Niph.org.kh

Ethical considerations in biomedical HIV prevention trials
UNAIDS/WHO guidance document
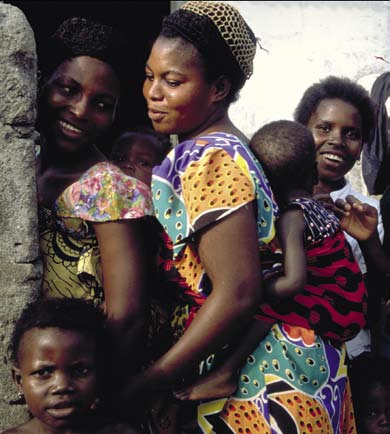
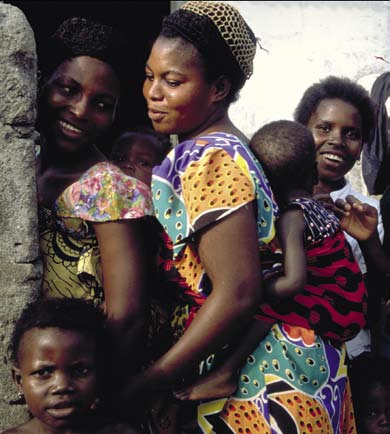
Cover photos: L Taylor/UNAIDS, S Noorani/UNAIDS
UNAIDS/07.28E / JC1349E (English original, July 2007)
Joint United Nations Programme on HIV/AIDS (UNAIDS)
2007. All rights reserved.
The designations employed and the presentation of the
material in this publication do not imply the expression of
any opinion whatsoever on the part of UNAIDS concerning
the legal status of any country, territory, city or area or of
its authorities, or concerning the delimitation of its frontiers
UNAIDS does not warrant that the information contained
in this publication is complete and correct and shall not be liable for any damages incurred as a result of its use.
WHO Library Cataloguing-in-Publication Data
Ethical considerations in biomedical HIV prevention trials.
«UNAIDS/07.28E / JC1349».
1.HIV infections - prevention and control. 2.Bioethics.
3.Biomedical research. 4.Intervention studies. I.UNAIDS.
II.World Health Organization.
ISBN 978 92 9 173625 6 (NLM classification: WC 503.6)
UNAIDS – 20 avenue Appia – 1211 Geneva 27 – SwitzerlandTelephone: (+41) 22 791 36 66 – Fax: (+41) 22 791 48 35E-mail: [email protected] – Internet: http://www.unaids.org
Ethical considerations in biomedical HIV prevention trials
UNAIDS and WHO gratefully acknowledge the contribution of the Expert Panel which proposed changes to the 2000 UNAIDS guidance document "Ethical considerations in HIV preventive vaccine trials". Members of the Expert Panel met in Montreux, Switzerland at a consultation chaired by Catherine Hankins (UNAIDS Secretariat) to review the entire document, discuss each guidance point and come to consensus on suggested wording.
Expert Panel Members:
Quarraisha Abdool Karim*, Women and HIV/AIDS Programme University of KwaZulu Natal, Durban, South Africa
Jorge Beloqui*, Grupo de Incentivo à Vida, Sao Paulo, Brazil
Alexander M. Capron, University of Southern California, Los Angeles, United States of America
Dirceu Greco, Professor, Internal Medicine, Coordinator of the Center of Clinical Research, University Hospital and School of Medicine, Federal University of Minas Gerais, Belo Horizonte, Brazil.
Lori Heise*, Global Campaign for Microbicides, Washington DC, United States of America
Ruth Macklin, Albert Einstein College of Medicine, New York, United States of America
Sheena McCormack, Microbicides Development Programme, Medical Research Council Clinical Trials Unit, London, United Kingdom
Kathleen MacQueen, Family Health International, Research Triangle Park, North Carolina, United States of America
Vasantha Muthuswamy*, Indian Council of Medical Research, New Delhi, India
Punnee Pitisuttithum, Professor for Tropical Medicine, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand
Carmel Shalev, Faculty of Law, Tel Aviv University, Israel
Cathy Slack, HIV/AIDS Vaccine Ethics Group (HAVEG), University of Natal, Durban, South Africa
Daniel Tarantola, University of New South Wales, Sydney, Australia
Morenike Ukpong, Nigeria HIV Vaccines and Microbicide Advocacy Group, Nigeria
Steve Wakefield, HIV Vaccine Trials Network, Seattle, United States of America
Mitchell Warren*, AIDS Vaccine Advocacy Coalition, New York, United States of America
Oversight to the process revising the guidance document was provided by a UNAIDS/WHO Working Group composed of the following members:
Catherine Hankins, UNAIDS Secretariat, Geneva, Switzerland (chair)
Saladin Osmanov, World Health Organization, Geneva, Switzerland
Zarifah Reed, World Health Organization, Geneva, Switzerland
Jason Sigurdson, UNAIDS Secretariat, Geneva, Switzerland
Marie-Charlotte Bouesseau*, World Health Organisation, Geneva, Switzerland
Yves Souteyrand*, World Health Organization, Geneva, Switzerland
Tatiana Lemay*, UNAIDS Secretariat, Geneva, Switzerland
Jolene Nakao, UNAIDS Secretariat, Geneva Switzerland
UNAIDS and WHO would also like to express their sincere appreciation to Carmel Shalev who prepared the draft for the Expert Panel by incorporating content and recommendations from meetings and consultations conducted on topics related to the ethical conduct of biomedical HIV prevention trials as well as related literature since 2000.
Catherine Hankins, Carmel Shalev and Jolene Nakao finalized revisions after the Montreux meeting. Mihika Acharya and Constance Kponvi assisted with editing and Lon Rahn did the layout.
A companion document which readers may wish to consult is the UNAIDS/AVAC Good Participatory Practice for Biomedical HIV Prevention Trials. It covers core principles and essential activities throughout the research life-cycle, providing a foundation for community engagement in research. It is available on the UNAIDS website in a number of languages. For more information please contact [email protected] .
Comments on the Ethical considerations in biomedical HIV prevention trials and experience with implementation of this guidance are welcome. Please send them to [email protected]
* Those who did not attend the Montreux meeting
Ethical considerations in biomedical HIV prevention trials
SUGGESTED GUIDANCE
Guidance Point 1: Development of Biomedical HIV Prevention Interventions 15
Guidance Point 2: Community Participation
Guidance Point 3: Capacity Building
Guidance Point 4: Scientific and Ethical Review
Guidance Point 5: Clinical Trial Phases
Guidance Point 6: Research Protocols and Study Populations
Guidance Point 7: Recruitment of Participants
Guidance Point 8: Vulnerable Populations
Guidance Point 9: Women
Guidance Point 10: Children and Adolescents
Guidance Point 11: Potential Harms
Guidance Point 12: Benefits
Guidance Point 13: Standard of Prevention
Guidance Point 14: Care and Treatment
Guidance Point 15: Control Groups
Guidance Point 16: Informed Consent
Guidance Point 17: Monitoring Informed Consent and Interventions
Guidance Point 18: Confidentiality
Guidance Point 19: Availability of Outcomes
UNAIDS / WHO guidance document
Guidance Point 1: Development of Biomedical HIV Prevention Interventions
Given the human, public health, social, and economic severity of the HIV epidemic, countries, development partners, and relevant international organisations should promote the establishment and strengthening of sufficient capacity and incentives to foster the early and ethical development of additional safe and effective biomedical HIV prevention methods, both from the point of view of countries and communities in which biomedical HIV prevention trials take place, and from the point of view of trial sponsors and researchers.
Guidance Point 2: Community Participation
To ensure the ethical and scientific quality and outcome of proposed research, its relevance to the affected community, and its acceptance by the affected community, researchers and trial sponsors should consult communities through a transparent and meaningful participatory process which involves them in an early and sustained manner in the design, development, implementation, monitoring, and distribution of results of biomedical HIV prevention trials.
Guidance Point 3: Capacity Building
Development partners and relevant international organisations should collaborate with and support countries in strategies to enhance capacity so that countries and communities in which trials are being considered can practice meaningful self-determination in decisions about the scientific and ethical conduct of biomedical HIV prevention trials and can function as equal partners with trial sponsors, local and external researchers, and others in a collaborative process.
Guidance Point 4: Scientific and Ethical Review
Researchers and trial sponsors should carry out biomedical HIV prevention trials only in countries and communities that have appropriate capacity to conduct independent and competent scientific and ethical review.
Guidance Point 5: Clinical Trial Phases
As phases I, II, and III in the clinical development of a biomedical HIV preventive intervention all have their own particular scientific requirements and specific ethical challenges, researchers and trial sponsors should justify in advance the choice of study populations for each trial phase, in scientific and ethical terms in all cases, regardless of where the study population is found. Generally, early clinical phases of biomedical HIV prevention research should be conducted in communities that are less vulnerable to harm or
Ethical considerations in biomedical HIV prevention trials
exploitation, usually within the sponsor country. However, countries may choose, for valid scientific and public health reasons, to conduct any trial phase within their populations, if they are able to ensure sufficient scientific infrastructure and sufficient ethical safeguards.
Guidance Point 6: Research Protocols and Study Populations
In order to conduct biomedical HIV prevention trials in an ethically acceptable manner, researchers and relevant oversight entities should ensure that the research protocol is scientifically appropriate and that the interventions used in the experimental and control arms are ethically justifiable.
Guidance Point 7: Recruitment of Participants.
In order to conduct biomedical HIV prevention trials in an ethically acceptable manner, participation of individuals should be voluntary and the selection of participating communities and individuals must be fair and justified in terms of the scientific goals of the research.
Guidance Point 8: Vulnerable Populations
The research protocol should describe the social contexts of a proposed research population (country or community) that create conditions for possible exploitation or increased vulnerability among potential trial participants, as well as the steps that will be taken to overcome these and protect the rights, the dignity, the safety, and the welfare of the participants.
Guidance Point 9: Women
Researchers and trial sponsors should recruit women into clinical trials in order to verify safety and efficacy from their standpoint, including immunogenicity in the case of vaccine trials, since women throughout the life span, including those who may become pregnant, be pregnant or be breastfeeding, should be recipients of future safe and effective biomedical HIV prevention interventions. During such research, women should receive adequate information to make informed choices about risks to themselves, as well as to their foetus or breastfed infant, where applicable.
Guidance Point 10: Children and Adolescents
Children and adolescents should be included in clinical trials in order to verify safety and efficacy from their standpoint, in addition to immunogenicity in the case of vaccines, since they should be recipients of future biomedical HIV preventive interventions. Researchers, trial sponsors, and countries should make efforts to design and implement biomedical HIV prevention product development programmes that address the particular safety, ethical, and legal
UNAIDS / WHO guidance document
considerations relevant for children and adolescents, and safeguard their rights and welfare during participation.
Guidance Point 11: Potential Harms
Research protocols should specify, as fully as reasonably possible, the nature, magnitude, and probability of all potential harms resulting from participation in a biomedical HIV prevention trial, as well as the modalities by which to minimise the harms and mitigate or remedy them.
Guidance Point 12: Benefits
The research protocol should provide an accurate statement of the anticipated benefit of the procedures and interventions required for the scientific conduct of the trial. In addition, the protocol should outline any services, products, and other ancillary interventions provided in the course of the research that are likely to be beneficial to persons participating in the trials.
Guidance Point 13: Standard of Prevention
Researchers, research staff, and trial sponsors should ensure, as an integral component of the research protocol, that appropriate counselling and access to all state of the art HIV risk reduction methods are provided to participants throughout the duration of the biomedical HIV prevention trial. New HIV-risk-reduction methods should be added, based on consultation among all research stakeholders including the community, as they are scientifically validated or as they are approved by relevant authorities.
Guidance Point 14: Care and Treatment
Participants who acquire HIV infection during the conduct of a biomedical HIV prevention trial should be provided access to treatment regimens from among those internationally recognised as optimal. Prior to initiation of a trial, all research stakeholders should come to agreement through participatory processes on mechanisms to provide and sustain such HIV-related care and treatment.
Guidance Point 15: Control Groups
Participants in both the control arm and the intervention arm should receive all established effective HIV risk reduction measures. The use of a placebo control arm is ethically acceptable in a biomedical HIV prevention trial only
Ethical considerations in biomedical HIV prevention trials
when there is no HIV prevention modality of the type being studied that has been shown to be effective in comparable populations.
