tolerance Questionnaire. Journal of Behavioral Medicine, 12, 159–182. Retrieved 1 August 2009, from http://www.springerlink.com/content/j275u36n87322687/
Faymonville, M., Roediger, L., Del Fiore, G., Delgueldre, C., Phillips, C., Lamy, M.,
Luxen, A., Maquet, P., & Laureys, S. (2003). Increased cerebral functional connectivity underlying the antinociceptive effects of hypnosis. Cognitive Brain Research, 17, 255–262.
Forbes, E., & Pekala, R. J., (1993). Predicting hypnotic susceptibility via a phenomenological
approach. Psychological Reports, 73, 1251–1256.
Glassman, A. H., Helzer, J. E., Covey, L. S., Cottler, L. B., Stetner, F., Tipp, J. E., & Johnson, J.
(1990). Smoking, smoking cessation and major depression. Journal of the American Medical Association, 264, 637–640.
Godtfredsen, N. S., H olst, C., Prescott, E., Vestbo, J., & Osler, M. (2002). Smoking reduction,
smoking cessation, and mortality: A 16-year follow-up of 19,732 men and women from the Copenhagen Centre for Prospective Population Studies. American Journal of Epidemiology, 156, 994–1001.
Goran, D. K. (1991). The effects of hypnosis and hypnotizability testing on chronic pain.
Unpublished manuscript. Retrieved 20 August 2009, from http://drc.ohiolink.edu/handle/2374.OX/16353?show=full
Green, J. P., Lynn, S., & Montgomery, G. H. (2008). Gender-related differences in hypnosis-
based treatments for smoking: A follow-up meta-analysis. American Journal of Clinical Hypnosis, 50, 259–271.
Hajek, P. (1996). Current issues in behavioral and pharmacological approaches to smoking
cessation. Addictive Behaviors, 21, 699–707.
224 Hely, Jamieson, and Dunstan
Heatherton, T. F., Kozlowski, L. T., Frecker, R. C., & Fagerstrom, K. O. (1991). The
Fagerstrom Test for Nicotine Dependence: A revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addictions, 86, 1119–1127.
Hegaard, H. K., Kjaergaard, H., Moller, L. F., Wachmann, H., & Ottesen, B. (2003).
Multimodal intervention raises smoking cessation rate during pregnancy. Acta Obstetricia et Gynecologia Scandinavica, 82, 813–819 [Abstract]. Retrieved 9 September 2009, from http://www.ncbi.nlm.nih.gov/pubmed/12911442
Henry, J. D., & Crawford, J. R. (2005). The short-form version of the Depression Anxiety
Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. British Journal of Clinical Psychology, 44, 227–239.
Hitsman, B., Borrelli, B., McChargue, D. E., Spring, B., & Niaura, R. (2003). History of
depression and smoking cessation outcome: A meta-analysis. Journal of Consulting and Clinical Psychology, 71, 657–663.
Hyland, A., Borland, R., Li, Q., Yong, H. H., McNeill, A., Fong, G. T., O'Connor, R. J., &
Cummings, K. M. (2006). Individual level predictors of cessation behaviours among participants in the International Tobacco Control (ITC) four country survey. Tobacco Control, 15(Suppl. 3), 83–94.
Janz, N. K., Becker, M. H., Kirscht, J. P., Eraker, S. A., Billi, J. E., & Woolloscroft, J. O. (1987).
Evaluation of a minimal contact smoking cessation intervention in an outpatient setting. American Journal of Public Health, 77, 805–809.
Jorenby, D. E., Leischow, S. J., Nides, M. A., Rennard, S. I., Johnston, J. A., Hughes, A. R.,
Smith, S. S., Muramoto, M. L., Daughton, D. M., Doan, K., Fiore, M. C., & Baker, T. B. (1999). A controlled trial of sustained-release bupropion, a nicotine patch, or both for smoking cessation. New England Journal of Medicine, 340, 685–691.