Guidance Point 16: Informed Consent
Each volunteer being screened for eligibility for participation in a biomedical HIV prevention trial should provide voluntary informed consent based on complete, accurate, and appropriately conveyed and understood information before s/he is actually enrolled in the trial. Researchers and research staff should take efforts to ensure throughout the trial that participants continue to understand and to participate freely as the trial progresses. Informed consent, with pre- and post-test counselling, should also be obtained for any testing for HIV status conducted before, during, and after the trial.
Guidance Point 17: Monitoring Informed Consent and Interventions
Before a trial commences, researchers, trial sponsors, countries, and communities should agree on a plan for monitoring the initial and continuing adequacy of the informed consent process and risk-reduction interventions, including counselling and access to proven HIV risk-reduction methods.
Guidance Point 18: Confidentiality
Researchers and research staff must ensure full respect for the entitlement of potential and enrolled participants to confidentiality of information disclosed or discovered in the recruitment and informed consent processes, and during conduct of the trial. Researchers have an ongoing obligation to participants to develop and implement procedures to maintain the confidentiality and security of information collected.
Guidance Point 19: Availability of Outcomes
During the initial stages of development of a biomedical HIV prevention trial, trial sponsors and countries should agree on responsibilities and plans to make available as soon as possible any biomedical HIV preventive intervention demonstrated to be safe and effective, along with other knowledge and benefits helping to strengthen HIV prevention, to all participants in the trials in which it was tested, as well as to other populations at higher risk of HIV exposure in the country, potentially by transfer of technology.
UNAIDS / WHO guidance document
Well into the third decade of the HIV pandemic, there remains no effective HIV preventive vaccine, microbicide, product or drug to reduce the risk of HIV acquisition. As the numbers of those infected by HIV and dying from AIDS continue to increase, the need for such biomedical HIV preventive interventions becomes ever more urgent. Several such products are at various stages of development, including some currently in phase III efficacy trials. The successful development of effective HIV preventive interven-tions requires that many different candidates be studied simultane-ously in different populations around the world. This in turn will require a large international cooperative effort drawing on partners from various health sectors, inter-governmental organisations, government, research institutions, industry, and affected populations. It will also require that these partners be able and willing to address the difficult ethical concerns that arise during the development of biomedical HIV prevention products.
Following deliberations during 1997-99 involving lawyers, activists, social scientists, ethicists, vaccine scientists, epidemiologists, non-governmental organisation (NGO) representatives, people living with HIV, and people working in health policy from a total of 33 countries, UNAIDS published a guidance document on ethical considerations in HIV preventive vaccine research in 2000. Since then there have been numerous developments related to the conduct of biomedical HIV prevention trials, including vaccine trials. Consultations have been held to explore key issues such as:
Creating effective partnerships, collaboration and community
participation in HIV prevention trials (International AIDS Society
(IAS) 2005; UNAIDS 2006; UNAIDS/AIDS Vaccine Advocacy
Coalition (AVAC) 2007);
Ethical considerations in biomedical HIV prevention trials
The inclusion of adolescents in HIV vaccine trials (WHO/IVR
2002; WHO/UNAIDS 2004; WHO/UNAIDS/African AIDS
Vaccine Program 2006);
Gender considerations related to enrolment and informed consent
(WHO/UNAIDS 2004);
Provision of support, care and treatment to participants and the
community engaged in HIV prevention trials (WHO/UNAIDS
2003; IAS 2005; UNAIDS 2006; Forum for Collaborative
Research 2006; International AIDS Society Industry Liaison
Post-trial responsibilities of sponsors, researchers and local
providers (AVAC and the International Council of AIDS Service
In light of these consultations, and evolution in the level of prevention, treatment and care available in the era of ‘Towards Universal Access', the 2000 guidance document was revised and updated. The revision incorporates developments which have taken place since the original publication, including lessons learned in the field of biomedical HIV prevention research. Many different strategies for HIV prevention are now being explored, including microbicides, vaccines, female-initiated barrier methods, herpes simplex virus-2 (HSV-2) treatment/suppres-sion, index partner treatment, antiretroviral pre-exposure prophylaxis, prevention of mother-to-child transmission and drug substitution/maintenance for injecting drug users. Of note, following the compel-ling evidence of a 50 to 60 per cent reduction in HIV acquisition for men who became circumcised in three randomised controlled trials in South Africa, Kenya and Uganda, WHO/UNAIDS produced recommendations in 2007 judging adult male circumcision to be an accepted risk reduction measure in men, particularly in high preva-lence generalised HIV epidemics in which heterosexual transmis-sion predominates. Finally, the guidelines in this document specifi-cally address trials of biomedical HIV preventive interventions but are relevant to those engaged in trials of various behavioural HIV prevention methods.
UNAIDS / WHO guidance document
This document does not purport to capture the extensive discussion, debate, consensus, and disagreement which have taken place among stakeholders in HIV prevention research. Rather it highlights, from the perspective of UNAIDS and WHO, some of the critical ethical elements that must be considered during the development of safe and effective biomedical HIV prevention interventions. Where these are adequately addressed, in the view of UNAIDS/WHO, by other existing texts, there is no attempt to duplicate or replace these texts, which should be consulted extensively throughout biomedical HIV prevention product development activities. Such texts include: the Nuremberg Code (1947); the Declaration of Helsinki, first adopted by the World Medical Association in 1964 and most recently amended in 2000 ; the revised International Ethical Guidelines for Biomedical Research Involving Human Subjects, issued in 2002 by the Council for International Organisations of Medical Sciences (CIOMS) (and developed in close cooperation with WHO); the World Health Organization's Handbook for Good Clinical Research Practice (2005); the International Conference on Harmonisation's Good Clinical Practice (ICH GCP) Guideline (1996); and the UNAIDS Interim Guidelines on Protecting the Confidentiality and Security of HIV Information (2007).
Systematic guidance on the role and responsibilities of entities funding and conducting biomedical HIV prevention trials towards participants, and their communities can be found in the UNAIDS/AVAC Good Participatory Practice Guidelines for Biomedical HIV Prevention Trials (2007).
It is hoped that this document will be of use to potential research volunteers and trial participants, investigators, research staff, community members, government representatives, pharmaceutical companies and other industry partners and trial sponsors, and ethical and scientific review committees involved in the development of biomedical HIV prevention products and interventions. It suggests standards, as well as processes for arriving at standards which can be used as a frame of reference from which to conduct further discussion at the local, national, and international levels and can inform the development of national guidelines for the conduct of biomedical HIV prevention trials.
Ethical considerations in biomedical HIV prevention trials
The HIV pandemic is characterised by unique biological, social and geographical factors that, among other things, affect the balance of risks and benefits for individuals and communities who participate in biomedical HIV prevention trials. These factors may require that additional efforts be taken to address the needs of participating indi-viduals and communities. They have an urgent need for additional HIV prevention choices for use at various stages of the life-cycle, a need to have their rights protected and their welfare promoted in the context of the development and testing of novel HIV prevention modalities, and a need to be able to participate fully as equal partici-pants in the research process. These factors include the following:
The global burden of disease and death related to HIV continues
to increase at a rate unmatched by any other pathogen. For many countries, AIDS is the leading cause of death. Currently available treatments do not lead to cure, but do slow the progression of disease. The most effective treatment for slowing HIV-related disease progression, antiretroviral medication, is a life-long treatment which requires close medical monitoring, is still very costly, especially for 2nd line regimens, and can cause significant adverse effects. Because of this, antiretroviral medi-cation is not readily available to the vast majority of people living with HIV who need it. More than 2 million people had access to antiretroviral treatments in low- and middle-income countries in 2006, five times more people than in 2003. But despite this tremendous progress in the roll-out of antiretroviral treatment, global coverage of needs is below 30%.
For every person placed on antiretroviral treatment in 2006,
another six people became newly infected with HIV. There is therefore an ethical imperative to seek, as urgently as possible, effective and accessible biomedical HIV prevention technolo-gies, to complement existing prevention strategies. This ethical
UNAIDS / WHO guidance document
imperative demands that these technologies be developed to address the situation of those people and populations most vulnerable to exposure to HIV infection.
Genetically distinct subtypes of HIV have been described, and
different HIV subtypes are predominant in different regions and countries. The relevance of these sub-types to probabilities of HIV transmission and acquisition, speed of disease progression and potential protection is not clearly understood.
For the conduct of efficacy trials of any biomedical HIV
prevention product, the populations with the highest incidence of HIV will be those most likely to be considered for participa-tion and would be those most likely to benefit from an effective intervention. However, for a variety of reasons, these popula-tions may be relatively vulnerable to exploitation and harm in the context of biomedical HIV prevention trials. Trial sponsors, countries, researchers, research staff and community leaders must make additional efforts to overcome this vulnerability.
In some biomedical HIV prevention trials, individuals other than
the trial participants may experience risks if they are exposed to the experimental product and may experience benefits if the product is effective. For example in trials of prophylaxis of mother-to-child transmission, the foetus is exposed to the prophylactic antiretroviral regimen in addition to the mother. If the mother develops antiretroviral resistance, she may transmit resistant virus to the infant. When the intervention is effective, the newborn baby is protected. In trials of vaginal microbicides, male sexual partners may be exposed to the product even when condoms are used. In trials of successful vaccine candidates, not only sexual partners benefit but communities may benefit from population level effects.
Some biomedical HIV prevention modalities may be conceived
and manufactured in laboratories of one country (sponsor country or countries), usually in high-income countries, and tested in human populations in another country, often low- and middle-income countries. The potential imbalance of such a
Ethical considerations in biomedical HIV prevention trials
situation demands particular attention to ways to address the differing perspectives, interests and capacities of trial sponsors, countries, and communities engaged in trials with the goal of encouraging the urgent development of additional safe and effective biomedical HIV prevention tools, in ethically accept-able manners, and their early distribution to populations most in need. Countries and communities considering participa-tion in biomedical HIV prevention trials should be encour-aged and given the capacity to make decisions for themselves regarding their participation, based on their own health and human development priorities, in a context of equal collabora-tion with sponsors.
HIV infection is both highly feared and stigmatised. This is in
large part because it is associated with blood, death, sex, and activities which may not be legally sanctioned, such as commer-cial sex, men having sex with men, and illicit substance use. These are issues which are often difficult to address openly - at a societal and individual level. As a result, people living with HIV and those affected by AIDS may experience stigma, discrimination, and even violence; some communities continue to deny the existence and prevalence of HIV infection. Furthermore, vulnerability to HIV exposure and to the impact of AIDS is greater where people are marginalized due to their social, economic, and legal status. These factors increase the risk of social and psychological harm for people participating in biomedical HIV prevention trials. Additional efforts must be made to address these increased risks and to ensure that the risks participants take are justified by the anticipated benefits of the preventive intervention to the participants themselves or to others in the future.
A key means by which to protect participants and the commu-
nities from which they come is to ensure that the community in which the research is carried out is meaningfully involved in the design, implementation, monitoring, and dissemination of results of HIV prevention trials, including the involvement of representatives from marginalized communities from which participants are drawn.
UNAIDS / WHO guidance document
Site selection for moving forward into empirical efficacy
trials of biomedical HIV prevention technologies is a major challenge. Part of this challenge is the need to integrate biomedical HIV prevention tool development with other HIV prevention modalities, all of which need to be integrated with HIV treatment and care as provided by the local health care system. It is imperative that appropriate financial arrangements are in place to implement agreements made between partners at the time a study is initiated. These agreements should cover the period of the trial but also address what will be provided to study participants once the study is completed. Advance planning and collaboration between partners is also needed to facilitate timely product licensure and distribution once a method has been proven safe and effective.
It has been the experience to date that HIV incidence in both
the experimental and control arms of biomedical HIV preven-
tion trials tends to fall below the pre-trial incidence, presumably
as a result of sustained risk-reduction counselling and provision
of effective HIV prevention tools. The discovery of additional
safe and effective biomedical HIV preventive interventions will
necessitate discussions among all research stakeholders involved in
planned or active trials of other biomedical HIV prevention tools.
A decision to introduce the new method in a trial that is already
underway has to be made collectively as it may have implications
for resource requirements, sample sizes, and potential futility of
continuing the trial. The possibility that such a decision could be
required should be anticipated during initial discussions among
the research stakeholders.
No single biomedical HIV prevention product or intervention is
now or will be 100 per cent effective. This is in part because none
are expected to achieve 100 per cent efficacy in the controlled
circumstances of a trial and in part because behaviour will
influence both consistency and correctness of uptake for many
of the interventions being investigated, with the result that the
efficacy seen in the trial will not lead to effectiveness at the same
level in the real world. Furthermore, the manner in which an
effective biomedical HIV prevention product is introduced into
comprehensive HIV prevention programming will affect the
Ethical considerations in biomedical HIV prevention trials
extent to which risk compensation1 will occur. Therefore, social
change communication strategies which emphasize combination
prevention will be crucial to ensure that a new biomedical HIV
prevention product truly does add to the existing tools when it is
Selected circumstances in which biomedical
HIV prevention trials should not be conducted
when the product to be tested would not be appropriate for
use, should it be proven safe and effective, in the community
that would participate in the trial (see Guidance Point 1);
when capacity to conduct independent and competent scien-
tific and ethical review does not exist (see Guidance Point 4);
where truly voluntary participation and ongoing free informed
consent cannot be obtained (see Guidance Point 7);
when conditions affecting potential vulnerability or exploita-
tion may be so severe that the risk outweighs the benefit of
conducting the trial in that population (see Guidance Point 8);
when a survey of protective local laws and regulations applicable
at the trial site has not been conducted or when such a survey
indicates insurmountable legal barriers (see Guidance Point 10);
when agreements have not been reached among all research
stakeholders on standard of prevention (see Guidance Point 13)
and access to care and treatment (see Guidance Point 14);
when agreements have not been arrived at on responsibili-
ties and plans to make a trial product which proves safe and
effective affordably available to communities and countries
where it has been tested (see Guidance Point 19).
� Risk compensation: an increase in risk-taking as a result of a decrease in perception
� The term "combination prevention" refers to the combination of various strategies
that individuals can choose at different times in their lives to reduce their risks of
sexual exposure to the virus.

Ethical considerations in biomedical HIV prevention trials
SUGGESTED GUIDANCE
Guidance Point 1:
Development of Biomedical HIV Prevention Interventions
Given the human, public health, social, and economic severity of the HIV epidemic, countries, development partners, and relevant international organisations should promote the establishment and strengthening of sufficient capacity and incentives to foster the early and ethical development of additional safe and effective biomedical HIV prevention methods, both from the point of view of countries and communities in which biomedical HIV prevention trials take place, and from the point of view of trial sponsors and researchers.
Given the global nature of the epidemic, the devastation being wrought in some countries by it, the fact that biomedical HIV preventive interventions may be the best long term solution by which to control the epidemic, especially in low- and middle-income countries, and the potentially universal benefits of effective biomedical HIV prevention tools, there is an ethical imperative for global support to develop these modalities. This effort requires intense international collaboration and coordination over time among countries with scientific expertise and resources, and countries in which candidate products could be tested but whose infrastructure, resource base, and scientific and ethical capacities may need strengthening. Though potential HIV prevention tools such as microbicides, vaccines, herpes simplex virus-2 (HSV-2) suppression/treatment, female-initiated barrier methods, index partner treatment, antiretroviral drugs for prophylaxis, and biomedical interventions for injecting drug users should benefit all those in need, it is imperative that they benefit the populations at greatest risk of exposure to HIV. Thus, HIV prevention
UNAIDS / WHO guidance document
product development should ensure that products are appropriate for use among such populations, among which it will be necessary to conduct trials; and, when developed, they should be made available and affordable to such populations.
Because HIV prevention product development activities take time, are complex, and require infrastructure, resources, and international collaboration,
countries who may sponsor trials and countries who may
participate in trials should include biomedical HIV prevention
product development in their national HIV prevention and
control plans.
countries who may participate in trials should assess how they
can and should take part in biomedical HIV prevention product
development activities either nationally or on a regional basis,
including identifying resources, establishing partnerships,
conducting national information and research literacy campaigns,
strengthening their scientific and ethical sectors, and including
biomedical HIV prevention product research to complement
current comprehensive HIV prevention programming.
development partners, international agencies, and governments
should make early and sustained commitments to allocate sufficient
funds to make biomedical HIV preventive interventions a reality.
This includes funds to strengthen ethical and scientific capacity
in countries where multiple trials will have to be conducted, to
enhance South-South as well as North-South capacity building
and technology transfer, and to purchase and distribute future
biomedical HIV prevention tools.
potential trial sponsors and countries who may participate in
trials should establish partnerships with each other, initiate
community consultations, support the strengthening of
necessary scientific and ethical components, and make plans
with all stakeholders for equitable distribution of the benefits of

Ethical considerations in biomedical HIV prevention trials
Guidance Point 2:
Community Participation2
To ensure the ethical and scientific quality and outcome of proposed research, its relevance to the affected community, and its acceptance by the affected community, researchers and trial sponsors should consult communities through a transparent and meaningful participatory process which involves them in an early and sustained manner in the design, development, implementation, and distribution of results of biomedical HIV prevention trials.
It is highly important to engage in consultations with communities who will participate in the trial from the beginning of the research concept, in an open, iterative, collaborative process that involves a wide variety of participants and takes place under public scrutiny. Participatory management benefits all parties; helps ensure smooth trial functioning; and builds community capacity to understand and inform the research process, raise concerns, and help find solutions to unexpected issues that may emerge once the trial is underway. Failure to properly and genuinely engage communities early in the stages of research planning may result in an inability to properly conduct and complete important trials. Furthermore, active community participation should strengthen not only local ownership of the research, but also the negotiating power of communities, the research skills of local investigators, and the social leverage that can be useful in areas of the society beyond the research trial site. Communities of people affected by research should conversely play an active, informed role in all aspects of its planning and conduct, as well as the dissemination of results. Achieving meaningful participation requires
� Consider further the UNAIDS/AVAC Good Participatory Practice Guidelines for
Biomedical HIV Prevention Trials (�007).
UNAIDS / WHO guidance document
the acknowledgement of structural power imbalances between certain communities and researchers and/or research sponsors, and striving to overcome them. In practical terms, this means putting in place outreach and engagement measures to support participation. Special attention should be paid to the inclusion and empowerment of women for active involvement throughout the research process, as well as to the representation of populations at higher risk of HIV exposure, including adolescents.
The nature of community involvement should be one of continuous
mutual education and respect, partnership, and consensus-building
regarding all aspects of the testing of potential biomedical HIV
prevention products. A continuing forum should be established for
communication and problem-solving on all aspects of the HIV
prevention product development programme from phase I through
phase III and beyond (see Guidance Point 6), to the distribution of a safe
and effective HIV prevention tool. All participating parties should define
the nature of this ongoing relationship. It should include appropriate
representation from the community on committees charged with the
review, approval, and monitoring of a biomedical HIV prevention trial.
As with investigators and sponsors, communities should also assume
appropriate responsibility to assure the successful completion of the
trial and the product development programme.
Defining the relevant community for consultation and partnership is a complex and evolving process that should be discussed with relevant local authorities. As more groups and people define themselves as part of the interested community, the concept needs to be broadened to civil society so as to include advocates, media, human rights organizations, national institutions and governments, as wel as researchers and community representatives from the trial site. Partnership agreements should include a clear delineation of roles for al stakeholders and should specify the responsibilities of sponsors, governments, community, advocacy organiza-tions, and media, as wel as researchers and research staff.
Ethical considerations in biomedical HIV prevention trials
Appropriate community representatives should be determined through a process of broad consultation. An agreement should be reached among stakeholders about the definition of a "community" and ways that it can be effectively represented in decision-making early in the design of the study protocol. The process for determining who will be credible and legitimate community representatives should be addressed through a preliminary consultative process between researchers and key members of the community in which the research is proposed to take place. Members of the community who may contribute to development of a safe and effective HIV prevention product include representatives of the research population eligible to serve as research participants, other members of the community who would be among the intended beneficiaries of the developed product, relevant non-government organisations, persons living with HIV, community leaders, public health officials, and those who provide health care and other services to people living with and affected by HIV.
Formal community meetings need to be organised in a way that facili-tates the active participation of those most affected by the research being proposed. The principal investigator and site research staff should work with representatives of affected communities to identify needs related to their participation, including logistical requirements such as trans-portation to the meeting site. Educational materials should be designed in an accessible format, using easy to understand language. Adequate consultation and full participation in the planning process will require more than formal community meetings, as such meetings may alienate some people or be inaccessible to others due to the timing or the format. The principal investigator and site research staff should make efforts to reach out to affected communities, meeting at community centres, workplaces, and other frequented locations. In both formal and informal consultations, the timing and length of the meetings should be convenient for community members, using approaches that facilitate two-way communication with two goals in mind: (1) to identify and
UNAIDS / WHO guidance document
understand community concerns and needs, as well as their knowledge and experience, and (2) to clearly describe the research being proposed, related benefits and risks, and other practical implications.
Participation of the community in the planning and implementation of a biomedical HIV prevention product development strategy can provide at least these favourable consequences:
information regarding the health beliefs and understanding of the
information regarding the cultural norms and practices of the
input into the design of the protocol input into the design of an effective recruitment and informed
insight into the design of risk reduction interventions effective methods for disseminating information about the trial
information to the community-at-large on the proposed research trust between the community and researchers equity in eligibility criteria for participation equity in decisions regarding level of care and treatment and its
equity in plans for releasing results and distributing safe and effi-
cacious HIV prevention products.
Researchers may lack the requisite language, communication skills, and experience to respond to community concerns, while communi-ties may be unfamiliar with research concepts, such as "double blind" and "cause and effect", and may not define HIV prevention research as a priority. This underscores the need for "joint literacy", whereby researchers and community groups become sufficiently fluent in the requisite concepts and language to work productively together. Research literacy programs that include ethics training for study staff can facilitate and enhance cooperation with civil society groups.

Ethical considerations in biomedical HIV prevention trials
Guidance Point 3:
Capacity Building
Development partners and relevant international organisations should collaborate with and support countries in strategies to enhance capacity so that countries and communities in which trials are being considered can practice meaningful self-determination in decisions about the scientific and ethical conduct of biomedical HIV prevention trials and can function as equal partners with trial sponsors, local and external researchers, and others in a collaborative process.
Countries and communities who choose to participate in biomedical HIV prevention trials have the right, and the responsibility, to make decisions regarding the nature of their participation. Yet disparities in economic wealth, scientific experience, and technical capacity among countries and communities have raised concern about possible exploitation of participant countries and communities. The develop-ment and testing of biomedical HIV preventive interventions requires international cooperative research, which should transcend, in an ethical manner, such disparities. Real or perceived disparities should be resolved in a way that ensures equality in decision-making and action. The desired relationship is one of equals, whose common aim is to develop a long-term partnership through South-South as well as North-South collaboration that sustains site research capacity.
Factors that affect perceptions of disparity in power between sponsors and the countries and communities in which research takes place may include, but are not limited to, the following:
level of the proposed community's economic capacity and social
community/cultural experience with and/or understanding of
scientific research and of their responsibilities;
UNAIDS / WHO guidance document
research staff experience with and/or understanding of the
local political awareness of the importance and process of biomed-
ical HIV prevention trials;
local infrastructure, personnel, and technical capacity for providing
comprehensive HIV health care and treatment options;
ability of individuals in the community to freely provide informed
consent, in light of cultural norms, socio-economic status, gender,
and other social factors (see Guidance Points 16 and 17);
level of experience and capacity for conducting ethical and scien-
tific review (see Guidance Point 4); and
local infrastructure, personnel, and laboratory and technical
capacity for conducting the proposed research.
Strategies to overcome these disparities and empower communities
characterisation of the local epidemic through prevalence/
incidence studies and behavioural assessments
scientific exchange, and knowledge and skills transfer, between
sponsors, researchers, communities and their counterparts, and
the countries in which the research takes place, including in the
field of social science;
capacity-building programmes in the science and ethics of
biomedical HIV prevention research by relevant scientific insti-
tutions and local and international organisations;
support to develop national and local ethical review capacity
(see Guidance Point 4);
support to communities from which participants are drawn
regarding information, education, and consensus-building in
biomedical HIV prevention trials;
early involvement of communities in the design and implementa-
tion of HIV prevention product development plans and protocols
(see Guidance Point 2); and
development of laboratory capacity that can support health care
provision as well as research.
In the coming years, there will be increasing demands on clinical sites so that national governments, sponsors, and researchers should think

Ethical considerations in biomedical HIV prevention trials
about how to sustain site capacity and retain research staff expertise. Site development may build capacity for a specific trial or enhance the ability of a site to compete more broadly for a range of trials. Given the long time frames of biomedical HIV prevention research, special attention to communication and transparency is needed in order to build and maintain trust with participating communities, and to sustain site capacity even after the end of a trial.