Kane, P., & Reinecke, M. A (2006). Cognitive behavior therapy and the utility of hypnosis
as an adjunct to treatment. In R. A. Chapman (Ed.), The clinical use of hypnosis in cognitive behavior therapy (pp. 45–69). New York: Springer.
Kirsch, I. (1999). Hypnosis and placebos: Response expectancy as a mediator of suggestion
effects. Annals of Psychology, 15, 99–110.
Klesges, R. C., Meyers, A. W., Klesges, L. M., & LaVasque, M. E. (1989). Smoking, body
weight, and their effects on smoking behavior: A comprehensive review of the literature. Psychological Bulletin, 106, 204–230 [Abstract]. Retrieved 1 August 2009, from http://psycnet.apa.org/?fa=main.doiLanding&doi=10.1037/0033-2909.106.2.204
Lancaster, T., & Stead, L. F. (2005). Self-help interventions for smoking cessation. Cochrane
Database of Systematic Reviews, 3. Retrieved 5 August 2009, from http://mrw.interscience.
wiley.com/cochrane/clsysrev/articles/CD001118/frame.html
Lawhon, D., Humfleet, G. L., Hall, S. M., Reus, V. I., & Munoz, V. I. (2009). Longitudinal
analysis of abstinence-specific social support and smoking cessation. Health Psychology, 28, 465–472.
Le Foll, B., & George, T. P., (2007). Treatment of tobacco dependence: Integrating recent
progress into practice. Canadian Medical Association Journal, 177, 1373–1380.
CBT and Hypnosis Treat Smoking 225
Le Houezec, J., & Säwe, U. (2003). Smoking reduction and temporary abstinence: New
approaches for smoking cessation. Journal des Maladies Vasculaires, 28, 293–300.
Lovibond, S. H., & Lovibond, P. F. (1995). Manual for the depression anxiety stress scales. Sydney:
Lynn, S. J., & Green, J. P. (2011). The sociocognitive and dissociation theories of hypnosis:
Toward a rapprochement. International Journal of Clinical and Experimental Hypnosis, 59, 277–293.
Lynn, S. J., Green, J. P., & Brandon, T. H. (2009). Grant application for study of combined hypnosis
and CBT treatment protocol comparing group and self-help delivery formats. Unpublished manuscript.
Lynn, S. J., & Kirsch, I. (2006). Essentials of clinical hypnosis: An evidence-based approach.
Washington, DC: American Psychological Association.
Millatmal, T., Daughton, D., Thompson, A. B., Floreani, A. A., Romberger, D., Epperson,
K., Larson, L., & Rennard, S. I. (1994). Smoking reduction: An alternative approach for smokers who cannot quit. Monaldi Archives for Chest Disease, 49, 421–424.
Morrisey-Kane, E., & Prinz, R. J. (1999). Engagement in child and adolescent treatment:
The role of parental cognitions and attributions. Clinical Child and Family Psychology Review, 2, 183–198.
Myers, P. L., & Salt, N. R. (2007). Becoming an addictions counsellor (2nd ed.). Sudbury, MA:
Jones & Bartlett.
NSW Department of Health. (2007). Quit because you can [Brochure].
O'Brien, C. P., & McLellan, A. T. (1996). Myths about the treatment of addiction. Lancet,
Pan, W. (2006). Proactive telephone counselling as an adjunct to minimal intervention for
smoking cessation: A meta-analysis. Health Education Research, Theory and Practice, 21, 416–427.
Pekala, R. J., & Kumar, V. K. (1984). Predicting hypnotic susceptibility by a self-report
phenomenological state instrument. American Journal of Clinical Hypnosis, 27, 114–121.
Pekala, R. J., & Kumar, V. K. (1987). Predicting hypnotic susceptibility via a self-report
instrument: A replication. American Journal of Clinical Hypnosis, 30, 57 –65.
Pekala, R. J., & Kumar, V. K. (2007). An empirical–phenomenological approach to
quantifying consciousness and states of consciousness: With particular reference to understanding the nature of hypnosis. In G. Jamieson (Ed.), Towards a cognitive-neuroscience of hypnosis and conscious states: A resource for researchers, students, and clinicians (pp. 167–194). London: Oxford University Press.
Pekala, R. J., Kumar, V. K., & Maurer, R. (2005). Therapist's manual: Interpretation of the
Phenomenology of Consciousness Inventory – Hypnotic Assessment Procedure (PCI-HAP). Unpublished manuscript.
Pekala, R. J., Kumar, V. K., Maurer, R., Elliott-Carter, N., & Moon, E. (2006). "How
deeply hypnotized did I get?" Predicting self-reported hypnotic depth from a phenomenological assessment instrument. International Journal of Clinical and Experimental Hypnosis, 54, 316–339.
226 Hely, Jamieson, and Dunstan
Pomerleau, C. S., Carton, S. M., Lutzke, M. L., Flessland, K. A., & Pomerleau, O. F. (1994).
Reliability of the Fagerstrom Tolerance Questionnaire and the Fagerstrom Test for Nicotine Dependence. Addictive Behaviors, 19, 33–39.
Potter, G. (2004). Intensive therapy: Utilizing hypnosis in the treatment of substance abuse
disorders. American Journal of Clinical Hypnosis, 47, 21–29.
Prochaska, J. O., DiClemente, C. C., Velicer, W. F., & Rossi, J. S. (1993). Standardized,
individualized, interactive, and personalized self-help programs for smoking cessation. Health Psychology, 12, 399–405.
Raij, T. T., Numminen, J., Narvanen, S., Hiltunen, J., & Hari, R. (2005). Brain correlates
of subjective reality of physically and psychologically induced pain. Proceedings of the National Academy of Sciences of the United States of America, 102, 2147–2151.
Rainville, P., Duncan, G. H., Price, D. D., Carrier, B., & Bushnell, C. (1997). Pain affect
encoded in human anterior cingulate but not in somatosensory cortex. Science, 277, 968.
Reus, V. I., & Smith, B. J. (2008). Multimodal techniques for smoking cessation: A review
of their efficacy and utilization and clinical practice guidelines. International Journal of Clinical Practice, 62, 1753–1768 [Abstract]. Retrieved 9 September 2009, from http://www.ncbi.nlm.nih.gov/pubmed/18795968
Rigotti, N. (2009). Smoking cessation. In A. H. Goroll & A. G. Mulley (Eds.), Primary care
medicine: Office evaluation and management of the adult patient (6th ed.) (pp. 439–446). Philadelphia: Lippincott Williams & Wilkins.
Schubert, D. K. (1983). Comparison of hypnotherapy with systematic relaxation in the
treatment of cigarette habituation. Journal of Clinical Psychology, 39, 198–202.
Silagy, C., Lancaster, T., Stead, L., Mant, D., & Fowler, G. (2007). Nicotine replacement
therapy for smoking cessation (Review). The Cochrane Library, 3, 1–105.
Spiegel, D., Frischholz, E. J., Fleiss, J. L., & Spiegel, H. (1993). Predictors of smoking
abstinence following a single session restructuring intervention with self-hypnosis. American Journal of Psychiatry, 150, 1090–1097.
Spiegler, M. D., & Guevremont, D. C. (2003). Contemporary behavior therapy (4th ed.).
Belmont, CA., Thomson Wadsworth.
Spinhoven, P., & ter Kuile, M. M. (2000). Treatment outcome expectancies and hypnotic
susceptibility as moderators of pain reduction in patients with chronic tension-type headache. The International Journal of Clinical and Experimental Hypnosis, 48, 290–305.
Stead, L. F., & Lacaster, T. (2009). Group behaviour therapy programmes for smoking
cessation (Review). The Cochrane Library, 2, 1–77.