Guidance Point 4:
Scientific and Ethical Review
Researchers and trial sponsors should carry out biomedical HIV prevention trials only in countries and communities that have appropriate capacity to conduct independent and competent scientific and ethical review.
Proposed biomedical HIV prevention trial protocols should be reviewed by scientific and ethical review committees that are located in, and include membership from, the country in which researchers wish to operate. Trials should register with an international trial registry prior to committee review as a condition of approval. Community repre-sentatives should also be involved in review of the trial protocol to insure that the research is informed by the concerns and priorities of the community in which the study is to take place. This process ensures that the proposed research is analysed in scientific and ethical terms by individuals who are familiar with the conditions prevailing in the potential research population. Reviewers should not allow research to begin unless the potential benefits of the experimental intervention outweigh the risks to participating individuals and groups. Independent ethical review of research protocols ensures public accountability and also minimizes concerns with regard to researchers' conflicts of interest because of relationships with the sponsors or pressures from those promoting the research. The scientific and ethical review should involve individuals with training in science, statistics, ethics, and law.
UNAIDS / WHO guidance document
Some countries do not currently have the capacity to conduct inde-pendent, competent, and meaningful scientific and ethical review. If the country's capacity for scientific and ethical review is judged to be inadequate, the sponsor should be responsible for ensuring that adequate structures for scientific and ethical review prior to the start of the research are developed in the country in which the trial will take place — or the research should not take place. Care should be taken to minimise the potential for conflicts of interest, while providing assistance in capacity-building for scientific and ethical review. Capacity-building in scientific and ethical review may also be developed in collaboration with international agencies, organisations within the host country, and other relevant parties.
Scientific and ethical review prior to approval of a trial protocol should take into consideration these issues:
the value and validity of the research protocol community participation and involvement risk-benefit ratio recruitment strategies and methods inclusion and exclusion criteria and screening of participants informed consent procedures and written information sheets provision of support, care, and treatment to participants, and in
respect for potential recruits and enrolled trial participants and
protection of participants' rights
confidentiality, privacy, and data protection measures prevention of stigma and discrimination sensitivity to gender procedures for monitoring enrolled participants quality assurance and safety control plans for post-trial distribution and benefit sharing.

Ethical considerations in biomedical HIV prevention trials
Guidance Point 5:
Clinical Trial Phases
As phases I, II, and III in the clinical development of a biomedical HIV preventive intervention al have their own particular scientific requirements and specific ethical chal enges, researchers and trial sponsors should justify in advance the choice of study populations for each trial phase, in scientific and ethical terms in al cases, regardless of where the study population is found. General y, early clinical phases of biomedical HIV prevention research should be conducted in communities that are less vulnerable to harm or exploitation, usual y within the sponsor country. However, countries may choose, for valid scientific and public health reasons, to conduct any trial phase within their populations, if they are able to ensure sufficient scientific infrastructure and sufficient ethical safeguards.
The initial pre-clinical phase in the development of a biomedical HIV prevention product entails research in laboratories and among animals. The transition to a phase I clinical trial in which testing involves the administration of the product to human subjects to assess safety, and in the case of vaccines to assess immunogenicity, is a time when risks may not yet be well-defined. Hence, specific infrastructures are often required in order to ensure the safety and care of the research participants at these stages. For these reasons, the first administration of a candidate biomedical HIV prevention product in humans should generally be conducted in populations which are not at risk of HIV acquisition, usually in the country of the trial sponsor.
Clinical trial researchers have been designing trials that fall somewhere between phase II (expanded safety and immunogenicity) and phase III (large scale trials to assess efficacy) – called phase IIB trials, or proof of concept trials. Phase IIB trials may provide an indication of
UNAIDS / WHO guidance document
an experimental candidate's efficacy but are less costly in terms of money, time, and number of trial participants. However, such phase IIB trials are not designed to provide enough information for regula-tory approval at the end of the trial for an HIV prevention product subject to regulation; instead, these trials test the general concept of the candidate product and efficiently filter out products that lack efficacy. Eventually, a phase III trial would have to be conducted to develop a useable and licensable HIV product.
There may be situations where low- and middle-income countries choose to conduct phases I/II and/or IIB and III among their populations that are relatively vulnerable to risk and exploitation. For instance, this could occur where an experimental HIV vaccine is directed primarily toward a viral strain that does not exist in the trial sponsor's country but does exist in the country in which it is proposed the trial be conducted. Conducting phase I/II trials in the country where the strain exists may be the only way to determine whether safety and immunogenicity are acceptable in that particular population, prior to conducting a phase III trial. Another example might be a country that decides that, due to the high level of HIV risk to its population and the gravity of HIV prevalence in the country, it is willing to test a biomedical HIV prevention product concept that has not or is not being tested in another country. Such a decision may result in obvious benefits to the country in question if an effective product is eventually found. If phase I or phase II trials are conducted in the country intending to participate in an eventual phase III trial, if phases I and II are satisfactory, this may assist in building capacity for phase III trial conduct, including increasing levels of research literacy in the population.
Establishing a biomedical HIV prevention product development programme that entails the conduct of some, most, or all of its clinical trial components in a country or community that is rela-tively vulnerable to harm or exploitation is ethically justified if:
Ethical considerations in biomedical HIV prevention trials
the product is a vaccine anticipated to be effective against a
strain of HIV that is an important public health problem in the country;
the country and the community either have, or with assistance
can develop or be provided with, adequate scientific and ethical capability and administrative and health infrastructure for the successful conduct of the proposed research;
community members, policy makers, ethicists, and investiga-
tors in the country have determined that their residents will be adequately protected from harm and exploitation, and that the biomedical HIV prevention product development programme is necessary for and responsive to the health needs and priorities in their country; and
all other conditions for ethical justification as set forth in this
document are satisfied.
In cases in which it is decided to carry out phase I or phase II trials first in a country other than the trial sponsor's country, due consideration should be given to conducting them simultaneously in the country of the trial sponsor, where this is practical and ethical. Also, as a general rule, phase I/II trials that have been performed in the country of the trial sponsor should ordinarily be repeated in the community in which the phase III trials are to be conducted, although this may not be needed, particularly in situations in which a product has demonstrated unexpectedly high efficacy.
UNAIDS / WHO guidance document
Guidance Point 6:
Research Protocols and Study Populations
In order to conduct biomedical HIV prevention trials in an ethical y acceptable manner, researchers and relevant oversight entities should ensure that the research protocol is scientifical y appropriate and that the interventions used in the experimental and control arms are ethical y justifiable.
In order to be ethical, clinical trials of novel biomedical HIV preven-tion tools should be based on scientifically valid research protocols, and the scientific questions posed should be rigorously formulated in a research protocol that is capable of providing reliable responses. Valid scientific questions relevant to biomedical HIV prevention product development are those that seek:
to gain scientific information on the safety and efficacy (degree
of protection) of candidate biomedical HIV prevention products,
and, in the case of vaccine candidates, immunogenicity (ability to
induce immune responses against HIV);
to determine correlates or surrogates of safety and protection in
order to better characterise and elicit protective mechanisms;
to compare different candidate products; and
to test whether biomedical HIV prevention products effective in
one population are effective in other populations.
Furthermore, the selection of the research population should be based on the fact that its characteristics are relevant to the scientific issues raised; and the results of the research will potentially benefit the selected population. In this sense, the research protocol should:
justify the selection and size of the research population from a
scientific point of view;
Ethical considerations in biomedical HIV prevention trials
demonstrate how the candidate biomedical HIV prevention
intervention being tested is expected to be beneficial to the
population in which testing occurs;
establish safeguards for the protection of research participants
from potential harm arising from the research (see Guidance
Point 11); and
be sensitive to issues of privacy and confidentiality in recruitment
procedures (see Guidance Point 17).
Guidance Point 7:
Recruitment of Participants
In order to conduct biomedical HIV prevention trials in an ethical y acceptable manner, participation of individuals should be voluntary and the selection of participating communities and individuals must be fair and justified in terms of the scientific goals of the research.
Selection and recruitment of communities and individuals for partici-pation in a trial must be fair and should create a research climate which shows respect for all persons. This encompasses decisions about who will be included through the formulation of inclusion and exclusion criteria, and through the strategy adopted for recruiting participants. The scientific goals of the study should be the primary basis for determining the individuals who will be recruited and enrolled. Individuals should not be excluded from the opportunity to participate without a good scientific reason or a susceptibility to risk that justifies their exclusion. Social and cultural factors should be considered to determine the vulnerability within the community of individuals who are either included or excluded. In particular, gender-sensitive approaches are key when designing recruitment procedures and special attention needs to be paid to the inclusion or exclusion of pregnant women.
UNAIDS / WHO guidance document
In some situations, voluntariness of participation may be
compromised by factors such as social marginalization, political
powerlessness, and economic dependence. Voluntariness of
participation may also be compromised where there is a cultural
tradition of men holding decision making authority in marital
relationships, parental control of women, and other forms of
social subjugation and coercion (see Guidance Point 9). In some
communities, it is customary to require the authorization of a third
party, such as a community elder or head of a family, in order for
investigators to enter the community or to approach individuals.
However, the third party only gives permission to invite individuals
to participate and such authorisation or influence must not be used
as a substitute for individual informed consent. Trials should not be
conducted where truly voluntary participation and ongoing free
informed consent cannot be obtained. Authorisation by a third
party in place of individual informed consent is permissible only
in the case of some minors who have not attained the legal age of
consent to participate in a trial. In cases where it is proposed that
minors will be enrolled as research participants, specific and full
justification for their enrolment must be given, and their own assent
or consent must be obtained in light of their evolving capacities
(see Guidance Point 10).
Ethical considerations in biomedical HIV prevention trials
Guidance Point 8:
Vulnerable Populations
The research protocol should describe the social contexts of a proposed research population (country or community) that create conditions for possible exploitation or increased vulnerability among potential trial participants, as wel as the steps that wil be taken to overcome these and protect the rights, the dignity, the safety, and the welfare of the participants.
By definition, HIV prevention research must follow the epidemic. In order to test if a biomedical HIV prevention intervention works, large numbers of individuals at high risk for HIV infection must be recruited for clinical trials. Sites based in communities with mature HIV epidemics have lower incidence rates and may be most appropriate for safety studies. Sites in communities with younger epidemics may be better suited for efficacy trials. However, partici-pating communities and populations, particularly for large-scale efficacy trials, will generally be characterized by multiple vulnera-bilities. The same factors that put these individuals at higher risk for exposure to HIV also make them vulnerable to cultural exclusion, social inequality, economic exploitation, and political oppression. Examples of populations that may have an increased vulnerability include women, children and adolescents, men who have sex with men, injecting drug users, sex workers, transgender persons, indig-enous populations, the poor, the homeless, and communities from resource-poor settings in high-income and low- and middle-income countries. At the same time, it is precisely these populations who stand to benefit most from the successful development of a new biomedical HIV prevention product or method. For these reasons, it is imperative to ensure protection of the rights of participants in biomedical HIV prevention trials, and respect for their dignity, safety, and welfare.
UNAIDS / WHO guidance document
Decision-making around conducting a biomedical HIV prevention
trial needs to consider in what ways the trial might increase or decrease
vulnerabilities. On the one hand, a trial might increase a participant's
risk of exposure to stigmatisation and discrimination if it highlights a
population's increased vulnerability to HIV exposure. On the other
hand, a trial might decrease vulnerability, if it empowers the community
or provides tangible assistance to participants, for example by improving
the accessibility, affordability, and quality of appropriate healthcare
services in the community. A social and political analysis should be
carried out early on in planning the research process, to assess determi-
nants of vulnerability, such as poverty, gender, age, ethnicity, sexuality,
health, employment, education, and legal conditions in potential partic-
ipating communities. Findings from this analysis should inform the
design of research protocols, which should be sensitive to emerging
information on incidental risks of social harm throughout the course
of a trial. Research protocols might also include ongoing independent
monitoring of a trial in relation to its impact on the vulnerabilities of
communities participating in the study (see Guidance Point 17).
The particular aspects of a social context that create conditions for exploi-tation or increased vulnerability should be described in the research protocol, as should the safeguards and measures that will be taken to prevent and overcome them. In some potential research populations (countries or communities), conditions affecting potential vulnerability or exploitation may be so severe that the risk outweighs the benefit of conducting the study in that population. In such populations, biomed-ical HIV prevention trials should not be conducted.