Svengalis, S., Nygaard, I. E., Cervone, D., & Kreder, K. J. (1995). Perceived self-efficacy
as a predictor of outcome of pelvic muscle exercises in the treatment of urinary incontinence. International Urogynecology Journal, 6, 262–266.
Sykes, C. M., & Marks, D. F (2001). Effectiveness of a cognitive behaviour therapy self-help
programme for smokers in London, UK. Health Promotion International, 16, 225–260. Retrieved 3 September 2009, from http://heapro.oxfordjournals.org/cgi/content/full/16/3/255
CBT and Hypnosis Treat Smoking 227
US Department of Health and Human Services. (1984). The health consequences of smoking:
Chronic obstructive lung disease: A report of the Surgeon General. DHHS Publication No. PHS 84-50204. Rockville, MD: US Department of Health and Human Services, Public Health Service, Office on Smoking and Health.
US Food and Drug Administration. (2009). The smoking cessation aids varenicline
(marketed as Chantix) and bupropion (marketed as Zyban and generics): Suicidal ideation and behavior. Postmarket Reviews, 2(1). Retrieved 9 September 2009, from http://www.fda.gov/Drugs/DrugSafety/DrugSafetyNewsletter/ucm110235.htm
Watson, D., Clark, L. A., & Tellegen, A. 1988. Development and validation of brief measures
of positive and negative affect: The PANAS scale. Journal of Personality and Social Psychology, 54, 1063–1070
Wetter, D. W., Kenford, S. L., Smith, S. S., Fiore, M. L., Jorenby, D. E., & Baker, T. B. (1999).
Gender differences in smoking cessation. Journal of Consulting and Clinical Psychology, 67, 555–562.
Wise, L., & Correia, A. (2008). A review of nonpharmacologic and pharmacologic therapies
for smoking cessation. Formulary 43(2), 44–64. Retrieved 12 October 2008, from http://findgalegroup.com.ezproxy.une.edu.au/itx/start.do?prodId=EAIM
Wonnacott, S., Sidhpura, N., & Balfour, D. J. K. (2005). Nicotine: From molecular
mechanisms to behaviour. Current Opinion in Pharmacology, 5, 53–59.
Zimet, G. D., Dahlem, N. W., Zimet, S. G., & Farley, G. K. (1988). The Multidimensional
Scale of Perceived Social Support. Journal of Personality Assessment, 52, 30–41.
Zwar, N., Richmond, R., Borland, R., Stillman, S., Cunningham, M., & Litt, J. (n.d.).
Smoking cessation guidelines for Australian general practice. Retrieved 8 September 2009, from http://www.quitsa.org.au/cms_resources/documents/AustralianGeneralPracticeGuidelineHandbook.pdf
Source: https://www.hipnosis.org.es/biblioteca-hipnosis/hipnosis-revistas/australian-journal-of-clinical-and-experimental-hypnosis-11-2011.pdf
Surface Analysis under Ambient Conditions UsingPlasma-Assisted Desorption/Ionization MassSpectrometry Lucy V. Ratcliffe,† Frank J. M. Rutten,†,# David A. Barrett,*,† Terry Whitmore,‡ David Seymour,‡Claire Greenwood,‡ Yolanda Aranda-Gonzalvo,‡ Steven Robinson,§ and Martin McCoustra†,⊥ Centre for Analytical Bioscience, School of Pharmacy, University of Nottingham, University Park, Nottingham, NG7 2RD,United Kingdom, Hiden Analytical Ltd., 420 Europa Boulevard, Warrington, Cheshire, WA5 7UN, United Kingdom, andForensic Science Service, Unit 2900, Solihull Parkway, Birmingham Business Park, Birmingham, B37 7YN, United Kingdom
Breast Cancer, Cancer and Surgery The Condition: Tumors in the breasts are not uncommon, especially after age 30. Tumors may be cancerous (malignant) or non-cancerous (benign). Approximately one in nine women will develop breast cancer. Early detection can be made with regular, manual self-examinations of the breasts, but not all tumors can be