Sensitivity to factors of potential vulnerability, including language and cultural barriers, should inform procedures for recruiting and screening potential participants, informed consent processes, and the support, care, and treatment that participants receive in relation to the trial. If a scien-tifically appropriate population is identified as vulnerable to social harm, specific safeguards should be implemented to protect individual partici-pants, such as ensuring confidentiality, the freedom to decline joining the study and the right to withdraw at any time without penalty.
Ethical considerations in biomedical HIV prevention trials
Guidance Point 9:
Women
Researchers and trial sponsors should include women in clinical trials in order to verify safety and efficacy from their standpoint, including immunogenicity in the case of vaccine trials, since women throughout the life span, including those who are sexual y active and may become pregnant, be pregnant or be breastfeeding, should be recipients of future safe and effective biomedical HIV prevention interventions. During such research, women's autonomy should be respected and they should receive adequate information to make informed choices about risks to themselves, as wel as to their foetus or breastfed infant, where applicable.
Women throughout the life span, including those who are sexually active and may become pregnant, be pregnant or be breastfeeding, should be recipients of future safe and effective biomedical HIV prevention products and therefore should be eligible for enrolment in biomedical HIV prevention trials, both as a matter of equity and because in many communities throughout the world women, particularly young women, are at higher risk of HIV exposure. Therefore, the efficacy of candidate biomedical HIV prevention products, and their immunogenicity in the case of vaccines, should be established for women. Clinical trials should also be designed with the intent of establishing the safety of candidate biomedical prevention products for the health of the woman and, where appli-cable, her foetus, breastfed infant and, in the case of vaginal or rectal microbicides, her sexual partners.
If the safety of the biomedical HIV prevention product for a pregnant women and her foetus has not been established prior to commence-ment of the trial, women who become pregnant in the course of the trial might be discontinued from using the product, which would
UNAIDS / WHO guidance document
result in loss to follow-up of the participating women. Therefore the question of whether a safety study for pregnant women should be conducted early on in the research, at the stage when a candidate has sufficient promise to advance into a Phase IIB or Phase III efficacy trial in adults or only after the trial product has been shown to be effective should be discussed and resolved on a case-by-case basis early on in the planning of the research design. In any event, researchers should monitor adverse events among pregnant women and women who become pregnant in the course of the trial, notably in the case of a miscarriage, to determine their relatedness to the biomedical HIV preventive intervention.
The most notable data gap in the evaluation of some prevention
methods, particularly in phase I and II trials, is adequate evaluation
of safety and efficacy among women. Barriers for women partici-
pating in trials include contraceptive requirements, issues related
to current or future fertility, concerns about safety for the foetus,
and fear of being labelled as being at higher risk for HIV exposure.
Also, women present issues of particular complexity with regard to
recruitment and informed consent. In some cultures, women and
girl adolescents may not be able to exercise true autonomy in light
of the influence of their parents or sexual partners (see Guidance
Point 7). In others, young people may be more informed than their
parents, and their view and their parents' or partners' views on
their participation may differ. Further, the need for HIV testing or
pregnancy testing to assess eligibility for inclusion in a trial may
raise difficult issues regarding the maintenance of appropriate confi-
dentiality. Researchers and research staff should improve recruit-
ment strategies by anticipating and finding solutions to address
and overcome these barriers (see Guidance Point 7). Appropriate
reproductive and sexual health counselling and ancillary services,
including family planning, should be provided to trial participants.
Ethical considerations in biomedical HIV prevention trials
Although the enrolment of pregnant or breastfeeding women complicates the analysis of risks and benefits, because both the woman and the foetus or infant could be benefited or harmed, such women should be viewed as autonomous decision-makers, capable of making an informed choice for themselves and for their foetus or child. In order for pregnant women to be able to make an informed choice for their foetus/breastfed infant, they should be duly informed about any potential for teratogenesis and other known or unknown risks to the foetus and/or the breastfed infant. If there are risks related to breastfeeding, women should be informed of the availability of nutritional substitutes and other supportive services. Researchers should observe and study the positive and adverse effects on the children of these women. They should maintain pregnancy registries to collect data on outcomes of pregnancies that inadvertently occur during the trial, follow-up babies born to women participants, and take due measures for protection of privacy and personal data. In the particular case of trials of prevention of mother-to-child transmis-sion, both women and their infants who became infected should also be assessed for the development of antiretroviral resistance and its potential for effects on subsequent therapeutic options.
UNAIDS / WHO guidance document
Guidance Point 10:
Children and Adolescents
Children and adolescents should be included in clinical trials in order to verify safety and efficacy from their standpoint, in addition to immunogenicity in the case of vaccines, since they should be recipients of future biomedical HIV preventive interventions. Researchers, trial sponsors, and countries should make efforts to design and implement biomedical HIV prevention product development programmes that address the particular safety, ethical, and legal considerations relevant for children and adolescents, and safeguard their rights and welfare during participation.
Children3, including infants and adolescents, should be eligible for enrolment in biomedical HIV preventive intervention trials, both as a matter of equity and because in many communities throughout the world children are at a higher risk of HIV exposure. Infants born to HIV-infected mothers are at risk of becoming infected during birth and during the postpartum period through breastfeeding. Many adolescents are also at higher risk of HIV infection due to sexual activity, lack of access to HIV prevention education and means, and through injecting drugs with non-sterile equipment.
Therefore, biomedical HIV prevention product development programmes should consider the needs of children for a safe and effective preventive intervention; should research the legal, ethical, and health considerations relevant to their participation in biomedical trials; and should enrol children in clinical trials designed to establish safety and efficacy for their age groups, including establishing immunogenicity in the case of vaccines, if their health needs and the ethical considerations relevant to their
3 As defined by the Convention on the Rights of the Child, Article 1: "… a child means
every human being below the age of eighteen years unless, under the law applicable to the child, majority is attained earlier."
Ethical considerations in biomedical HIV prevention trials
situation can be met. Those designing biomedical HIV prevention product development programmes that might include children should do so in consultation with groups dedicated to the protec-tion and promotion of the rights and welfare of children, both at international and national levels.
It is generally understood that adolescents, prior to initiation of
sexual activity and exposure to any risk of HIV infection, will be
the primary target for any public health intervention involving
a successful biomedical intervention. In the case of HIV vaccine
candidates and other products requiring licensure that would have
an indication for use in both adolescents and adults, it is impera-
tive that there be no delays in achieving simultaneous licensure/
registration for both populations. It is therefore recommended in
such cases, that adolescents be included in trials as soon as possible
when a candidate has sufficient promise to advance into a Phase
IIB or Phase III efficacy trial in adults (see Guidance Point 5).
The use of bridging studies designed for safety (and, in the case of
an HIV vaccine, immunogenicity testing), but not including HIV
infection as a primary endpoint could be considered as an alterna-
tive for younger adolescents, to be carried out in parallel to Phase
III trials in adults.
There may be legal barriers to enrolment of younger adolescents into a clinical trial in which sexual activity is directly linked to achieving primary endpoints. It is imperative that trials are conducted in compliance with the protective laws and regulations applicable at the trial sites, including those related to legal age of consent, the age of majority, the legal age for consensual sex, legal obligations to report abuse or neglect, and other aspects which may have an impact on the conduct of biomedical HIV preventive intervention trials. Thus, undertaking a survey of applicable local laws is an essential requirement to ensure required compliance prior to making plans for such trials in a particular country.
UNAIDS / WHO guidance document
As with all other trials involving children, the permission of a parent or legal guardian is required along with the assent of the child. Unless exceptions are authorised by national legislation, consent to participate in a biomedical HIV preventive intervention trial must be secured from the parent or guardian of a child who is a minor, before the enrolment of the child as a participant in a vaccine trial. The consent of one parent is generally sufficient, unless national law requires the consent of both. Every effort should be made to obtain assent to participate in the trial also from the child according to the evolving capacities of the child, and his or her refusal to participate should be respected.
In some jurisdictions, individuals who are below the age of consent are authorised to receive, with their active consent and without the consent or awareness of their parents or guardians, such medical services as therapeutic abortion, contraception, treatment for illicit drug use or alcohol abuse, and treatment of sexually transmitted infections. In some of these jurisdictions, such minors are also authorised to consent to serve as participants in research in the same categories without the agreement or the awareness of their parents or guardians, provided the research presents no more than "minimal risk". However, such authorisation does not justify the enrolment of minors as participants in biomedical HIV prevention trials without the consent of their parents or guardians.
In some jurisdictions, some individuals who are below the general age of consent are regarded as "emancipated" or "mature" minors and are authorised to consent without the agreement or even the awareness of their parents or guardians. These may include those who are married, parents, pregnant or living independently. When authorised by national legislation, minors in these categories may consent to participation in biomedical HIV prevention trials without the permission of their parents or guardians.
Ethical considerations in biomedical HIV prevention trials
During the informed consent process, it is recommended that
investigators conduct the consent (parent) and assent (adolescent)
processes separately. This would ensure confidential counselling for
the adolescent and protect the adolescent's privacy (see Guidance
Point 18). It is also important to inform adolescents of all the
elements disclosed to an adult, and to determine that the adoles-
cent understands what s/he is assenting to (see Guidance Point 16).
The consent process and document should describe clearly what
information regarding the adolescent will or will not be disclosed
to the parent(s) or legal guardian, as well as what medical or other
services will be provided to the adolescent, as needed, without
further parental permission.
In some settings, children may have guardians who have not been legally recognized by a court as such. Adolescents who do not have parents or legally recognized guardians should not be automatically excluded from participation in a biomedical HIV preventive inter-vention trial. Participation could be considered for such adolescents who wish to participate in a trial, as long as a protective ethical oversight mechanism can be established in compliance with the local law. In addition, mechanisms should be established for an independent evaluation of the capacity of such adolescents to give informed consent.
UNAIDS / WHO guidance document
Guidance Point 11:
Potential Harms
Research protocols should specify, as fully as reasonably possible, the nature, magnitude, and probability of all potential harms resulting from participation in a biomedical HIV prevention trial, as well as the modalities by which to minimise the harms and mitigate or remedy them.
Participation in biomedical HIV prevention trials may involve physi-
ological, psychological, and social risks. Participation in a compli-
cated, lengthy trial involving intensely intimate matters, repeated HIV
testing, and exposure to culturally different scientific and medical
concepts may cause anxiety, stress, depression, as well as stress between
partners in a relationship. Legal regulations for HIV disclosure may
require partner notification when volunteers test-positive or trial
participants acquire HIV infection (see Guidance Point 18).
Participation, if it becomes publicly known, may also cause stigma and discrimination against the participant if s/he is perceived to be HIV-infected or at higher risk of acquiring HIV infection, particularly for women and adolescents, and already marginalised populations. HIV has been associated with illicit behaviour, including injecting drug use, sex work, and sexual relations between men, as well as with behaviours which may not be condoned such as premarital or extra-marital sexual activity. Discrimination can take the form of accusa-tions or abuse, can affect marriage prospects, and can result in social ostracism, job loss, denial of property or inheritance rights, or the denial of health care. Women may be at heightened risk of domestic violence as a result of trial participation. Trial sponsors, countries, and researchers should ensure that trials take place only in communities where confidentiality can be maintained and where participants will
Ethical considerations in biomedical HIV prevention trials
have access to, and can be referred to, ongoing psycho-social services, including counselling, social support groups, and legal support.
In addition to the risk of negative social impact of participation in HIV-related research, particularly for individuals and communities which are already stigmatised and marginalised, physical injuries may be sustained due to research-related activities, such as blood drawing or other medical interventions. Injections may result in pain, occa-sional skin reactions, and possibly other biological adverse events, such as fever and malaise.
In trials of microbicides, vaccines, HSV-2 suppression and antiret-roviral pre-exposure prophylaxis, there may be unknown risks to a foetus exposed to the product. In trials of prevention of mother-to-child transmission, mothers may develop antiretroviral drug resistance and may transmit resistance virus to their infants; infants may develop resistance during prophylaxis while breastfeeding.
Despite previous safety testing of microbicide products, trial partici-pants and/or sexual partners who are exposed to the product may experience adverse effects, including those which may increase risk of HIV acquisition. In the case of microbicides containing antiret-roviral drugs, there may be systemic absorption of active ingredients with possible development of antiretroviral resistance should HIV infection be acquired. In pre-exposure prophylaxis trials, individuals who acquire HIV infection may develop resistance to the antiretro-viral drug in the experimental product.
Vaccine trial participants who are exposed to HIV may have a greater risk of developing established infection, or of progressing more rapidly once infected, than if the vaccine had not been adminis-tered. If a vaccine candidate elicits a positive HIV antibody test in the absence of HIV infection, i.e. a "false positive" HIV test, negative social consequences similar to those that may exist for those actually HIV-infected may result. Informed consent procedures should
UNAIDS / WHO guidance document
include discussion of the possibility of testing HIV antibody–positive without being HIV–infected. Laboratory techniques that differen-tiate vaccine-induced antibodies and actual HIV infection should be provided at the clinical site and trial participants should be provided with necessary documentation to demonstrate that their participation in an HIV vaccine trial may be the cause of their HIV-antibody sero-positivity. Consideration should be given to appointing an ombud-sperson who can intervene on behalf of participants with outside parties, if necessary and requested.
The potential for adverse reactions to a candidate biomedical HIV prevention product, as well as possible injuries related to the conduct of biomedical HIV prevention research, should be described, as far as possible, in the research protocol and fully explained in the informed consent process. Both the protocol and the informed consent process should describe the nature of medical treatment to be provided for injuries, as well as compensation for harm incurred due to research-related activities and the process by which it will be decided whether an injury will be compensated. HIV infection acquired during partic-ipation in a biomedical HIV prevention trial should not be consid-ered a compensable injury unless directly attributable to the preven-tion product being tested itself, or to direct contamination through a research-related activity. In addition to compensation for trial-related biological/medical injuries, appropriate consideration should be given to compensation for social or economic harms.
Ethical considerations in biomedical HIV prevention trials
Guidance Point 12:
Benefits
The research protocol should provide an accurate statement of the anticipated benefit of the procedures and interventions required for the scientific conduct of the trial. In addition, the protocol should outline any services, products, and other ancil ary interventions provided in the course of the research that are likely to be beneficial to persons participating in the trials.
Clinical research inherently entails uncertainty about the degree of risk and benefits, with earlier phases of research having greater uncertainty. Proceeding to a human trial can be justified only if there is reasonable biological plausibility that a product could be safe and effective, and there is equipoise – meaning that whether a product will actually work is unknown but there is a favourable risk-benefit ratio. Only anticipated benefits of study-related procedures required for the safe and scientific conduct of the trial should be considered in the risk-benefit analysis, that is, only health care benefits derived directly from the study design. Extraneous benefits, such as payment or ancillary services, such as HIV risk-reduction interventions or reproductive health care services, should not be considered in the risk-benefit analysis. Scientific and ethical review committees must be satisfied that the potential risks to individual subjects are minimized, the potential benefits to individual participants are enhanced, and the potential benefits to individual participants and the community are proportionate to or outweigh the risks.
There should be an ongoing iterative consultative process to facili-tate local or national decision-making about the appropriate level of support, care, and treatment provided to potential and enrolled partic-ipants. Some of the activities related to the conduct of HIV biomed-ical HIV prevention trials which may benefit those who participate may actually be rights. At a minimum, participants should:
UNAIDS / WHO guidance document
have regular and supportive contact with health care workers and
counsellors throughout the course of the trial;
receive comprehensive information regarding HIV transmission
and how it can be prevented;
receive access to HIV testing and prevention methods, including
male and female condoms, sterile injecting equipment, and sexual
and reproductive health care services; and
have access to a pre-defined care and treatment package for HIV-
related illness if they become HIV-infected while enrolled in the
trial (see Guidance Point 14).
Participants should also receive reimbursement for travel and other expenses related to participation in a biomedical HIV prevention trial. In recognising the time and inconvenience their participation entails, the appropriate form and level of extraneous non-health incentives will depend on the local economic and social context.
Some have contended that to promise antiretroviral treatment to HIV prevention trial participants who become infected would constitute an undue inducement to participate in the trial. That supposition is most unlikely, since biomedical HIV prevention trials enrol healthy people, not individuals who are already sick and need treatment. If anything, the possibility of being protected from acquiring HIV by the preventive method itself could conceivably be considered an undue inducement; however, if that were the case, clinical trials of preven-tive methods could never be ethically carried out. Concerns that any form of care and treatment promised to participants in research on biomedical HIV preventive interventions could be an undue induce-ment are unwarranted.
Some may argue that provision of state-of-the-art prevention, care, and treatment services for participants introduces local inequalities and is therefore unjust when non-participants do not receive those services. However, all scale-up programmes involve temporary inequalities in the community until universal access can be attained. Achieving a perfect system of equal justice is a long-term process.
Ethical considerations in biomedical HIV prevention trials
Guidance Point 13:
Standard of Prevention
Researchers, research staff, and trial sponsors should ensure, as an integral component of the research protocol, that appropriate counsel ing and access to al state of the art HIV risk reduction methods are provided to participants throughout the duration of the biomedical HIV prevention trial. New HIV-risk-reduction methods should be added, based on consultation among al research stakeholders including the community, as they are scientifical y validated or as they are approved by relevant authorities.
The ethical principle of beneficence obligates researchers and sponsors to maximise benefits and minimise risks to participants in clinical trials. This obligation pertains not only to the preventive method being studied, but also to reducing the risk that any trial participant will acquire HIV infection during a biomedical HIV prevention trial.
Protocols for HIV prevention research obligate researchers to provide the full range of information and services for risk reduction, although they vary in defining the package of services and modes of delivery. If the study aims to test a product by comparing its additive effects to those of routinely practiced prevention, in all cases this preven-tion standard should be defined in the study protocol as well as in informed consent documents. If researchers are unable to guarantee that this standard is met, it is unethical to conduct the proposed trial.
Risk-reduction packages should include provision for family planning, pregnancy and childbirth services. Women may become pregnant during a trial. Some of these women may wish to carry the babies to term, some might have miscarriages, and some might elect to have therapeutic abortions. Researchers should guarantee that all commu-nities engaged in biomedical HIV prevention trials have state of the art reproductive health care services.
UNAIDS / WHO guidance document
Researchers should engage appropriate stakeholders in tailoring the design, implementation, and oversight of risk-reduction interven-tions addressing the specific needs and risks of trial participants in a given community. Trial sponsors, researchers, and advocates should continue efforts to resolve ongoing conflicts about legal constraints on public health practice, such as the provision of therapeutic abortion services or the provision of appropriate risk-reduction interventions for trial participants who inject drugs, including sterile injecting equipment and drug substitution treatment.
All trial participants should receive HIV risk-reduction counselling, as well as access and entitlement to proven prevention methods, and to post-exposure prophylaxis in the event of a known likely exposure. Comprehensive counselling should include the basic principles of safer sexual practice and safer injecting practices, as well as education concerning general health and treatment of sexually transmitted infections (STIs), reproductive health (contraception, pregnancy care etc.), and strategies to reduce domestic violence. Investigators should provide trial participants appropriate access to male and female condoms, sterile injecting equipment, medical substitution therapy such as methadone or buprenorphine maintenance, and treatment for other STIs. All trial participants should also be counselled at the beginning of a biomedical HIV prevention trial regarding the potential benefits and risks of post-exposure prophylaxis with antiret-roviral medication, and how it can be accessed in the community. Ways should be explored with local authorities to provide trial volun-teers and participants with information about HIV prevention and treatment services available in the community. Referral mechanisms should be established and follow-up mechanisms instituted to ensure quality case management services.
Ethical considerations in biomedical HIV prevention trials
The technique, frequency, and message content of counselling sessions should be agreed upon by the community-government-investigator-sponsor partnership, and should be based upon reliable information about the prevailing social and behavioural characteristics of the study population. The provision of HIV risk reduction counselling should be monitored to ensure quality and to minimise the potential conflict of interest between risk-reduction goals and the biomedical preven-tion trial's scientific goals. Consideration should be given to providing counselling through an agency or organisation that is independent of the investigators in order to prevent any real or perceived conflict of interest. If such an arrangement is put in place the researchers and community must ensure that the services are of a high enough standard to meet the trial's ethical obligations. Local capacity may need to be developed to provide such services in a culturally suitable and sustainable fashion, guided by the best scientific data. National and international research oversight groups should evaluate the pros and cons of independent organizations implementing risk-reduction interventions in biomedical HIV prevention trials; where such efforts are warranted and feasible, they should be undertaken and rigorously evaluated.
Mechanisms for negotiation among all research stakeholders, including the community, about the standards for enhancement of the risk-reduction package during the trial as new biomedical HIV preven-tion modalities are scientifically validated or are approved by national authorities need to be set in the study protocol. Negotiations should take into consideration feasibility, expected impact, and the ability to isolate the efficacy of the biomedical HIV modality being tested, as other prevention activities improve.
UNAIDS / WHO guidance document
Guidance Point 14:
Care and Treatment
Participants who acquire HIV infection during the conduct of a biomedical HIV prevention trial should be provided access to treatment regimens from among those international y recognised as optimal. Prior to initiation of a trial, al research stakeholders should come to agreement through participatory processes on mechanisms to provide and sustain such HIV-related care and treatment.
The obligation on the part of sponsors and investigators to ensure access to HIV care and treatment, including antiretroviral treatment, for participants who become infected derives from some or all of three ethical principles. The principle of beneficence requires that the welfare of participants be actively promoted. The principle of justice as reciprocity calls for providing something in return to participants who have volunteered their time, been inconvenienced or experi-enced discomfort by enrolling in the trial. The principle of justice, meaning treating like cases alike, requires that trial participants in high-income and low- and middle-income countries be treated equally regarding access to treatment and care.
A consensus on the level of care and treatment that should be provided to trial participants has emerged in recent years with increasing accessibility of antiretroviral treatment in low- and middle-income countries, based on strong commitments from countries, development partners and multilateral organizations; dramatic decreases in drug prices; and evidence that treatment programmes in resource-poor settings are feasible and sustainable. There is consensus that sponsors need to ensure access to internationally recognised optimal care and treatment regimens, including antiretroviral therapy, for participants who become HIV infected during the course of the trial. There is also agreement that prevention trials ought to contribute constructively to the development of HIV service provision in countries participating
Ethical considerations in biomedical HIV prevention trials
in biomedical HIV prevention research, for the sustainable provision of care and treatment after the completion of a trial.
The provision of antiretroviral treatment to trial participants who acquire HIV infection during the trial requires planning for logistics and implementation. Most such participants will not need antiretroviral treatment until years after sero-conversion. However they may benefit from a comprehensive care and prevention package including cotrimoxasole prophylaxis, isoniazid, nutritional advice, and positive prevention counselling. Biomedical HIV prevention trials should undertake to support such therapy until individuals become eligible for the national program of care and treatment in their country. Countries should include participants in biomedical HIV prevention trials in their priority list for access to antiretroviral treatment under the "Towards Universal Access" programme.
Trial sponsors and researchers should collaborate with governments in low- and middle-income countries to explore, develop, and strengthen national and local capacity to deliver the highest possible level of HIV prevention, care, and treatment services through strategic investment and development of trial-related resources. In most situations, no one stakeholder should bear the entire burden of providing resources for such services and the central responsibility for delivery should lie with local health systems.
Decisions on how these obligations are to be met are best made for
each specific trial through a transparent and participatory process that
should involve all research stakeholders before a trial starts to recruit
participants (see Guidance Point 2). This process should explore options
and determine the core obligations applicable to the given situation,
in terms of the level, scope, and duration of the care and treatment
package, equity in eligibility to access services, and responsibility for
provision and delivery. Agreements on who will finance, deliver, and
monitor care and treatment should be documented. All stakeholders
should recognize that this is a critically important and highly uncertain
UNAIDS / WHO guidance document
area that requires all partners to commit themselves to experimentation and the careful documentation of approaches, successes, and failures.
Clinical trials should be integrated into national prevention, treatment, and care plans so that services provided through clinical trials or arrangements brokered for trial participants serve to improve the health conditions of both the trial participants and the community from which they are drawn, and support and to strengthen a country's comprehensive response to the epidemic. Strengthening mechanisms to provide care, treatment, and support for people who acquire HIV infection during the course of a trial wil assist in ensuring referral and care provision for people who are deemed ineligible at recruitment to a biomedical HIV prevention trial because they already have HIV infection.
A care and treatment package should include, but not be limited to, some or all of the following items, depending on the type of research, the setting, and the consensus reached by all interested parties before the trial begins:
counselling preventive methods and means treatment for other sexually transmitted infections prevention of mother to child transmission prevention/treatment of tuberculosis prevention/treatment of opportunistic infections nutrition palliative care, including pain control and spiritual care referral to social and community support family planning reproductive health care for pregnancy and childbirth home-based care antiretroviral therapy
Ethical considerations in biomedical HIV prevention trials
Guidance Point 15:
Control Groups
Participants in both the control arm and the intervention arm should receive al established effective HIV risk reduction measures. The use of a placebo control arm is ethical y acceptable in a biomedical HIV prevention trial only when there is no HIV prevention modality of the type being studied that has been scientifical y validated in comparable populations or approved by relevant authorities.
Aside from male circumcision, a biomedical HIV prevention inter-vention with proven efficacy in preventing HIV acquisition or HIV-related disease does not currently exist. Therefore, until an effica-cious intervention is developed, the use of a placebo control arm could be ethically acceptable in appropriately designed protocols, such as three-arm trials. For example, there may be compelling scien-tific reasons which justify the use of a placebo rather than a known effective biomedical HIV intervention in the following instances:
An effective HIV vaccine exists but it is not known to be effective
against the virus that is prevalent in the research population.
The biological conditions that prevailed during the initial trial
demonstrating efficacy of a biomedical HIV prevention product
are so different from the conditions in the proposed research
population that the results of the initial trial are not generalizable
and cannot be directly applied to the research population under
A microbicide shown to be effective for vaginal intercourse may
not be effective for rectal intercourse.
Effectiveness of an intervention in one population may not be
reproduced in the context of another population if the success of
the intervention is strongly related to behaviour or behavioural
modification and conditions of product utilisation. For example,
a partially effective, coitally dependent microbicide evaluated
among women in stable partnerships may not be generalizable to
women with multiple casual partners.
UNAIDS / WHO guidance document
Guidance Point 16:
Informed Consent
Each volunteer being screened for eligibility for participation in a biomedical HIV prevention trial should provide voluntary informed consent based on complete, accurate, and appropriately conveyed and understood information before s/he is actual y enrol ed in the trial. Researchers and research staff should take efforts to ensure throughout the trial that participants continue to understand and to participate freely as the trial progresses. Informed consent, with pre- and post-test counsel ing, should also be obtained for any testing for HIV status conducted before, during, and after the trial.
Biomedical HIV prevention trials require informed consent for all
components of participation at a number of stages. The first stage
consists of screening candidates for eligibility for participation in
the trial. The screening process involves interviews on personal
matters, such as sexual behaviour and drug use, which are protected
by a right to privacy. To guarantee this right, secrecy and confi-
dentiality must be strictly observed and appropriate measures of
personal data protection should be set in place (see Guidance Point
18). The screening process also involves medical tests (such as blood
draws, pregnancy and HIV tests, vaginal examinations, and a general
physical examination), the results of which are also private and
should be kept in confidence. Informed consent should be obtained
to undergo this screening process, based on a full divulgence of all
material information regarding the screening procedures, as well as
an outline of the biomedical HIV prevention trial in which they
will be invited to enrol, if found eligible. Fully informed consent
should also be given for the test for HIV status, which should be
accompanied by pre-and post-test counselling and, if the result is
HIV positive, referral to clinical and social support services.
Ethical considerations in biomedical HIV prevention trials
The second stage at which informed consent is required occurs
once a person is judged eligible for enrolment. That individual
should then be given full information concerning the nature and
length of participation in the trial, including the risks and benefits
posed by participation, so that s/he is able to give informed consent
to participate. Time should be allowed to consider participation,
discuss with others such as partners, and ask questions. Candidates
should also be informed of their rights as participants, including
the right to confidentiality (see Guidance Point 18) and the right
to refuse to participate or to withdraw at any time from the study
without penalty.
Once enrolled, efforts should then be made throughout the trial to obtain assurance that the participation continues to be on the basis of free consent and understanding of what is happening. Informed consent, with pre- and post-test counselling, should also be given for any repeated tests for HIV status. Throughout all stages of the trial and consent process, there should be assurance by the investigator that the information is understood by the participant before consent is given. Informed consent is a process, not just a piece of paper to be read and signed. The information should be presented in appropriate forms and languages, including written information sheets. In addition, there should be oral communication of information, especially for participants who may be illiterate, and standardized tests for assessment of comprehension, where necessary.
In addition to the standard content of informed consent prior to participation in a biomedical HIV preventive intervention trial, each prospective participant must be informed, using appropriate language and technique, of the following specific details:
the reasons they have been chosen as prospective participants,
including whether they are at higher risk of HIV exposure;
that the biomedical HIV prevention product is experimental and
it is not known that it will prevent HIV infection or disease, and
UNAIDS / WHO guidance document
further, when such is the case, that some of the participants
will receive a placebo instead of the candidate HIV prevention
product through random assignment;
that they will receive counselling concerning how to reduce
their risk of HIV exposure and access to risk-reduction means
(in particular, male and female condoms, clean injecting
equipment, and where relevant, male circumcision); and that,
in spite of these risk-reduction efforts, some of the partici-
pants may become infected, particularly in the case of phase III
trials where large numbers of participants at higher risk of HIV
exposure are participating;
the specific risks for physical harm, as well as for psychological
and social harm (see Guidance Point 11), the types of treatment
and compensation that are available for harm, and the services
to which they may be referred should harm occur;
the nature and duration of care and treatment that is available,
and how it can be accessed, if they become infected with HIV
during the course of the trial (see Guidance Point 14);
the collection, use, and period of storage of biological samples
and specimens provided by participants, and the options for
their disposal at the conclusion of the trial, including the option
to refuse to allow use of such samples or specimens beyond the
scope of the specific trial in which they have participated.
the use, confidentiality, period of storage, and disposal of personal
data including genetic information, including the option to
refuse to allow use of such data beyond the scope of the specific
trial in which they participated (see Guidance Point 18).
Researchers and research staff should take special measures to protect persons who are, or may be, limited in their ability to partic-ipate voluntarily in a biomedical HIV prevention trial due to their social or legal status. The presumption is that all adults are legally competent to give informed consent to participate in a biomed-ical HIV prevention trial. However, there are several categories of
Ethical considerations in biomedical HIV prevention trials
persons who are legally competent and who have sufficient cognitive
capacity to consent, but who may have limitations in their freedom
to make independent choices (see Guidance Point 8).
The following are individuals or groups who should be given extra consideration with regard to their ability to voluntarily participate in biomedical HIV prevention trials:
persons who are junior or subordinate members of hierarchical
structures, who may be vulnerable to undue influence or
coercion and may fear retaliation if they refuse cooperation with
authorities, including members of the armed forces, students,
government employees, prisoners, and refugees;
persons who engage in illegal or socially stigmatised activities,
who are vulnerable to undue influence and threats presented by
possible breaches of confidentiality and action by law enforce-
ment authorities, including sex workers, injecting drug users,
and men who have sex with men;
persons who are impoverished or dependent on welfare
programmes, who are vulnerable to being unduly influenced by
offers of what others may consider modest material or health
Those who plan, review, and conduct biomedical HIV prevention trials should be alert to the problems presented by the involvement of such persons, and take appropriate steps to ensure meaningful and independent ongoing informed consent, and to respect their rights, foster their well being, and protect them from harm. Such steps would include community involvement in the design of recruitment and informed consent processes, along with the sensitization and training of research staff and counsellors on these issues.
UNAIDS / WHO guidance document
Guidance Point 17:
Monitoring Informed Consent and Interventions
Before a trial commences, researchers, trial sponsors, countries, and communities should agree on a plan for monitoring the initial and continuing adequacy of the informed consent process and risk-reduction interventions, including counsel ing and access to proven HIV risk-reduction methods.
Methods for monitoring the adequacy of recruitment and informed consent processes, including evaluation of participants' comprehen-sion of information, should be designed and agreed upon by the community- government-investigator-sponsor partnership. The value of informed consent depends primarily on the ongoing quality of the process by which it is conducted and not solely on the structure and content of the informed consent document. The informed consent process should be designed and monitored to empower participants to allow them to make appropriate decisions about continuing or withdrawing from the study. Special attention should be given to ensure that individuals are aware of their right to withdraw from a trial without any penalty, and that they are actually free to do so. Similarly, there are many ways in which risk-reduction interventions (coun-selling and access to means of HIV prevention) can be conducted, with some methods being more effective than others in conveying the relevant information and in reducing risk of HIV exposure for different individuals and study populations.
Monitoring should include quality assurance of gender- and culture- sensitive counsel ing services, appropriate procedures for adolescents, and evaluation of the impact of the trial on the vulnerabilities of the commu-nities involved in the study. It should also cover the welfare of partici-pants throughout the trial, including when discontinuing participation in case of adverse reactions, untoward events or changes in clinical status.
Ethical considerations in biomedical HIV prevention trials
Consideration should be given to expansion of the responsibilities of the clinical trial monitor to include adherence to the recruitment and informed consent processes and to counsel ing standards. Consideration could also be given to the appointment of an independent ombud-sperson who would handle any complaints from participants related to the conduct of the trial and suggest appropriate responses.
The appropriateness of such plans should be determined by the scien-tific and ethical review committees that are responsible for providing prior and continuing review of the trial. This recommendation supplements the usual guidelines for the monitoring of biomedical HIV prevention trials for safety and compliance with scientific and ethical standards and regulatory requirements.
Guidance Point 18 :
Confidentiality
Researchers and research staff must ensure full respect for the entitlement of potential and enrolled participants to confidentiality of information disclosed or discovered in the recruitment and informed consent processes, and during conduct of the trial. Researchers have an ongoing obligation to participants to develop and implement procedures to maintain the confidentiality and security of information collected.
A lot of information about a volunteer or a study participant is collected as part of participation in HIV vaccine and prevention research. Very personal information, like sexual behaviour, drug use, HIV status, medical conditions or even association with the trial could be highly stigmatizing and might be socially harmful if other people wrongly discover it. It is therefore of particular importance in biomedical HIV prevention trials that researchers and research staff commit to keeping confidential all personal information of all
UNAIDS / WHO guidance document
potential and enrolled participants so as to minimise the likelihood of such harm, and that they explain to volunteers and participants what measures they will be taking to protect privacy and personal informa-tion, and what limitations may exist on their ability to do so.
All participants are entitled to confidentiality of information disclosed
or discovered in the recruitment and informed consent processes, and
during conduct of the trial. Community involvement should not
compromise the confidentiality of study participants. This is of partic-
ular importance with respect to participants from vulnerable popu-
lations, women and adolescents, who may be socially susceptible to
stigma and discrimination (see Guidance Points 8, 9, 10). There may
be specific exceptions to the duty of confidentiality for legal or ethical
reasons, but those exceptions should be prospectively identified and
disclosed to the participant during the informed consent process.
Legal exceptions to the duty to maintain confidentiality might exist, for example, where disclosure is mandated by a court order or where there is a duty to report to public health authorities. In the case of children and adolescents, reporting of abuse and neglect might be required under child protection laws. Similarly, the reporting of domestic violence might be a legal duty. Trial staff should be trained to identify instances where there is such a mandatory reporting duty.
Breach of confidentiality might also be warranted on ethical grounds, so as to notify sexual partners. For example, where women participate in microbicide trials, there may be unknown risks of harm to male partners. The sponsor and researcher should have a mechanism for them to come forward to report possible negative consequences and make sure that they are notified of such, preferably by the female participants. Likewise, when participants become HIV positive, sexual partners at ongoing risk should be notified for referral to testing programmes and treatment facilities. However, researchers and research staff should be sensitive to the possibility of domestic violence as a result of partner notification.
Researchers have an ongoing obligation to participants and the host community to develop and implement procedures to protect
Ethical considerations in biomedical HIV prevention trials
the privacy of participants and to maintain the confidentiality of information collected. Such procedures might include interviewing participants outside, where they cannot be overheard, or permitting participants to not receive HIV test results. Both health care workers and research staff may need explicit training on how to maintain confidentiality. To protect confidentiality, workers in the clinic or programme setting where recruitment is taking place should first ask potential volunteers whether they would be willing to speak to a researcher who will provide information about trial participation. In the case of adolescents being recruited for endpoint efficacy trials, researchers should inquire whether their parents are aware of their sexual behaviour and explain that parental permission will be required for enrolment. In the case of media interest in the trial, research staff members should also advise participants of possible negative impact that may result from public exposure. Community advisory boards may need training to enable members to interview about the trial in ways that do not compromise the duty of confidentiality owed to individual participants or jeopardise their right to privacy.
Research may involve collecting and storing private and sensitive
data relating to individuals and communities including data derived
from biological samples (see Guidance Point 16). Measures of data
protection are of major importance in large-scale studies such as HIV
prevention trials which establish large databases to integrate clinical
data and monitor public health effect. Decisions regarding which
personal data are to be collected and stored must be based on the
requirements of the trial design and the medical needs of participants.
Personal identifiable data should be collected only by people who
have signed a confidentiality agreement. The collection of personal
identifiable data should be kept at a minimum and such data should
not be stored longer than necessary. Procedures should be in place
to monitor the use of the system where the data are stored in order
to detect potential or actual security threats. Systematic guidance on
security of data can be found in the UNAIDS Interim Guidelines on
Protecting the Confidentiality and Security of HIV Information (2007).
UNAIDS / WHO guidance document
Guidance Point 19:
Availability of Outcomes
Researchers should inform trial participants and their communities of the trial results. During the initial stages of development of a biomedical HIV prevention trial, trial sponsors and countries should agree on responsibilities and plans to make available as soon as possible any biomedical HIV preventive intervention demonstrated to be safe and effective, along with other knowledge and benefits helping to strengthen HIV prevention, to al participants in the trials in which it was tested, as wel as to other populations at higher risk of HIV exposure in the country.
To respect and recognize the contribution of trial participants and their communities to clinical research, researchers should inform them of the trial results, whether the biomedical intervention does or does not demonstrate efficacy, or the trial is stopped prematurely. Once a trial product has proven safe and effective, sponsors and researchers should work with development partners, national governments, local authori-ties, and industry where relevant, to ensure planning for its manufac-turing, regulatory approval, fair distribution, and efficient delivery in the community engaged in the trial and the country.
Given the severity of the HIV epidemic, it is imperative that suffi-cient incentives exist, both through financial rewards in the market-place and through public subsidies, to foster development of safe and effective biomedical HIV prevention products and ensure that they are produced and made readily and affordably available to the communities and countries where a product is tested, as well as to populations at higher risk of HIV exposure in other countries.
Some argue that fair benefits to the population where clinical trials are conducted need not include making successful products of the
Ethical considerations in biomedical HIV prevention trials
research available to that population. Critics contend that it is pater-
nalistic to specify the benefits, and that the country may identify other
benefits that have a higher priority. However, given the severity of the
epidemic (see Guidance Point 1) making a successful HIV biomedical
HIV prevention product or intervention reasonably available to the
population where it was tested can be sustained as a basic ethical
requirement.
Health and research communities building biomedical HIV preven-tion product development programmes should initiate before trials commence, and carry on through the course of the research, a process of discussion and negotiation about how products will be made available, along with other benefits resulting from the research, if the HIV preventive intervention is effective. This discussion should include representatives from relevant country stakeholders, such as representatives from the executive branch, health ministry, local health authorities, and relevant scientific and ethical groups, as well as from community advisory mechanisms and other key stakeholders. It should address issues such as payments, royalties, subsidies, technology and intellectual property, as well as distribution costs, channels and modalities, including delivery strategies, target populations, demand estimates, and supply chain requirements.
The discussion concerning availability and distribution of an effective biomedical HIV prevention product should further engage the national government, international organisations, development partners, representatives from wider affected communities, local authorities, international and regional non-governmental organizations, and the private sector. In addition to considering financial assistance to make biomedical HIV prevention products available, these partners should respect and help build governments and community capacity to negotiate for and implement distribution plans. Among the issues to be addressed well in advance to ensure that novel effective HIV prevention products have the greatest impact are:
UNAIDS / WHO guidance document
ongoing communication with regulatory agencies to ensure
timely licensing of proven safe and efficacious methods which
require regulatory approval;
planning for capacity building, including transfer of technology,
to mass produce an effective biomedical HIV prevention product
well in advance of product licensing, so as to minimize manufac-
preparing in advance the infrastructures needed for delivery of
new products through existing distribution systems for other
currently available HIV prevention products, such as male and
female condoms or prophylaxis for mother-to-child transmission;
instituting advance purchase commitments or other supply side
planning to deliver product for those people and populations
which it has been agreed should enjoy first the benefit of a new
proven HIV prevention intervention.
Ethical considerations in biomedical HIV prevention trials
Building col aboration to advance HIV prevention: global consultation on tenofovir pre-exposure prophy-laxis research. International AIDS Society, Bill and Melinda Gates Foundation, US National Institutes of Health, and US Centers for Disease Control and Prevention, 2005.
Building consensus on industry responsibilities related to prep research and implementation. Discussion paper. Los Angeles, ILF Stakeholder Meeting, International AIDS Society and Industry Liaison Forum, 2007.
Collins C. Gaps and inconsistencies in ethical guidance for HIV prevention research. Geneva, Joint United Nations Programme on HIV/AIDS, (UNAIDS) 2005 (http://ews.unaids.org/public/CreatingeffectivepartnershipsforHIVPrevention/Documents/).
Collins C. A new era for HIV prevention? Report of the forum for col aborative HIV research "Biomedical interventions of HIV prevention" working group Sept. 2006 meeting. Washington, DC, Forum for Collaborative HIV Research, The George Washington University, and Bill and Melinda Gates Foundation, 2007.
Emanuel EJ, Wendler D, Grady C. What makes clinical research ethical? Journal of the American Medical Association, 2000, 283:2701-2711.
Emanuel EJ, Wendler D, Killen J, Grady C. What makes clinical research in developing countries ethical? The benchmarks of ethical research. Journal of Infectious Diseases, 2004, 189:930-937.
Ethical considerations arising from biomedical HIV prevention trials in paediatric populations with high disease burden in developing countries. Accra, Ghana, World Health Organization (WHO)/Initiative for Vaccine Research ethics meeting, 2002 (www.who.int/entity/ethics/topics/vaccinetrials_pediatric_ivr_en_2002.pdf).
WHO/UNAIDS/AAVP International Expert Group, Osmanov S. Executive summary and recommendations from WHO/UNAIDS and AAVP consultation on: ‘The inclusion of adoles-cents in HIV vaccine trials', 16-18 March 2006 in Gaborone, Botswana. AIDS 2007;21:W1-10.
Finding your way: a guide to understanding ethical issues related to participation in clinical trials for preven-tive HIV vaccines. New York and Toronto, AIDS Vaccine Advocacy Coalition and International Council of AIDS Service Organizations, 2005.
Good participatory practice guidelines in biomedical HIV prevention trials. UNAIDS/AVAC. Geneva, Joint United Nations Programme on HIV/AIDS (UNAIDS) and AIDS Vaccine Advocacy Coalition, 2007.
Guenter D, Esparza J, Macklin R. Ethical considerations in international HIV vaccine trials: summary of a consultative process by the Joint United Nations Programme on HIV/AIDS (UNAIDS). Journal of Medical Ethics, 2000, 26:37-43.
Interim guidelines on protecting the confidentiality and security of HIV information: Proceedings from a Workshop 15-17 May 2006, Geneva, Switzerland. UNAIDS http://data.unaids.org/pub/manual/2007/confidentiality_security_interim_guidelines_15may2007_en.pdf
UNAIDS / WHO guidance document
Lo B, Padian N, Barnes M. The obligation to provide antiretroviral treatment in HIV preven-tion trials. AIDS, 2007, 21:1129-1231.
Mills E, Cooper C, Guyatt G, Gilchrist A, Rachlis B, Sulway C, Wilson K. Barriers to partici-pating in an HIV vaccine trial: a systematic review. AIDS, 2004, 18:2235-2242.
Male circumcision and HIV prevention: research implications for policy and programming, Montreux, 6-8 March 2007. Conclusions and Recommendations. Geneva, World Health Organization (WHO), Joint United Nations Programme on HIV/AIDS (UNAIDS), and United Nations Children's Fund (UNICEF), 2007 (http://data.unaids.org/pub/Report/2007/mc_recommendations_en.pdf).
[Anonymous]. One standard, not two. Lancet, 2003, 362:1005.
Participants' bil of rights and responsibilities. Seattle, HIV Vaccine Trials Network, 2007.
Shapiro HT, Meslin EM. Ethical issues in the design and conduct of clinical trials in devel-oping countries. New England Journal of Medicine, 2001, 345:139-142.
Slack C, Strode A, Fleischer T, Gray G, Ranchod C. Enrolling adolescents in HIV vaccine trials: reflections on legal complexities from South Africa. BioMed Central Medical Ethics, 2007, 8:5 (http://www.biomedcentral.com/1472-6939/8/5).
Strengthening the PREP stakeholder dialogue: researcher and community update. Report of a meeting convened by the International AIDS Society on behalf of the Bil & Melinda Gates Foundation. Toronto, International AIDS Society and Bill and Melinda Gates Foundation, 2006.
Tarantola D, Macklin R, Reed ZH, Kieny MP, Osmanov S, Stobie M, Hankins C. Ethical considerations related to the provision of care and treatment in vaccine trials. Vaccine, 2007, 25:4863-4874.
Toward universal access: scaling up priority HIV/AIDS interventions in the health sector. Progress report, April 2007. Geneva, World Health Organization (WHO), Joint United Nations Programme on HIV/AIDS (UNAIDS), and United Nations Children's Fund (UNICEF), 2007 (http://www.who.int/hiv/mediacentre/universal_access_progress_report_en.pdf).
UNAIDS. Creating effective partnerships for HIV prevention trials: report of a UNAIDS consultation, Geneva 20-21 June 2005. AIDS, 2006, 20:W1-W11.
WHO/UNAIDS. Treating people with intercurrent infection in HIV prevention trials: report from a WHO/UNAIDS consultation, Geneva 17-18th July 2003. AIDS, 2004, 18:W1-W12.
WHO-UNAIDS Expert Group. Gender, age, and ethnicity in HIV vaccine-related research and clinical trials: report from a WHO-UNAIDS consultation, 26-28 August 2004, Lausanne, Switzerland. AIDS, 2005, 19:W7-W28.
The Joint United Nations Programme on HIV/AIDS (UNAIDS) brings together ten UN agencies in a common effort to fight the epidemic: the Office of the United Nations High Commissioner for Refugees (UNHCR), the United Nations Children's Fund (UNICEF), the World Food Programme (WFP), the United Nations Development Programme (UNDP), the United Nations Population Fund (UNFPA), the United Nations Office on Drugs and Crime (UNODC), the International Labour Organization (ILO), the United Nations Educational, Scientific and Cultural Organization (UNESCO), the World Health Organization (WHO), and the World Bank.
UNAIDS, as a cosponsored programme, unites the responses to the epidemic of its ten cosponsoring organizations and supplements these efforts with special initiatives. Its purpose is to lead and assist an expansion of the international response to AIDS on all fronts. UNAIDS works with a broad range of partners – governmental and nongovernmental, business, scientific and lay – to share knowledge, skills and best practices across boundaries.
UNAIDS20 AVENUE APPIACH-1211 GENEVA 27SWITZERLAND
Tel: (+41) 22 791 36 66Fax: (+41) 22 791 48 35e-mail: [email protected]
Uniting the world against AIDS
Source: http://www.niph.org.kh/sph/centers_program/1224005964Ethical%20consideration%20in%20Biomedical%20HIV%20preveniton%20trials.PDF
Contents lists available at European Journal of Pharmacology Molecular and Cellular Pharmacology Synthesis and characterization of [3H]-SN56, a novel radioligand for the σ1 receptor James A. Fishback , Christophe Mesangeau , Jacques H. Poupaert Christopher R. McCurdy , Rae R. Matsumoto ,a Department of Basic Pharmaceutical Sciences, West Virginia University, Morgantown, WV 26506, USAb Department of Pharmacology, University of Mississippi, University, MS 38677, USAc Department of Medicinal Chemistry, University of Mississippi, University, MS 38677, USAd Universite Catholique de Louvain, Avenue Emmanuel Mounier 74, B-1200, Brussels, Belgium
Submission to the Inquiry into drug and alcohol treatment March 2013 Contact for this submission: Ian Jackson State Director, NSW Email P: (02) 9641 5009 Mission Australia Mission Australia is a large national not-for-profit organisation that has been transforming the lives of Australians in need for more than 150 years. Our vision is to see a fairer Australia by eliminating disadvantage for vulnerable Australians. In 2011-12 our 326 Community Services (including our Early Learning Services) assisted 110,389 individuals and 5,732 families. MA Housing also grew its housing management portfolio to 1,418 dwellings in the same year, substantially increasing the number of people we have been able to support into stable accommodation. Our Employment Solutions also offered ten programs that helped 165,000 individuals and assisted 15,850 people move into sustainable employment1. In NSW/ACT